More evidence of the devastating impact of @COVID19 on people’s lives. Reduction in admissions with #heartattack & early signal of higher rate of deaths. academic.oup.com/ehjqcco/articl…
Many have hypothesised that #COVID19 might have affected the care & outcomes of people with acute myocardial infarction (#heartattack). Therefore, we aimed to determine whether the #COVID19UK pandemic changed patient response, #hospital treatment & mortality from #heartattack .
We classified admissions as non ST-elevation myocardial infarction (NSTEMI) or STEMI at 99 hospitals in #England through live feeding from the Myocardial Ischaemia National Audit Project (#MINAP @CardiacAudit ) between 1st January, 2019 & 22nd May, 2020
We undertook descriptive analyses & estimated time series plots using a 7-day simple moving average, adjusted for seasonality.
From 23rd March, 2020 (UK lockdown) median daily hospitalisations decreased more for NSTEMI (69 to 35; IRR 0.51, 95% CI 0.47-0.54) than STEMI (35 to 25; IRR 0.74, 95% CI 0.69-0.80) to a nadir on 19th April, 2020.
We have reported @TheLancet similar findings, but using English administrative data from @NHSDigital thelancet.com/journals/lance…
However, arising from that analysis, we speculated that reduced number of admissions may have resulted in increases in out-of-hospital deaths & long-term complications of #heartattack & missed opportunities to offer secondary prevention treatment
In the @CardiacAudit national #cardiovascular clinical registry analysis, we found that during #lockdown, patients were younger (mean age 68.7 years vs. 66.9 years), less frequently #diabetic (24.6% vs. 28.1%) or had #cerebrovascular disease (7.0% vs. 8.6%).
Patients with STEMI more frequently received primary PCI (81.8% vs 78.8%%) & the use of thrombolysis was negligible (0.5% vs. 0.3%).
The median admission-to-coronary angiography duration for NSTEMI decreased substantially (26.2 vs. 64.0 hours).
Overall, the median duration of hospitalisation decreased (4 to 2 days).
Notably, the prescription of secondary prevention pharmacotherapies was very high & remained unchanged (each evidenced-based medication reached >94.7%).
..., but “what about deaths?”, I hear you shout...
Well, we linked our live feed national clinical registry data to the @ONS Civial Register of Deaths to estimate all-cause mortality at 30 days.
In the UK, all deaths must be certified & registered, & within a short period of time.
...”so what did it show?”...
So, we found that for patient ts admitted with STEMI their mortality at 30 days decreased from 10.2% to 7.7%; OR 0.73, 95% CI 0.54-0.97).
... “,but what about NSTEMI?”...
We found that for patients admitted with NSTEMI, their mortality at 30 days increased from 5.4% to 7.5%; OR 1.41, 95% CI 1.08-1.80).
...”why?”
Who knows? One can only speculate at this point. We have further work to do to understand this.
It’s possible that those admitted with NSTEMI were somehow different from the normal admissions with NSTEMI, perhaps they were more like to have #COVID19 infection, or there were implications of their reduced length of hospital stay, or rates or of an invasive coronary strategy?
Quotes from me:
“This national study provides evidence for the devastating impact that COVID19 has had on people’s lives”.
“This national study provides evidence for the devastating impact that COVID19 has had on people’s lives”.
“The inflation in deaths among people attending hospital with heart attack is very likely an early signal of the mortality and morbidity that is yet to be observed”.
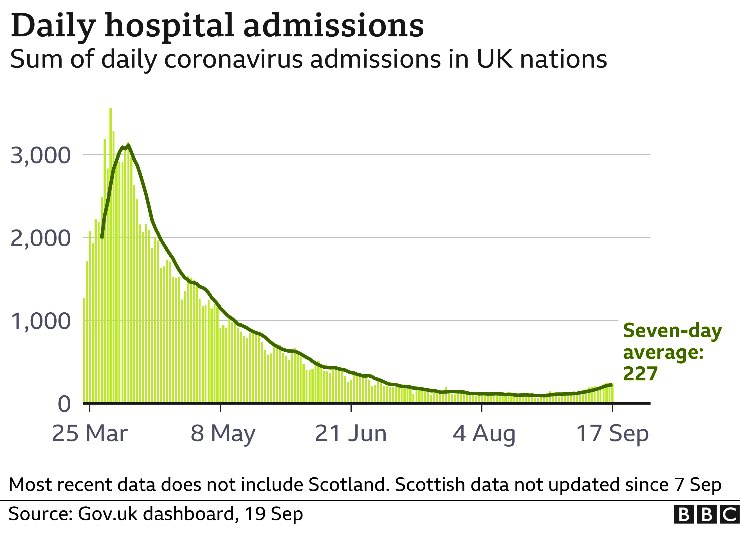
“Notably we have not seen a return to the normal rates of admissions with heart attack. This means that people may still be delaying seeking help”.@TheBHF
• • •
Missing some Tweet in this thread? You can try to
force a refresh