Okay #medtwitter and #dermtwitter, you knew it was only a matter of time, didn’t you?! Let’s do this #COVID19 themed #medthread:
#COVID TOES, a #TWEETORIAL!
#MedEd #FOAMEd #dermatology #dermatologia @AADskin @AADMember @Meddermsoc @dermhospitalist
First, a word of caution – this is one person’s thoughts on a new skin finding reported in a new disease that the medical community is still learning about! As such, nothing in the #tweetorial should be regarded as definite. Just wanted to share a thought process!
So, who cares? #COVID19 is devastating, at times even for the young & healthy! But it’s all respiratory, right?
Well, as we're learning, there's so much more to #SARScov2, and as a #dermatologist, this is the perfect example of how the exam helps frame possible mechanisms.
And also, what if #covidtoes can help us with the testing and contact tracing effort?!
As @DrEstherFreeman & @lindyfox1 pointed out 👇, maybe #covidtoes are the new anosmia! Perhaps we should be testing even mild/asx patients with this finding!
Now that I've hopefully made a case for why we should care, what’s actually happening underneath the skin?
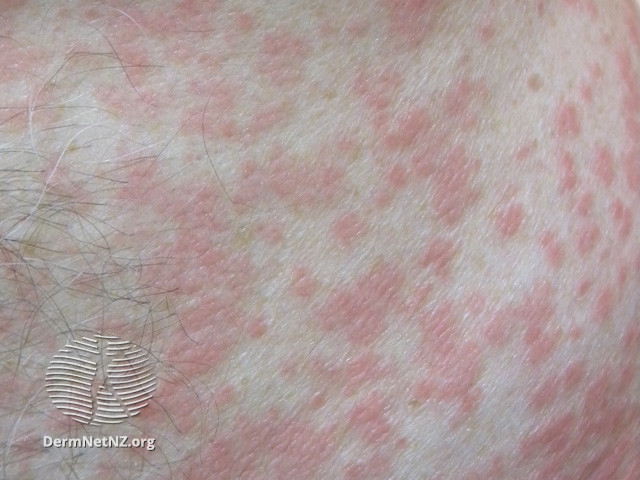
There have been multiple reports and different clinical photos of #covidtoes.👇
PC: fip-ifp.org/wp-content/upl… for pic1.
PC: today.com/health/skin-sy…


Importantly, these 2 photos make me think of 2 different processes!
The 1st photo looks like retiform purpura. This means that the purpura is stellate & makes me think that something is blocking blood flow. See my #tweetorial on purpura for details:

So hang on to your seats while I conjecture wildly:
- Are these 2 photos showing the same process?
- Could one be more thombotic & the other more inflammatory?
- Why is it only distal? Is it embolic (doubt it) or temperature related?
- Could this elucidate any vascular issues?
I would make a couple other points:
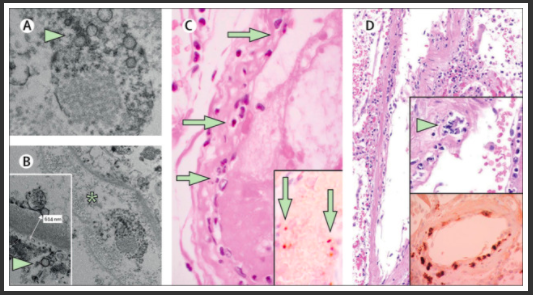
We already know that there is some thrombotic process with some cases of #COVID19. Perhaps #covidtoes are related to that. This paper found #SARS_CoV2 infected patients had viral inclusions in endothelial cells:
thelancet.com/journals/lance…
And anecdotally speaking, #covidtoes seem to affect the younger & milder COVID19 pts. What is it about this group of pts that makes it more common? Or perhaps the sicker pts get it too, but we just aren't noticing since they have bigger fish to fry.
👀yahoo.com/lifestyle/covi…
I should point out that there have been a host of other skin eruptions reported with #COVID. I think many of them are nonspecific and may just be reflections of the immune system dealing with a viral process. #Covidtoes seem to be much more specific for this.
pc: @dermnetnz

Bottom line: If I see #covidtoes & I have the capability, I'd consider a #COVID19 test for the purposes of improving our testing/tracing effort.
A quick plug for the @AADskin #COVID registry. It'd be great to gather more data so we can learn more!
aad.org/member/practic…








