Coagulopathy Strikes Back.
What happens when #COVID19 clashes with the world of hematology?
Buckle up again for a long one.
...let’s dive in like this macrophage (exploring all directions):
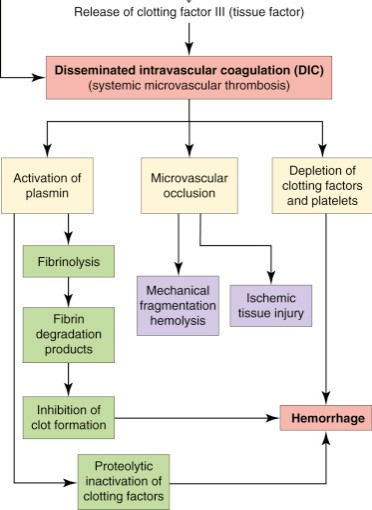
...so what have we seen pathologically in COVID19?
Cui et al (Chinese): 81 ICU pts, 25% VTE incidence without VTE ppx
Kiok et al (Dutch): 184 ICU pts, VTE in 27% despite ppx AC
Llitjos et al (French): 26 ICU pts, VTE in 69% of pts on therapeutic (56%) or prophylactic (100%) AC
With such an increased propensity for thrombosis, increased D-dimer levels have also been correlated with various risks in COVID-19:
2. Progressive⬆️over 7 days following admission is seen in non-survivors
3. >1 mg/L = HR of 18.4 for in-hospital mortality
4. 3-4x ULN D-dimer at baseline = need to admit to hospital (per ISTH guidelines)
...probably not.
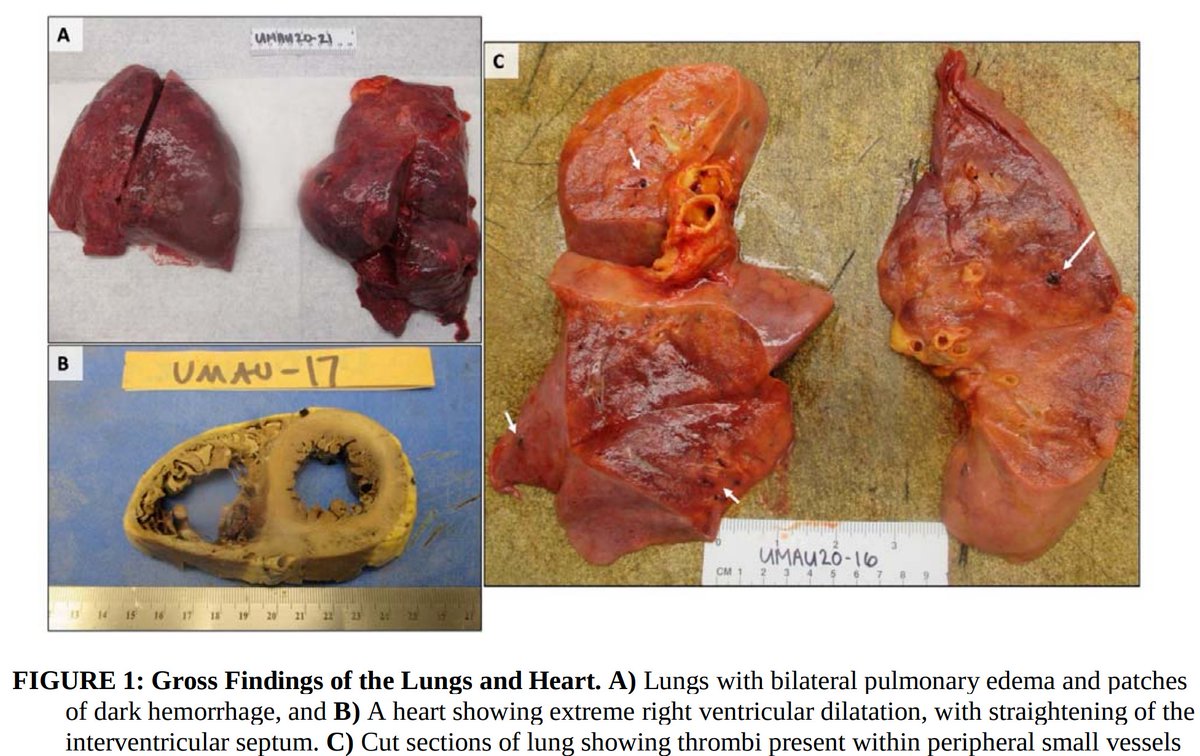
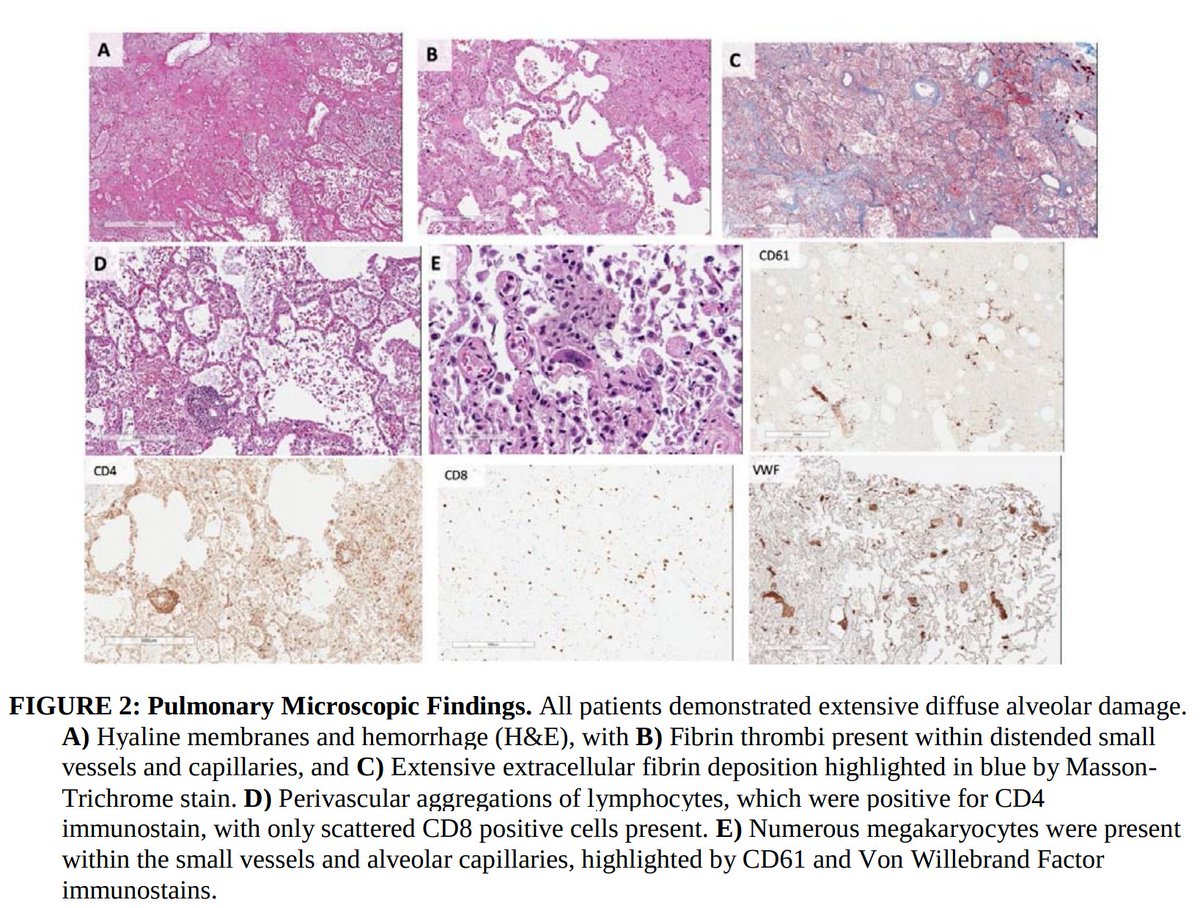
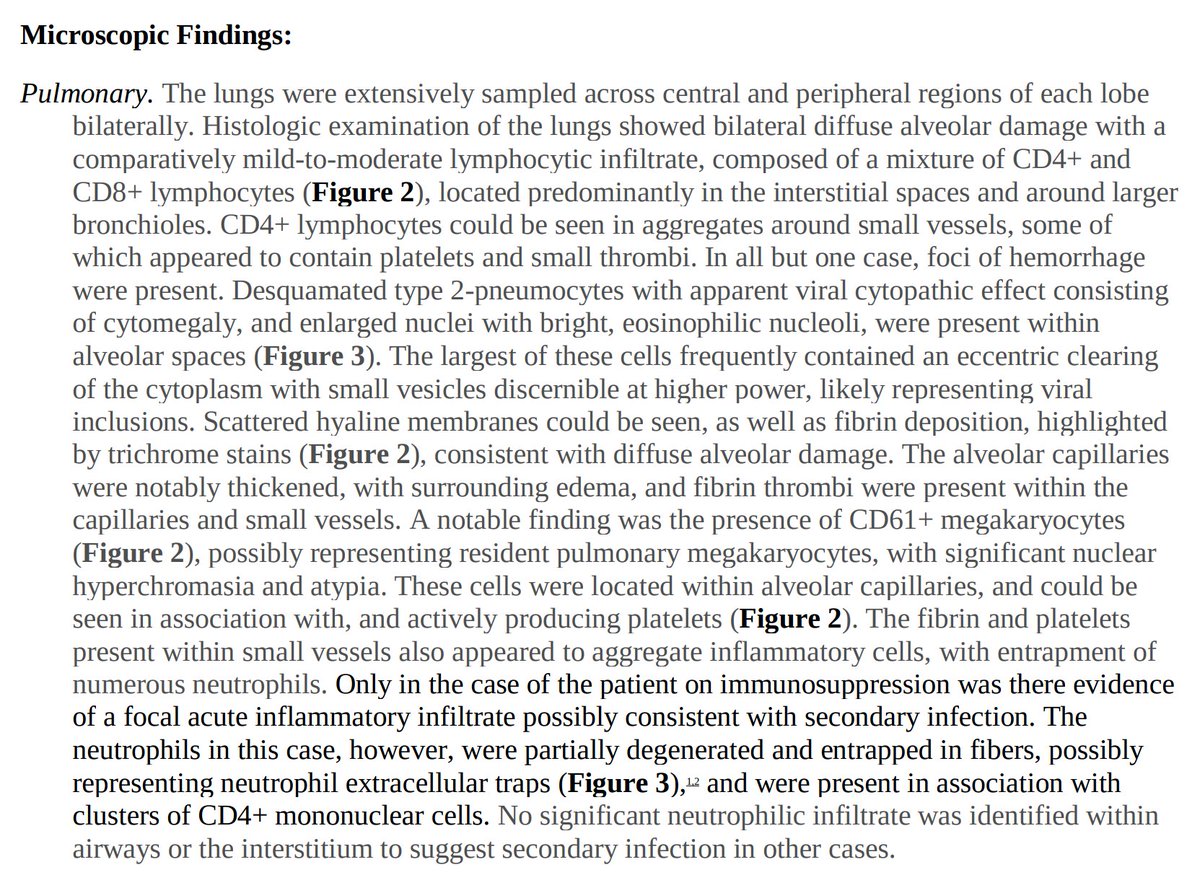
Marongiu et al suggest rather than overt DIC, a localized intravascular coagulation (LIC) first occurs in the lungs.
This moreso reflects thromboinflammation, or the complex interplay between acute inflammation & thrombosis.
First, true or false:
Thrombosis can be a protective mechanism in the setting of infection.
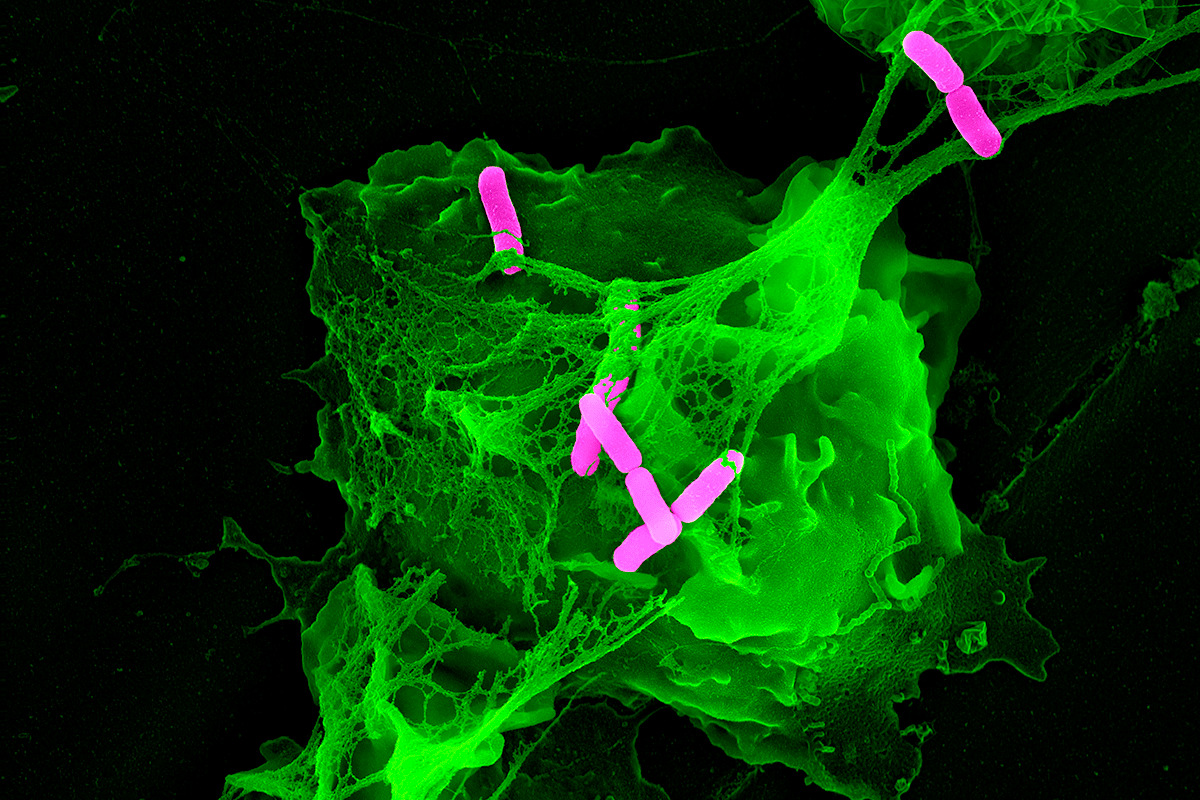
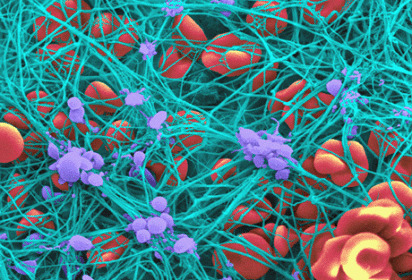
Though thrombosis is seldom discussed as an immunological phenomenon, the formation of fibrin clot can trap circulating bacteria and help in their phagocytosis, antigen presentation, and ultimately, eradication.
Think of a fish net catching salmon on a river.
Suicidal = PMN effectively kills itself by extruding it’s nuclear DNA (green material below).
Vital = only some nuclear material exocytosed from the nucleus and released. PMN can still go on with phagocytosis afterward.
How would vascular endothelial injury promote thrombosis?
TEG studies from Italy have demonstrated severe platelet hyperactivation and subsequent hypercoagulability.
Plasminogen activator-inhibitor (PAI-1) is released from damaged endothelium and leads to local hypofibrinolysis.
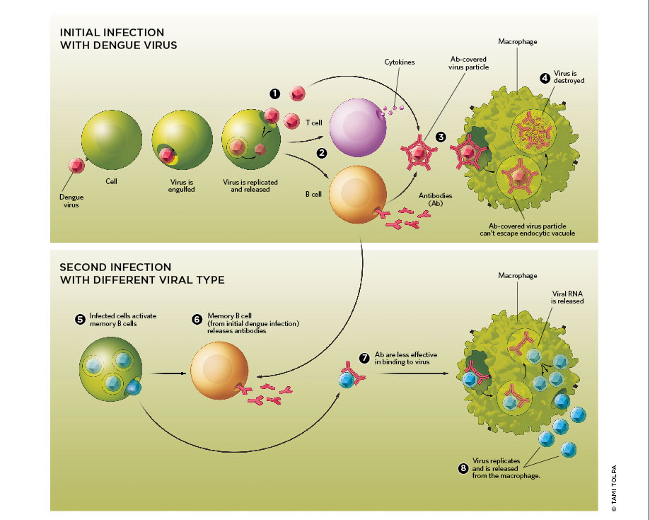
This is in stark contrast to Dengue fever, where hemorrhagic shock is the defining feature of severe disease.
...so why are they different?
1. COVID coagulopathy is multifactorial, but mainly represents thromboinflammation, not overt DIC.
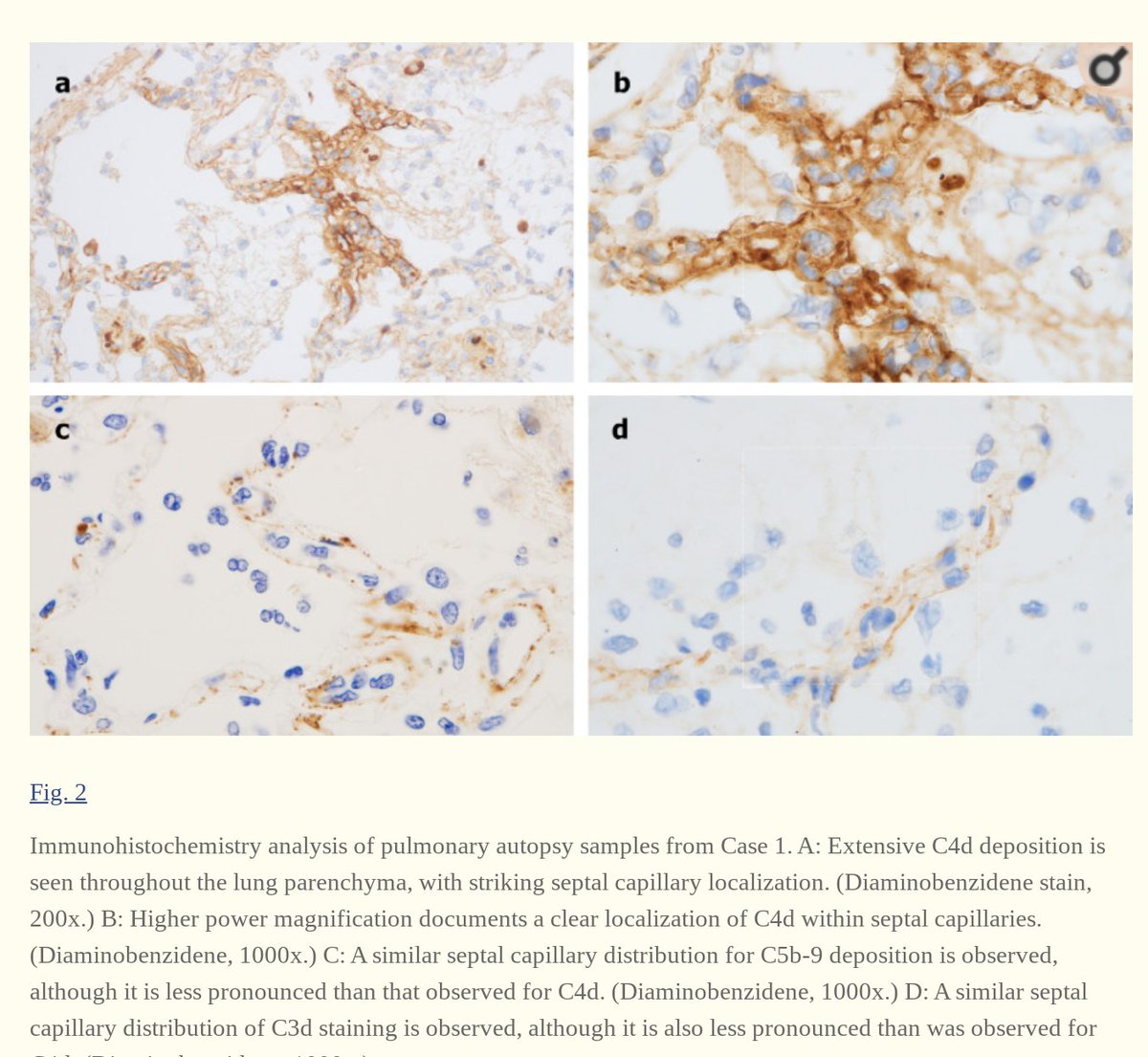
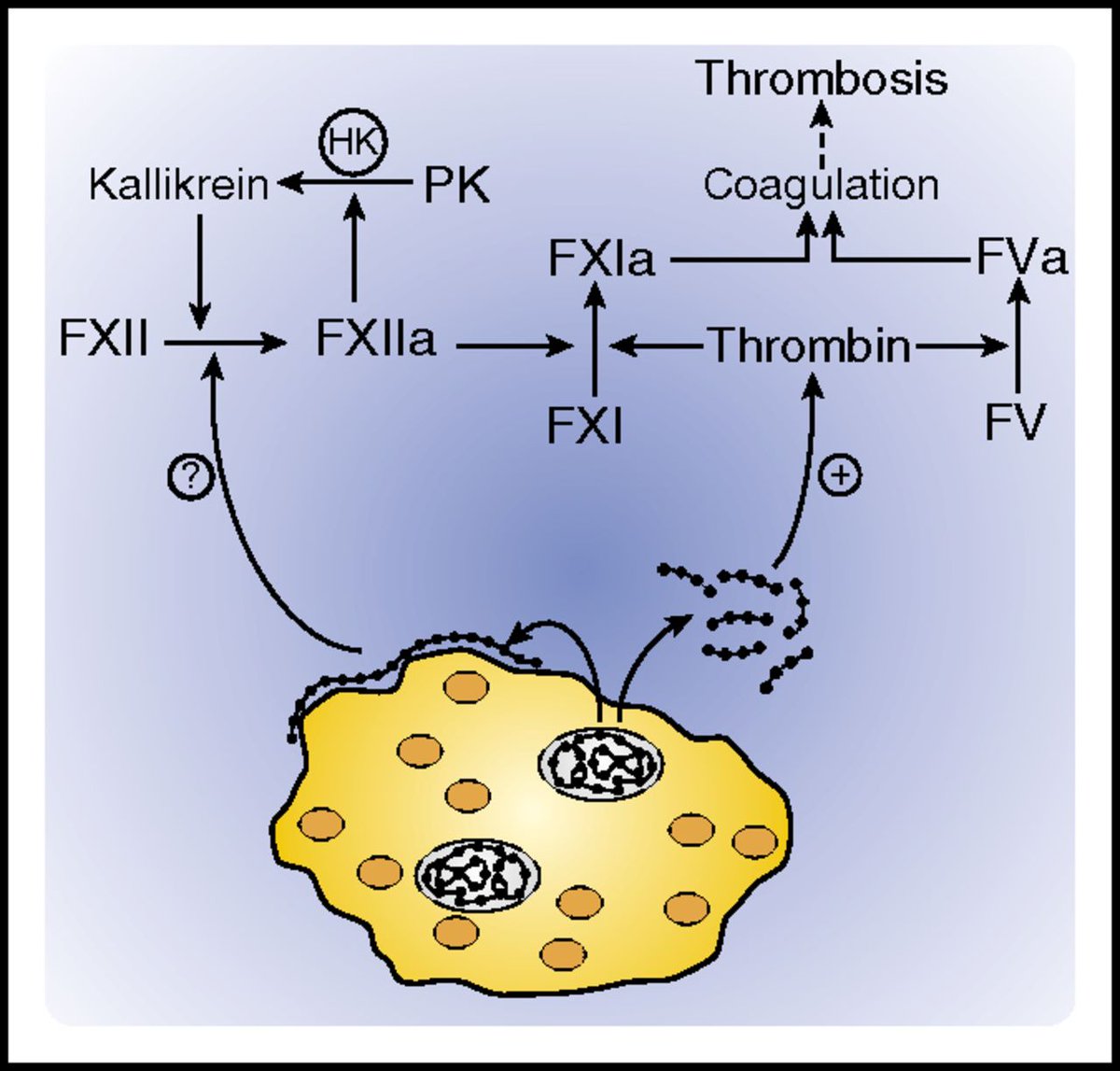
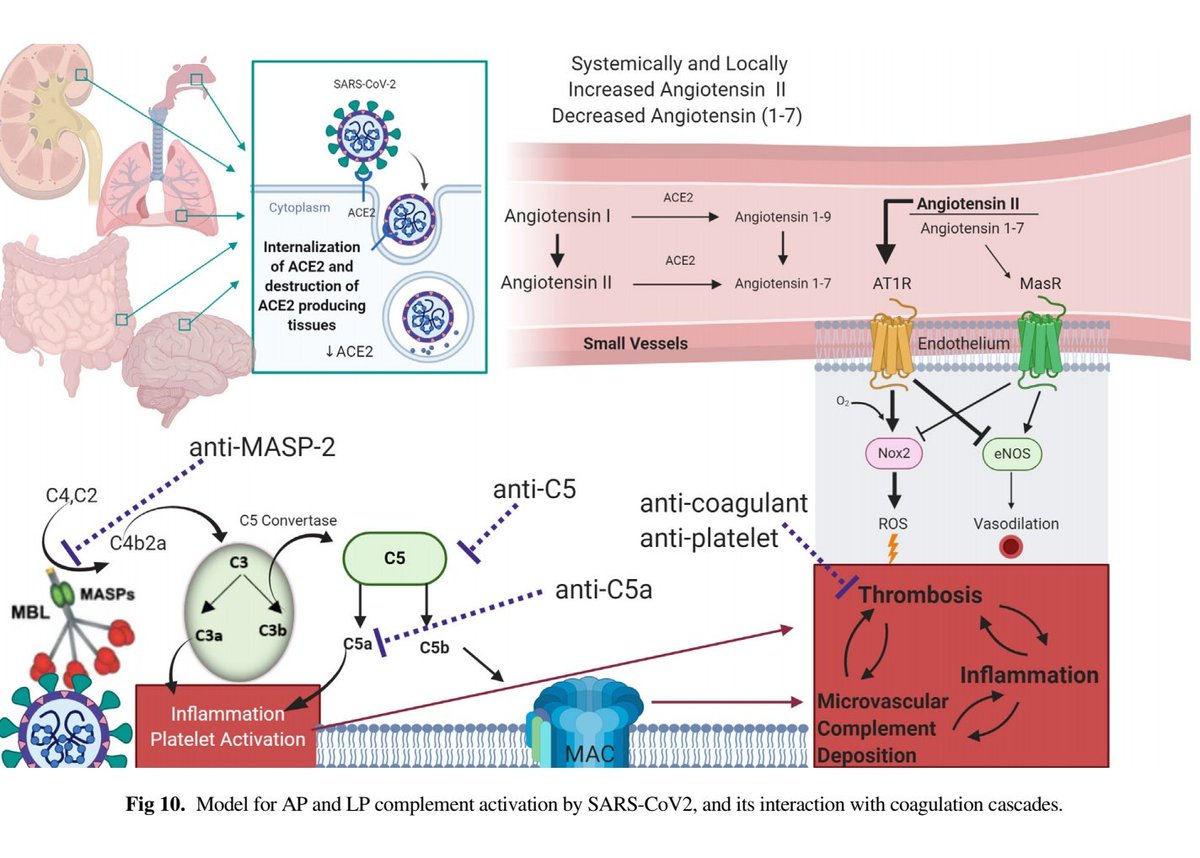
2. PMN NETs + platelet activation + direct viral endothelial invasion + complement activation = endothelial damage → ⬆️TF and PAI-1 release→ initial pulmonary LIC
4. Thromboinflammation mirrors what is seen pathologically in COVID-19, with increased PMN NETs, complement deposition, endotheliitis with capillary damage, and microvascular thrombosis
I know this is a controversial topic and I am always open to further data/suggestions.
In my last tweetorial, we will attempt to tie everything together, providing a framework to understand potential treatment options.
Amazing tweetorial from @acweyand on data surrounding this:
Best commentary on COVID-coagulopathy to date IMO:
onlinelibrary.wiley.com/doi/epdf/10.11…
Immunothrombosis:
onlinejacc.org/content/early/…
Endotheliitis:
thelancet.com/journals/lance…
medrxiv.org/content/10.110…
ncbi.nlm.nih.gov/pmc/articles/P…
medrxiv.org/content/10.110…
PMN NETs:
haematologica.org/content/haemat…
ADE SARS
sciencedirect.com/science/articl…
Polyphosphates:
ncbi.nlm.nih.gov/pubmed/22517894