While we're beginning to understand more and more about the #microbiome, research on the #mycobiome (fungi 🍄) is in its infancy. Here is my summary of 🔑 points from @aeprobio's seminar on the latest research on fungi and the gut!
#GITwitter
#GITwitter
Bacteria in the #gut outnumber fungi as a class, but at the individual species level can occur in the same numbers. 

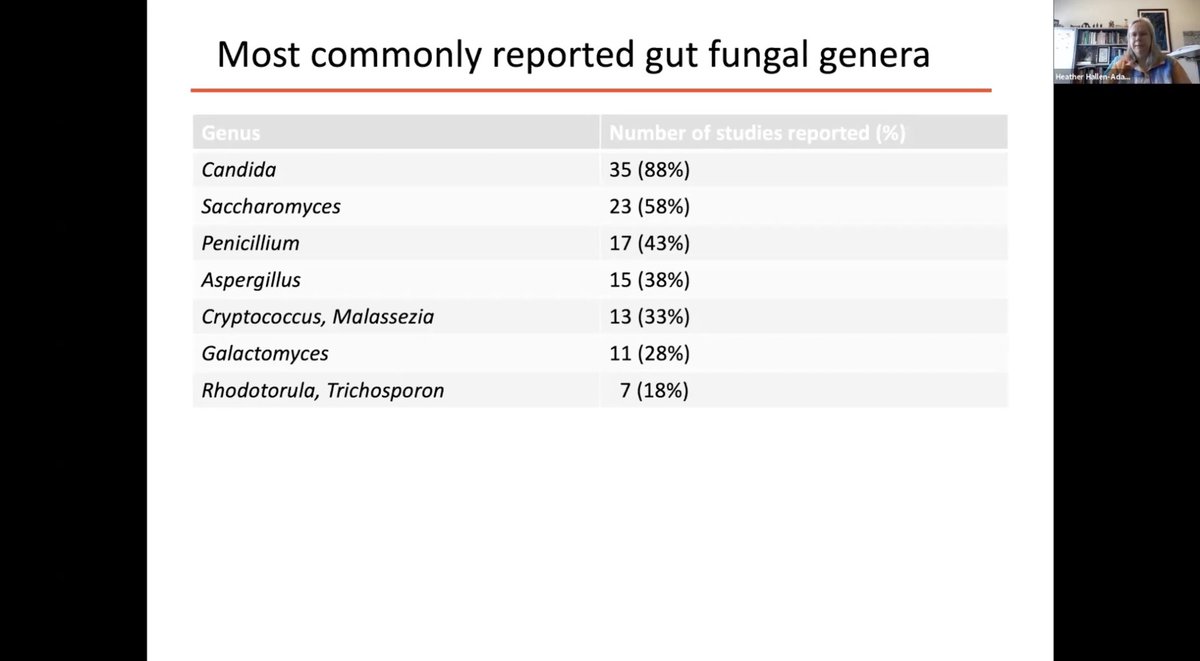
Most #gut fungi belong to Ascomycota or Basidiomycota 

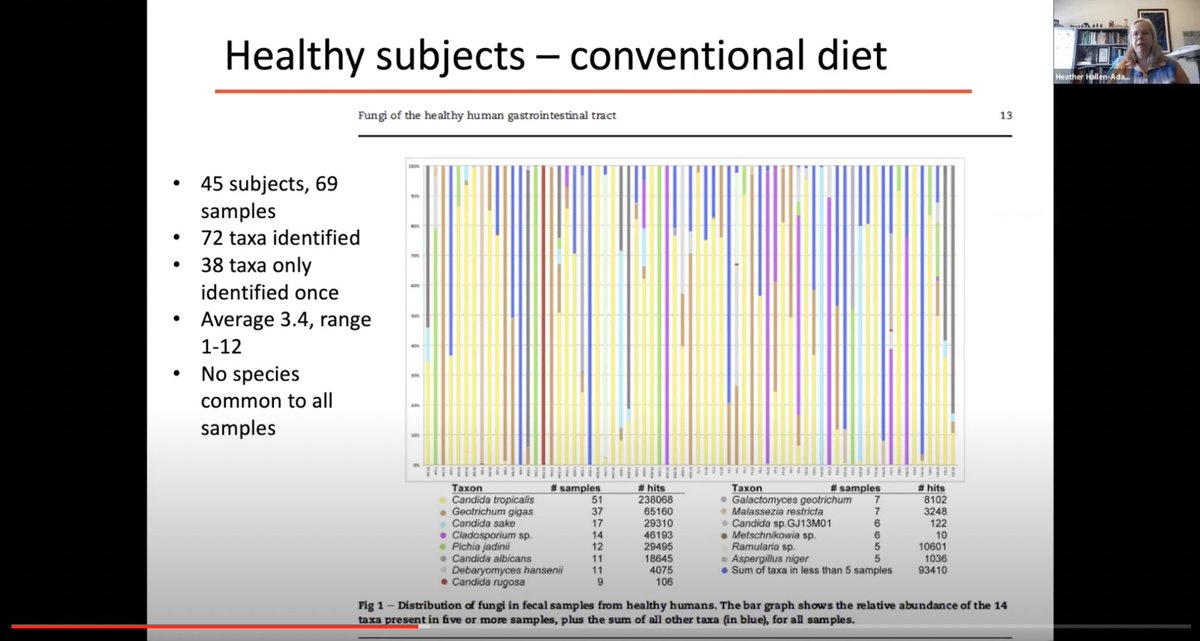
The #mycobiome has low evenness, with different individuals having dominant fungal communities 

On the other hand, fungal dysbiosis has been implicated in many disease states, including #IBD. 

The future of #mycobiome research 

Summary from @PaulineDScanlan 

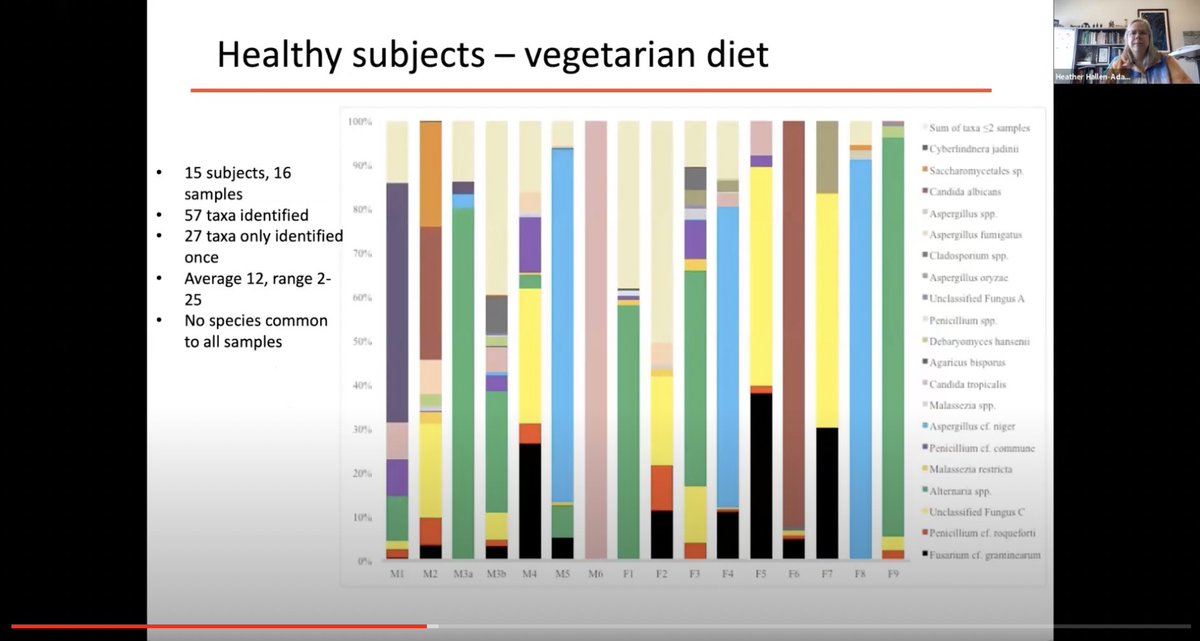
Just as #diet is an important contributor to the #gut #microbiome, diet also modulates the #mycobiome.
More frequent brushing of teeth is associated with ⬇️ gut Candida
More frequent brushing of teeth is associated with ⬇️ gut Candida

Western diet vs vegetarian diet:
Vegetarian diet has greater fungal diversity, and different composition of fungi (e.g. Candida 63% vs 84%). Fusarium and Aspergillus are common plant pathogens.


Vegetarian diet has greater fungal diversity, and different composition of fungi (e.g. Candida 63% vs 84%). Fusarium and Aspergillus are common plant pathogens.

Dietary fungi, even if not colonizing the gut, probably have a role in host health. For example, Debaromyces hansenii seem to inhibit Candida albicans and C. tropicalis 



Summary from @HallenAdams 

Fungal diversity in healthy individuals the #gut is lower than bacterial diversity. 



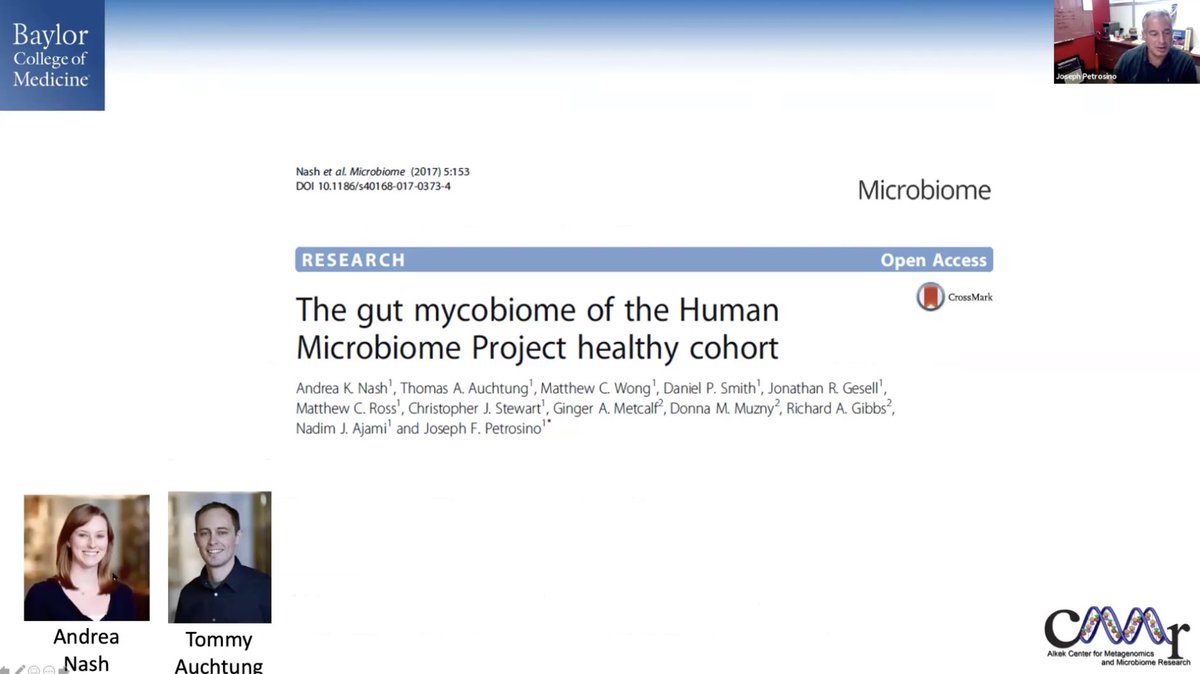



Fungi interact with #gut bacteria.
Can we use this knowledge to develop fungal-based #probiotics to support good bacteria and suppress the bad?
Can we use this knowledge to develop fungal-based #probiotics to support good bacteria and suppress the bad?

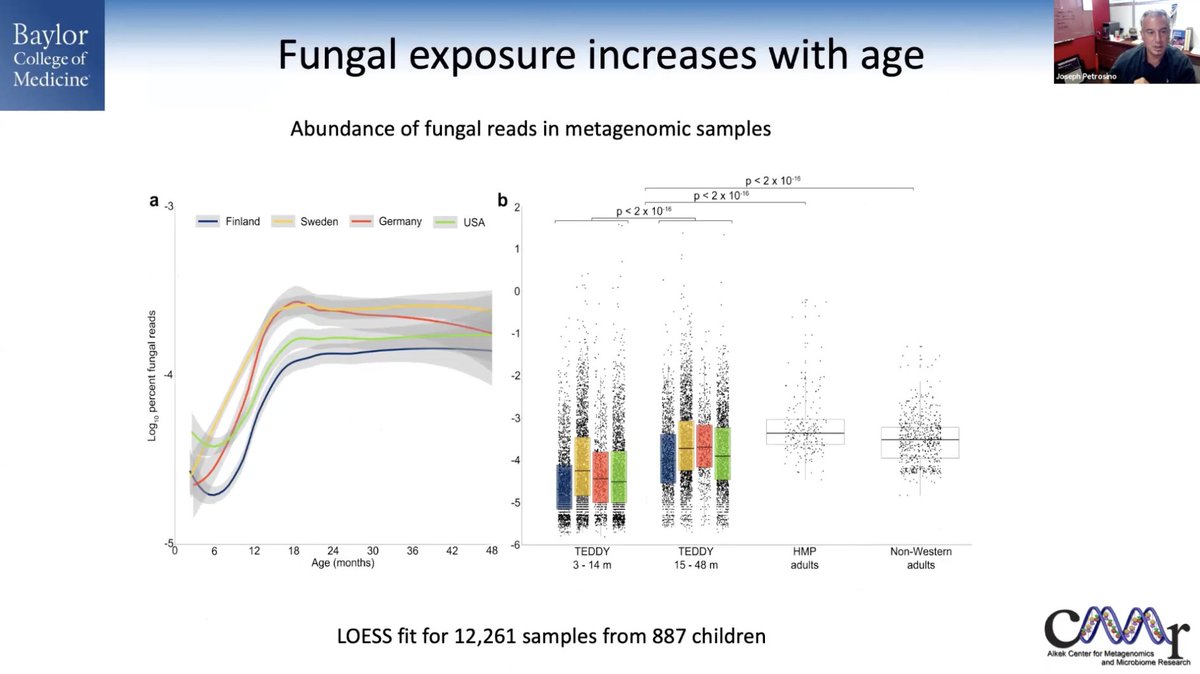
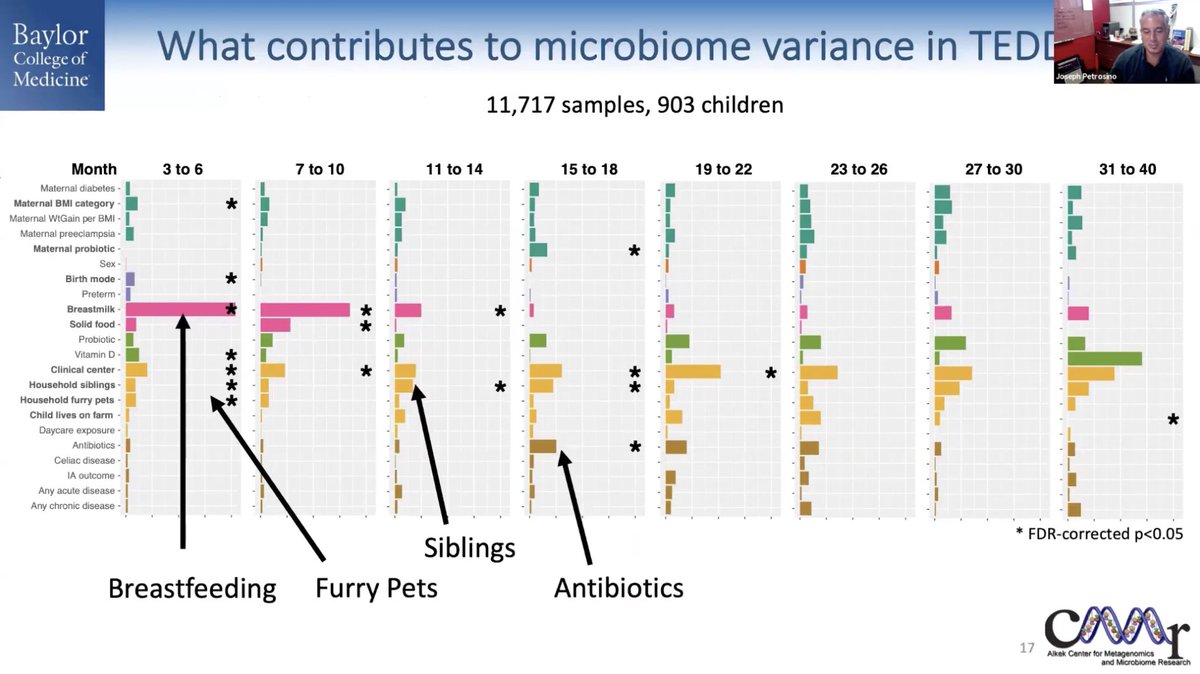
Fascinating large study identifying determinants in the development of type 1 #diabetes 



10 distinct bacterial communities in infants. These get more diverse over time.
Breastfeeding, furry pets, siblings, and antibiotics all had significant effects on the development of the #microbiome.

Breastfeeding, furry pets, siblings, and antibiotics all had significant effects on the development of the #microbiome.

Specific viral infections are associated with the development of type 1 #diabetes.
Enteroviruses (especially B). Infection with adenovirus C within 6 months of birth appears to be protective.
Enteroviruses (especially B). Infection with adenovirus C within 6 months of birth appears to be protective.

Sex, asthma, breastfeeding, and #probiotics impact fungal composition 





No differences in Candida abundance in type 1 #diabetes. 

Pichia kudriavzevii was not found to be associated with #asthma 

Candida sake was associated with #celiac disease, but not C. albicans 

@JosephPetrosino summary 

Eamonn Quigley on the clinical implications of the #mycobiome. What is the deal with Candida? Is "candida overgrowth" or #SIFO real? Does candidal dysbiosis contribute to #GI symptoms? 


Lots of online pseudoscience around "candida overgrowth" claiming that it causes anything and everything, and prescribing "candida killing" diets 




Fungal infections in the #GI tract include oropharyngeal and esophageal candidiasis. Immunosuppressed patients predispose to fungal infections. 

Candidemia is a potentially life-threatening fungal infection of the blood. This is almost always in immunocompromised hosts. 

Critical illness with prolonged use of broad spectrum antibiotics can lead to fungal diarrhea which resolves with nystatin. 

What about small intestinal fungal overgrowth (#SIFO)?
In 150 patients with unexplained #GI symptoms (probably DGBIs)
🦠63% had #SIBO or SIFO
🦠Dysmotility was risk factor for SIBO/SIFO
🦠PPI protected against SIFO
❓No evidence that SIBO/SIFO contributed to symptoms

In 150 patients with unexplained #GI symptoms (probably DGBIs)
🦠63% had #SIBO or SIFO
🦠Dysmotility was risk factor for SIBO/SIFO
🦠PPI protected against SIFO
❓No evidence that SIBO/SIFO contributed to symptoms


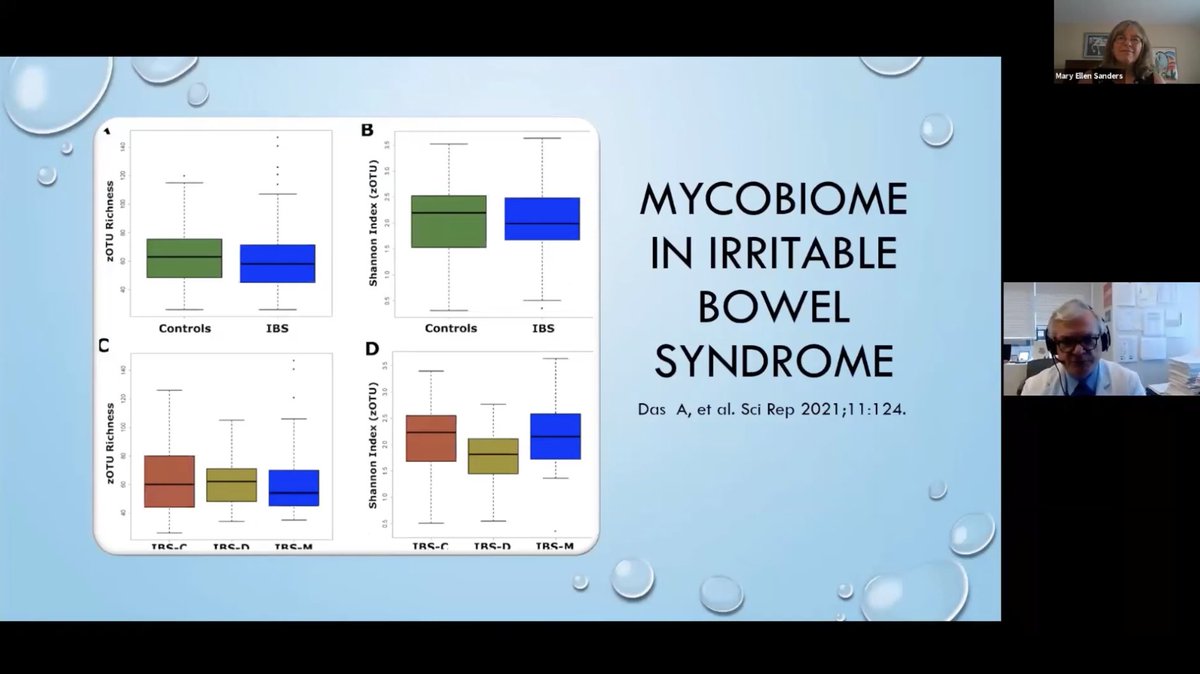
No difference in #mycobiome richness or diversity in #IBS compared to healthy controls, and no difference between IBS subtypes. Minor differences were present. 



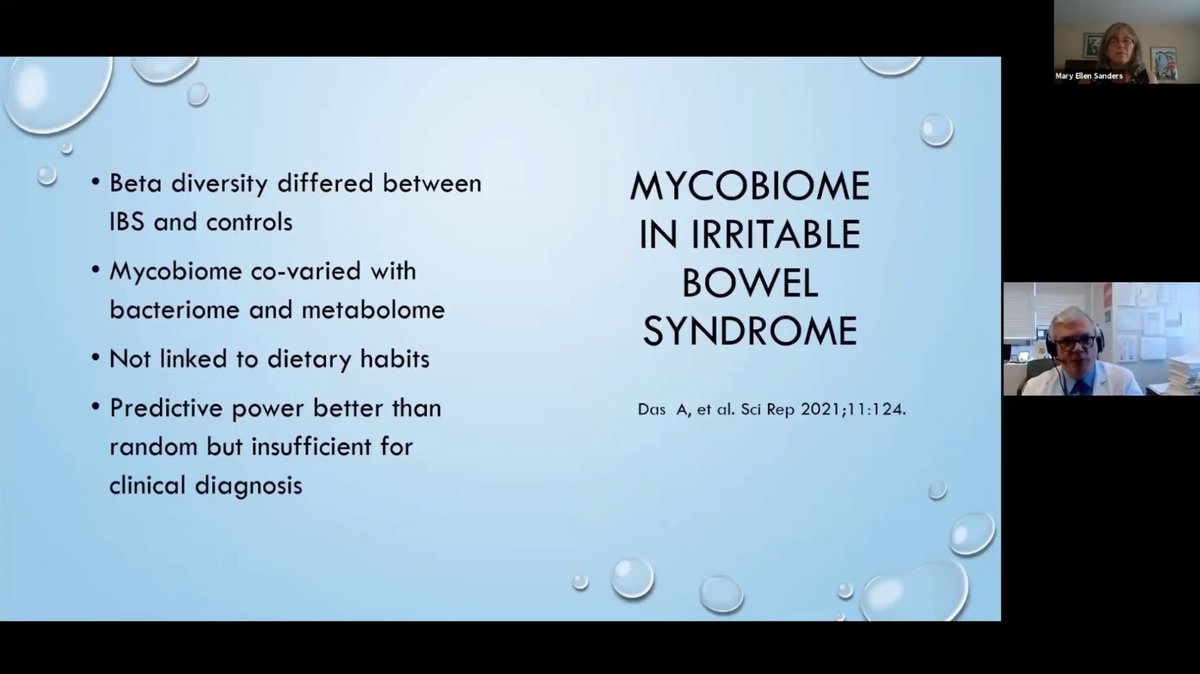
In another study, #IBS patients were divided into those with and without visceral hypersensitivity. The IBS patients had an altered #mycobiome compared to controls, but VH did not matter. In mice, however, VH was found to be affected by the mycobiome. 

Diet is an important contributor to the #mycobiome. Even one bite of bread can ⬆️ gut Saccharomyces!
Brushing teeth 3 (vs 1) times per day ⬇️ gut Candida albicans
Brushing teeth 3 (vs 1) times per day ⬇️ gut Candida albicans

@ISAPPscience seminar!
• • •
Missing some Tweet in this thread? You can try to
force a refresh