1) Welcome to @cardiomet_CE's series on #lipid management! This is a 10-#tweetorial program, all #accredited, that will cover IT ALL. The expert author for this module is Robert Giugliano MD @ @rgiugliano, renowned #cardiologist from @BrighamWomens & @harvardmed ! 

2) This #tweetorial, accredited for #CME/CE and intended for #physicians #physicianassociates #nurses #nursepractitioners #pharmacists is supported by an educational grant from Esperion Therapeutics. See faculty disclosures at cardiometabolic-ce.com/disclosures/.
3) @rgiugliano is going to discuss care of patients taking #statins who still have residual atherosclerotic cardiovascular disease #ASCVD risk.
4) What factors contribute to ASCVD risk?
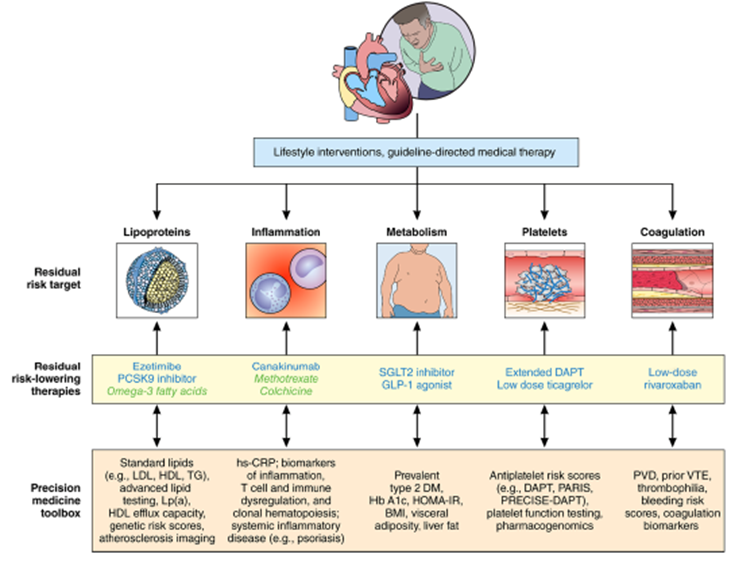
The 5⃣ major factors⬆️the risk of ASCVD include disorders of lipoproteins, inflammation, metabolism, platelet function, & hypercoagulability. Of these factors, lipid lowering has proven to have the largest effect & is easiest to treat.
The 5⃣ major factors⬆️the risk of ASCVD include disorders of lipoproteins, inflammation, metabolism, platelet function, & hypercoagulability. Of these factors, lipid lowering has proven to have the largest effect & is easiest to treat.
5) Over time we have developed a conceptual framework for addressing residual #ASCVD risk in the era of #PrecisionMedicine.
Figure from 🔓pubmed.ncbi.nlm.nih.gov/29643058/
Figure from 🔓pubmed.ncbi.nlm.nih.gov/29643058/
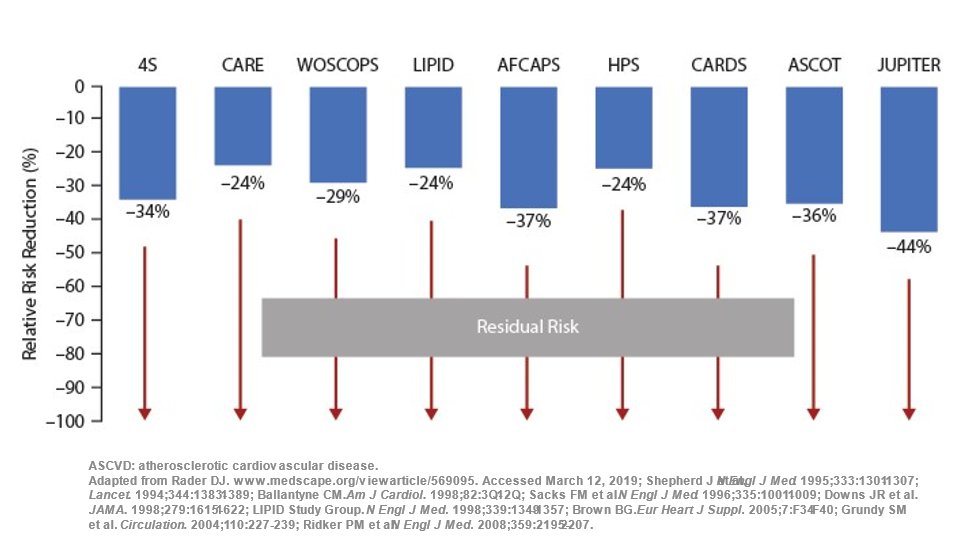
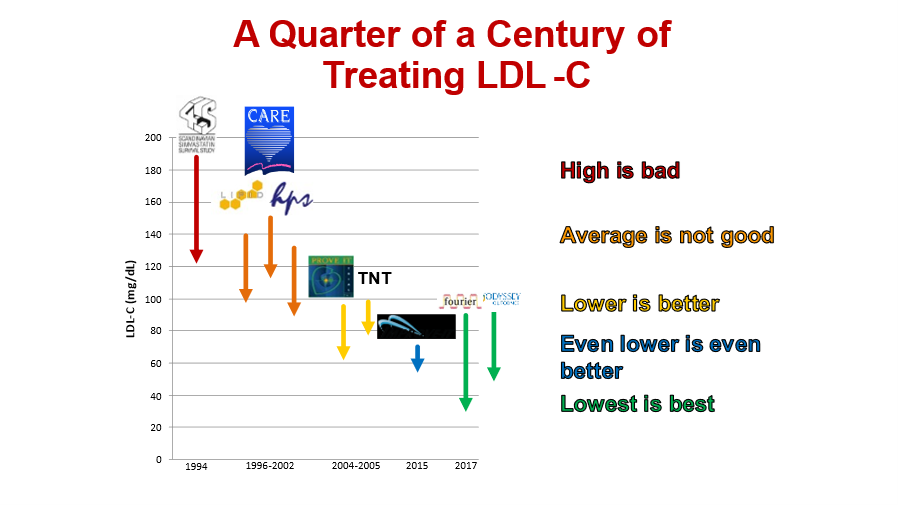
6) We have a 20-year track record of the benefits of statins in lowering #LDL-C: RCTs starting with the 4S trial in pts w/ avg LDL ~190 mg/dL & then moving to trials in pts w/ baseline LDLs <100 mg/dL showed⬇️in #CV events proportional to the LDL ⬇️(~22% per 40 mg/dL reduction) 
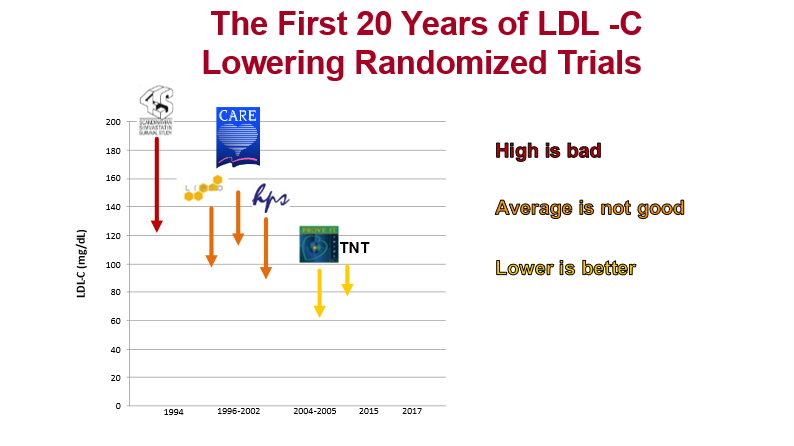
7) And yet, considerable residual risk persists despite intensive statin monotherapy.
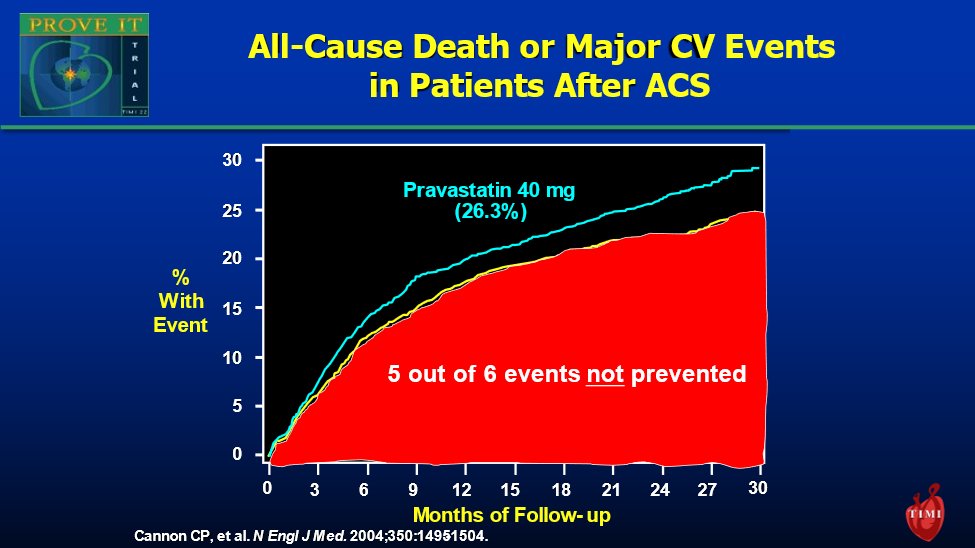
9) For example, only ~1/6 events were prevented with #atorvastatin 80 (compared to #pravastatin 40) in the PROVE IT-TIMI 22 trial. Could even more intensive LDL lowering help?
See 🔓nejm.org/doi/full/10.10… by @cardiomet_CE faculty @cpcannon et al
See 🔓nejm.org/doi/full/10.10… by @cardiomet_CE faculty @cpcannon et al
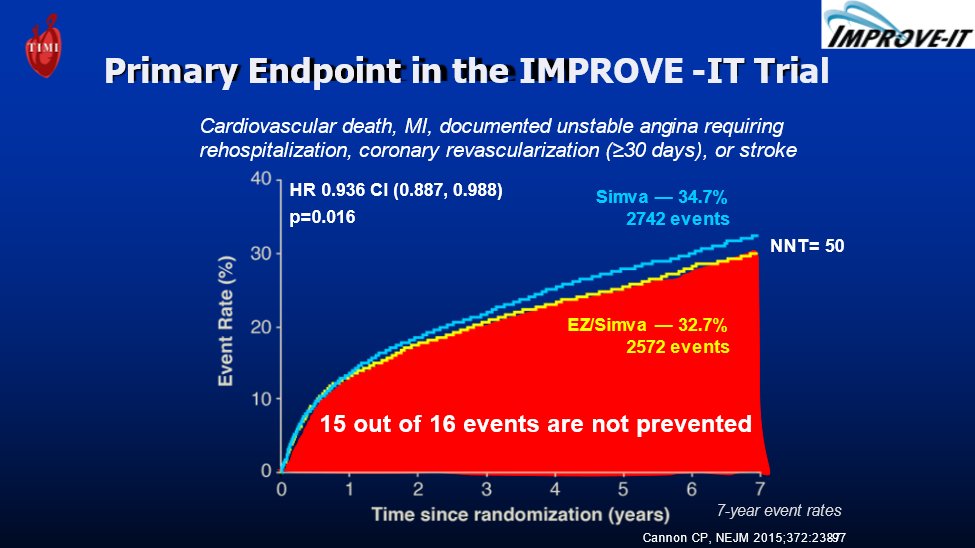
10) In fact, residual risk persists despite #statin+#ezetimibe & average LDL=54 mg/dL. Only ~1/16 events were prevented with #simvastatin 40+ezetimibe (comp to simva 40). Do we need STILL more potent therapies to achieve EVEN LOWER LDLs? @cpcannon again:🔓nejm.org/doi/full/10.10… 
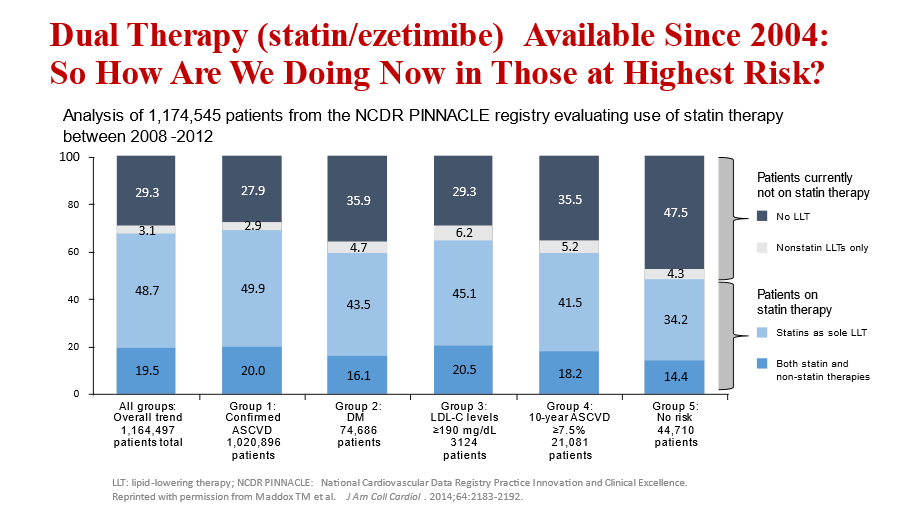
11) So we are saying that despite 2⃣proven #LDL-lowering therapies that ⬇️#CV risk, most patients are undertreated:
🔓pubmed.ncbi.nlm.nih.gov/25447259/ from @medtmaddox et al
🔓pubmed.ncbi.nlm.nih.gov/25447259/ from @medtmaddox et al
12) So what other options are there beyond statin and ezetimibe?
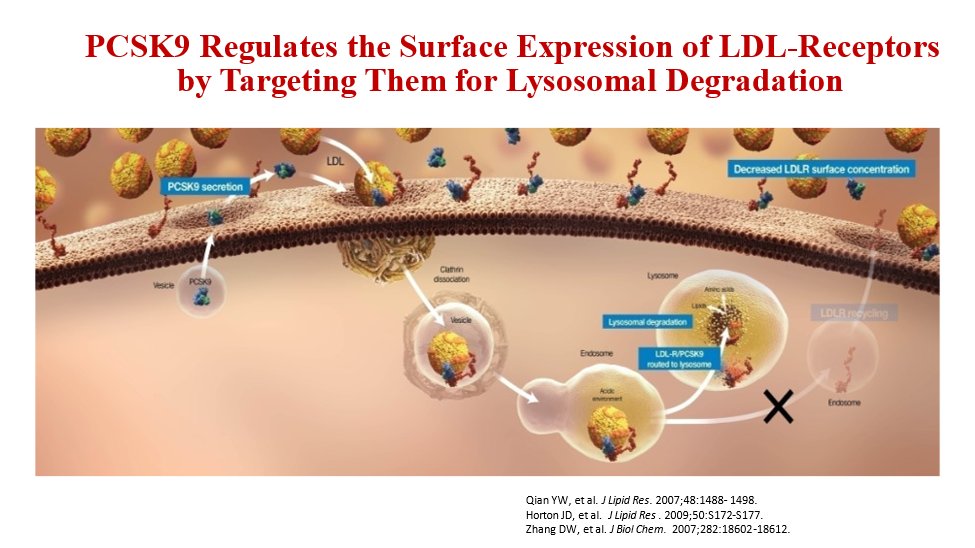
#PCSK9 inhibitors upregulate LDL-receptors by blocking the PCSK9 protein which function is to escort the LDL-receptor to its destruction within the cell
#PCSK9 inhibitors upregulate LDL-receptors by blocking the PCSK9 protein which function is to escort the LDL-receptor to its destruction within the cell
13) 2⃣ large outcome trials of PCSK9 monoclonal antibodies demonstrated significant ⬇️in CV events when added to #statin therapy:
🔓nejm.org/doi/10.1056/NE…
🔓nejm.org/doi/full/10.10…

🔓nejm.org/doi/10.1056/NE…
🔓nejm.org/doi/full/10.10…


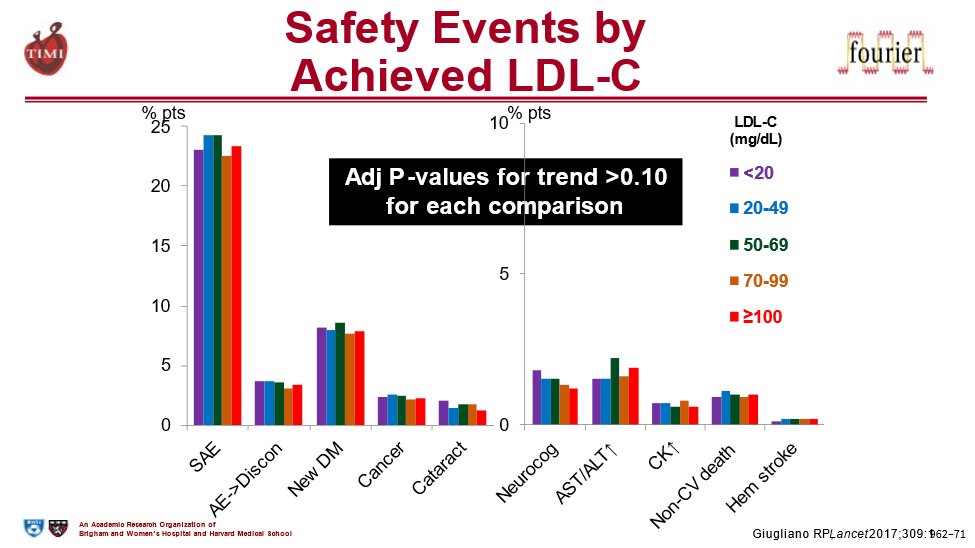
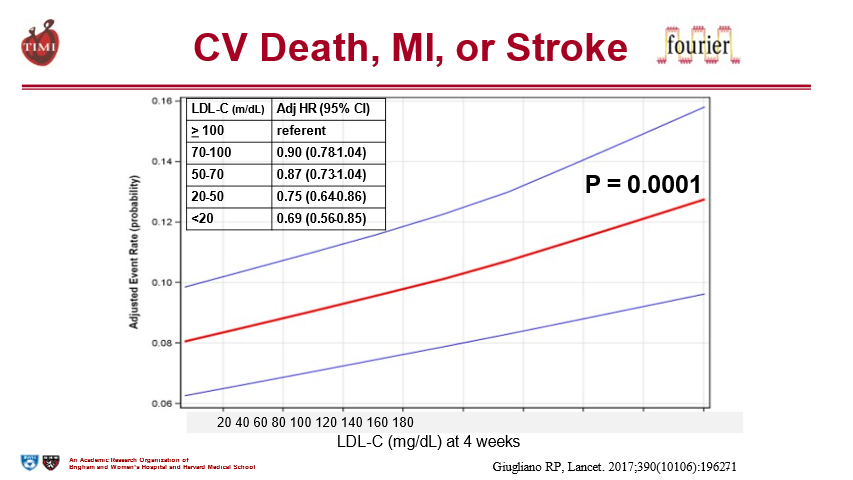
14) There was no “floor” to LDL levels with benefit extending to patients even <2⃣0⃣ mg/dL!
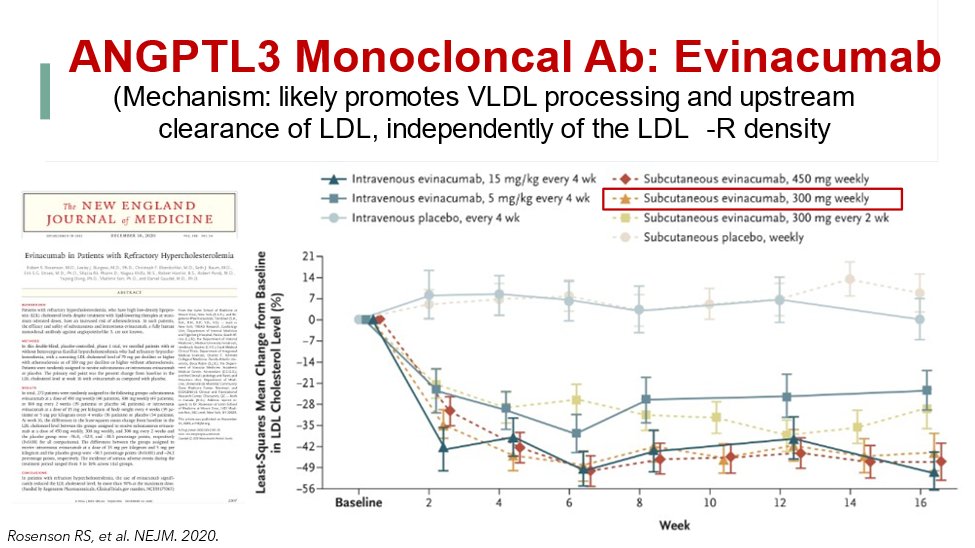
See thelancet.com/journals/lance…
See thelancet.com/journals/lance…
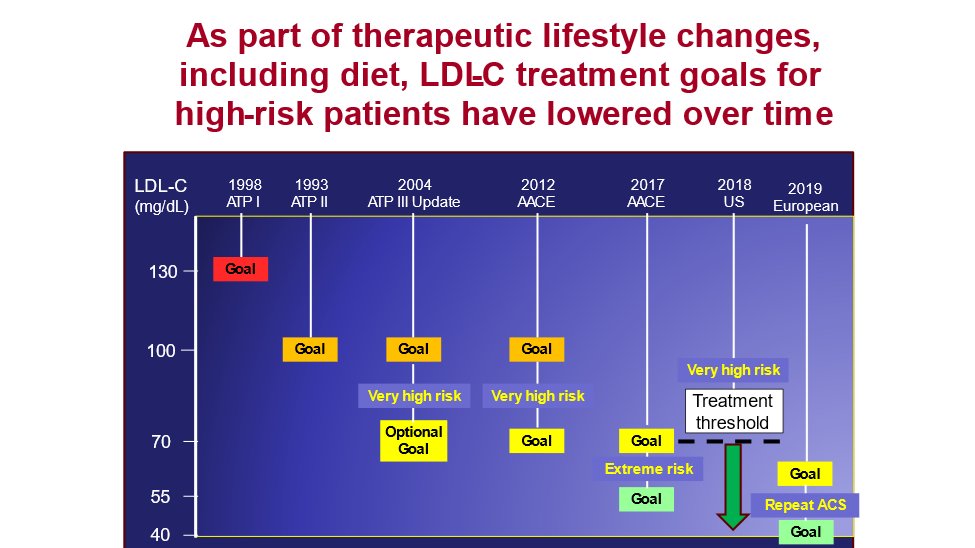
17) These advances in #lipid lowering therapies have been reflected in the latest guidelines that recommend much, much lower LDLs in patients at high risk. The most recent European 🇪🇺 guidelines target <40 mg/dL in high risk pts with recurrent events 
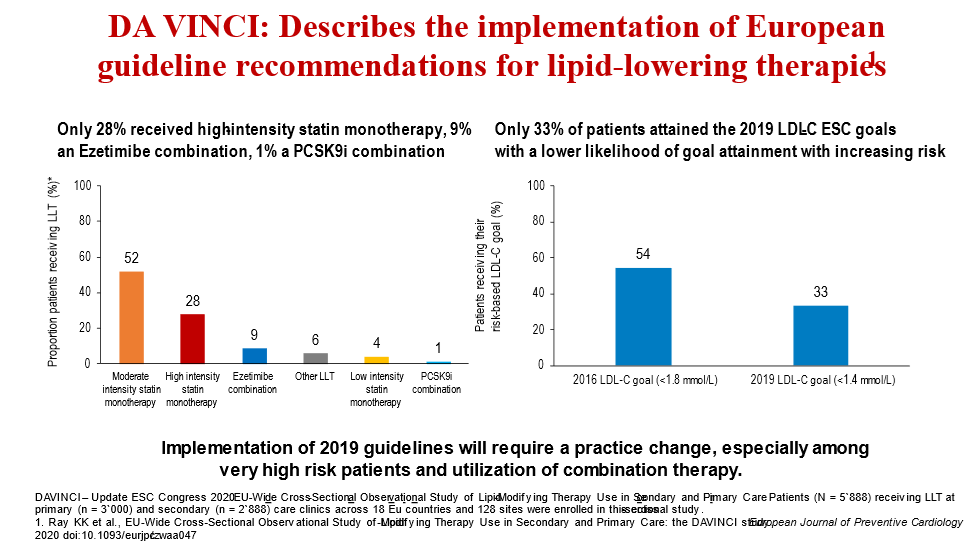
18) Implementation of 2019 guidelines will require a practice change, especially among very high-risk patients and utilization of combination therapy.
See 🔓academic.oup.com/eurjpc/article… from @cardiomet_CE faculty @ProfKausikRay et al:
See 🔓academic.oup.com/eurjpc/article… from @cardiomet_CE faculty @ProfKausikRay et al:
19) And monoclonal antibodies to PCSK9 are expensive and require self-injections every 2-4 weeks. So other options are needed. And this seems like a good time for a knowledge ✔️. Which of the following is NOT a recently @US_FDA-approved lipid-lowering therapy?
20) Mark your answer and return TOMORROW for more on the evaluation & treatment options for pts w/⬆️LDL-C despite #statins!
Nods to @HeartOTXHeartMD @HeartBobH @purviparwani @rblument1 @MinnowWalsh @Drlipid @SABOURETCardio @mmamas1973 @pnatarajanmd @Hragy @natraff8 #FOAMed
Nods to @HeartOTXHeartMD @HeartBobH @purviparwani @rblument1 @MinnowWalsh @Drlipid @SABOURETCardio @mmamas1973 @pnatarajanmd @Hragy @natraff8 #FOAMed
21) Welcome back! You are learning from expert author @rgiugliano about evaluating high-CV-risk pts with persistently elevated #LDL-C despite #statins. And you are earning CE/#CME! Welcome, @MedTweetorials #CardioTwitter #endotwitter @aayshacader @VietHeartPA @Lross246
22) So, as we were saying yesterday, the latest approved lipid therapies are in fact:
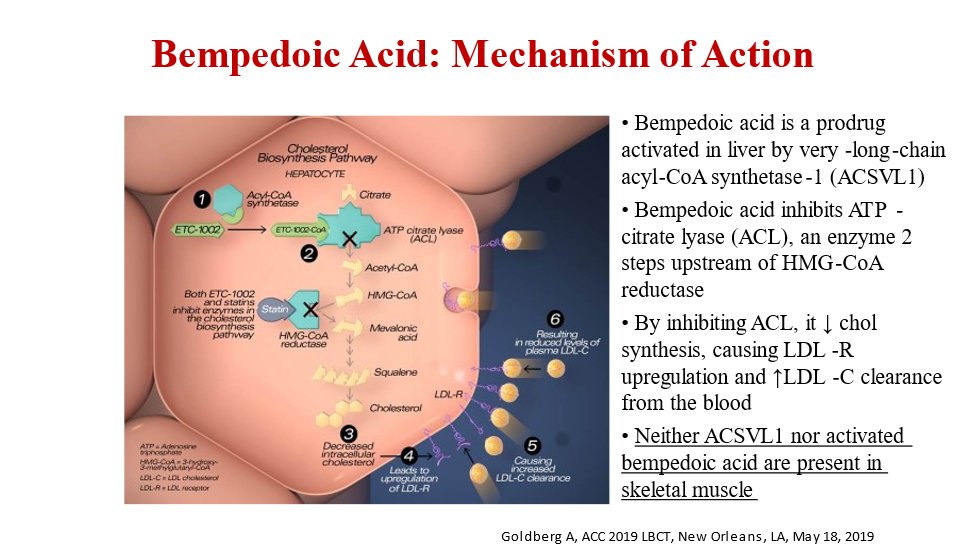
1⃣ # bempedoic Acid (ATP citrate lyase inhibitor)
2⃣ #evinacumab (#ANGPTL3 Monoclonal Antibody)
3⃣ #inclisiran (RNAi)
1⃣ # bempedoic Acid (ATP citrate lyase inhibitor)
2⃣ #evinacumab (#ANGPTL3 Monoclonal Antibody)
3⃣ #inclisiran (RNAi)
23) Bempedoic acid inhibits ATP-citrate lyase (ACL), an enzyme 2⃣ steps upstream⤴️of HMG-CoA reductase. Since ACL isn’t in skeletal muscle💪, bempedoic acid doesn’t cause muscle side effects. 
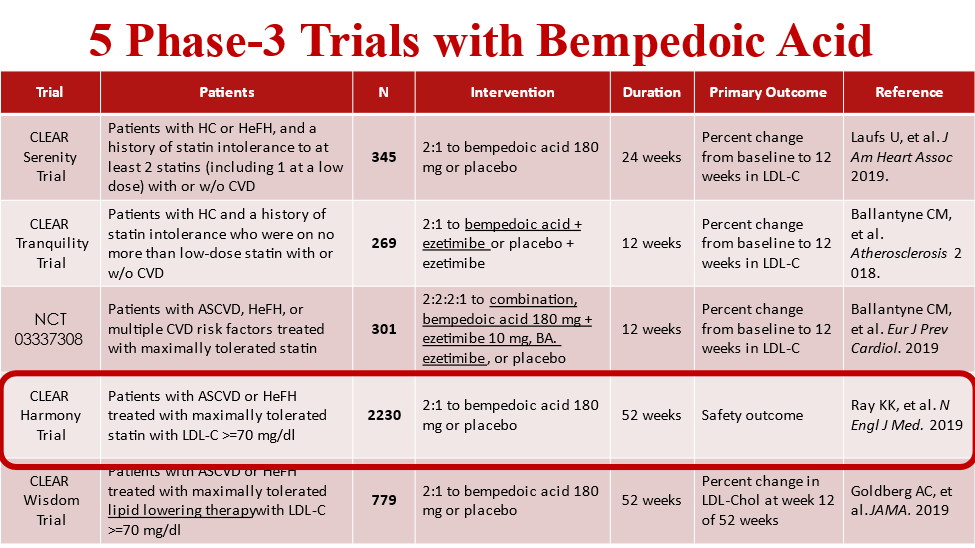
24) Bempedoic acid alone and in combo with #ezetimibe has been studied in 5⃣ Ph 3 lipid-lowering trials. The largest was CLEAR-HARMONY in 2230 pts. From our @cardiomet_CE faculty @ProfKausikRay, @CBallantyneMD, and others: 🔓nejm.org/doi/full/10.10… 
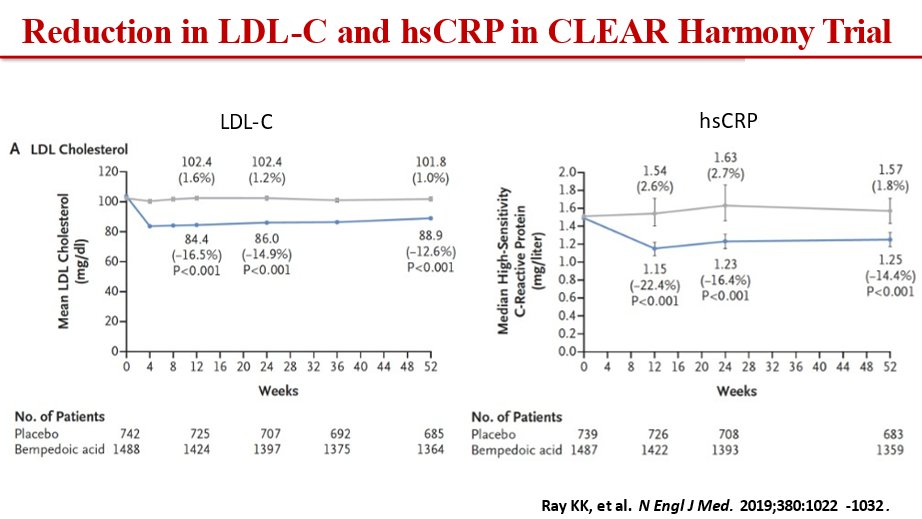
25) In CLEAR-HARMONY, bempedoic acid⬇️LDL by 16.5% and #hsCRP by 22.4% at 12 wks vs placebo. (Again 🔓nejm.org/doi/full/10.10… ) 
26) A different way to lower LDL is to block angiopoietin-like 3 (#ANGPTL3), which inhibits lipoprotein lipase and endothelial lipase. See 🔓mdpi.com/2308-3425/5/3/… for more 
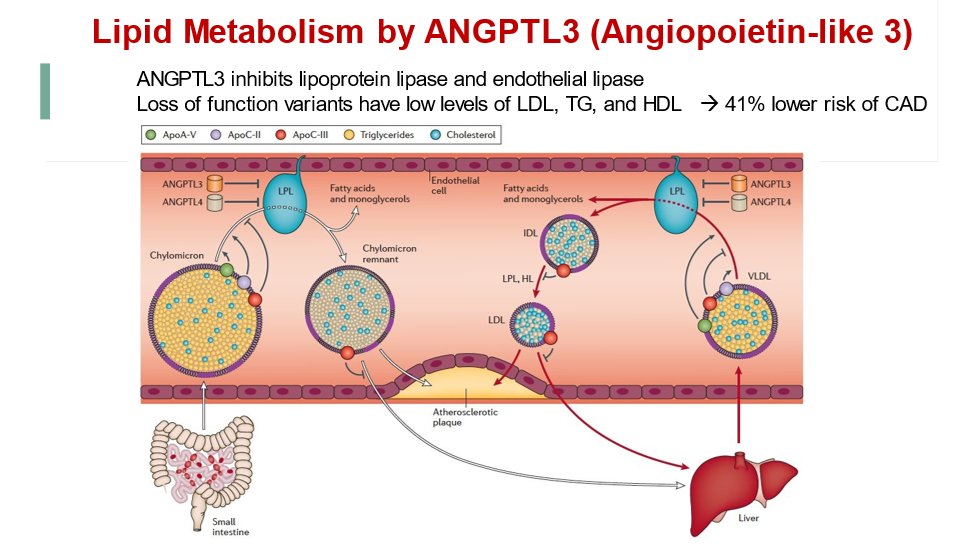
27) #Evinacumab is a monoclonal antibody inhibiting ANGPTL3 and was approved for use in familial hypercholesterolemia #FH in 2021. See 🔓nejm.org/doi/full/10.10… 
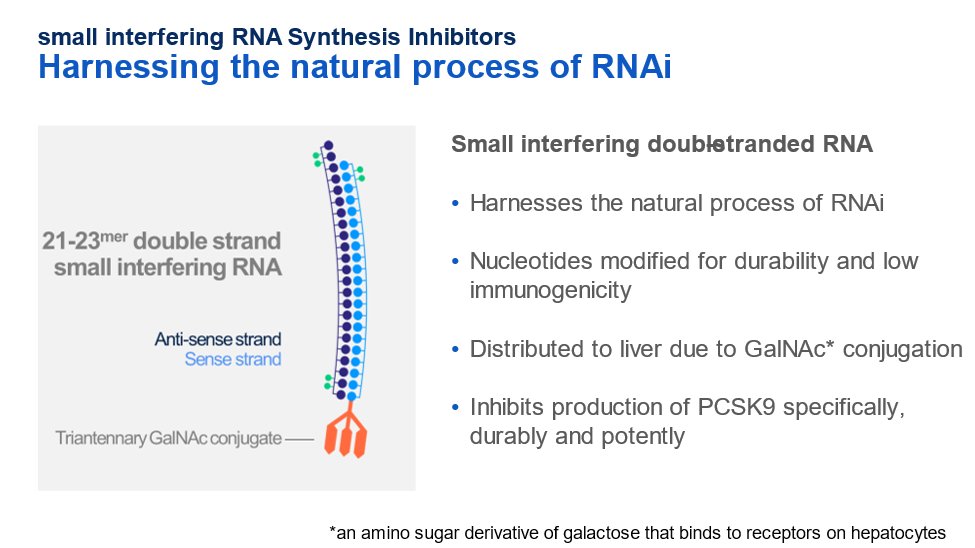
28) In Dec 2021, inclisiran, a small-interfering double-stranded RNA that blocks production of the PCSK9 mRNA was approved by @US_FDA for use in patients with #hyperlipidemia. It is given as a twice annual injection by the healthcare provider. 
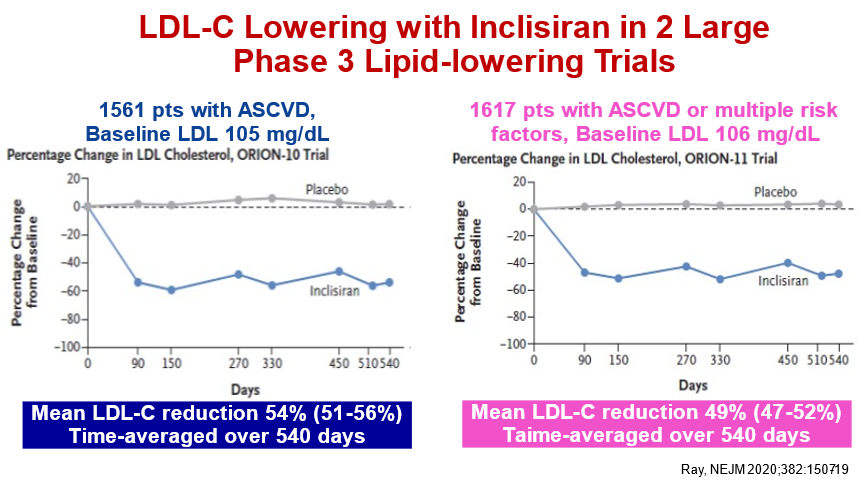
29) In Ph 3 lipid-lowering trials, inclisiran⬇️LDL-C by ~50% after injections at day 0, 90, 270 and twice annually thereafter. (Here's our @cardiomet_CE faculty and President of the European Atherosclerosis Society @ProfKausikRay again, with 🔓nejm.org/doi/full/10.10… ) 
30) What major lipid-lowering studies can we expect in 2022 and beyond?
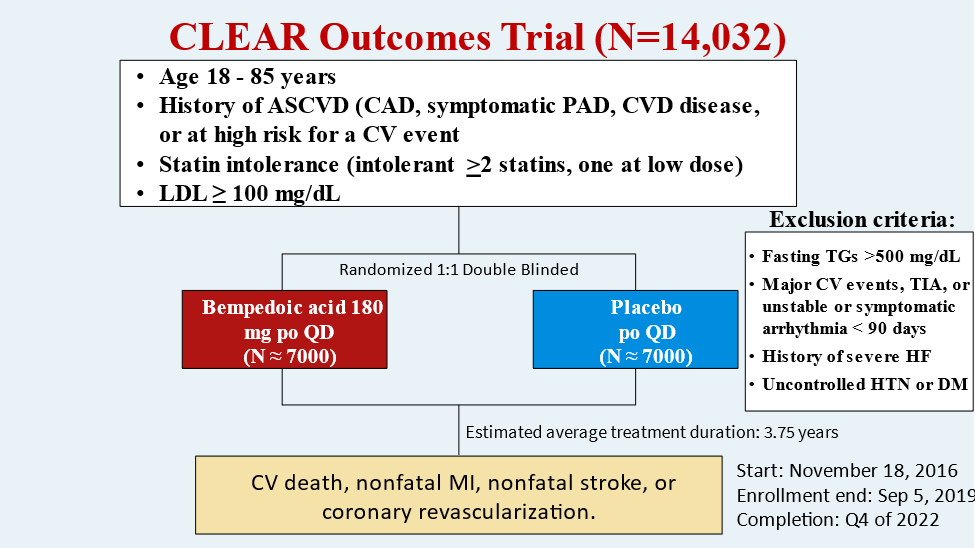
CLEAR-OUTCOMES, a phase 3 CV outcomes trial of #bempedoic acid in pts with #ASCVD intolerant of statins completed enrollment of 14,032 in Sept 2019 with results coming expected in 2023.
CLEAR-OUTCOMES, a phase 3 CV outcomes trial of #bempedoic acid in pts with #ASCVD intolerant of statins completed enrollment of 14,032 in Sept 2019 with results coming expected in 2023.
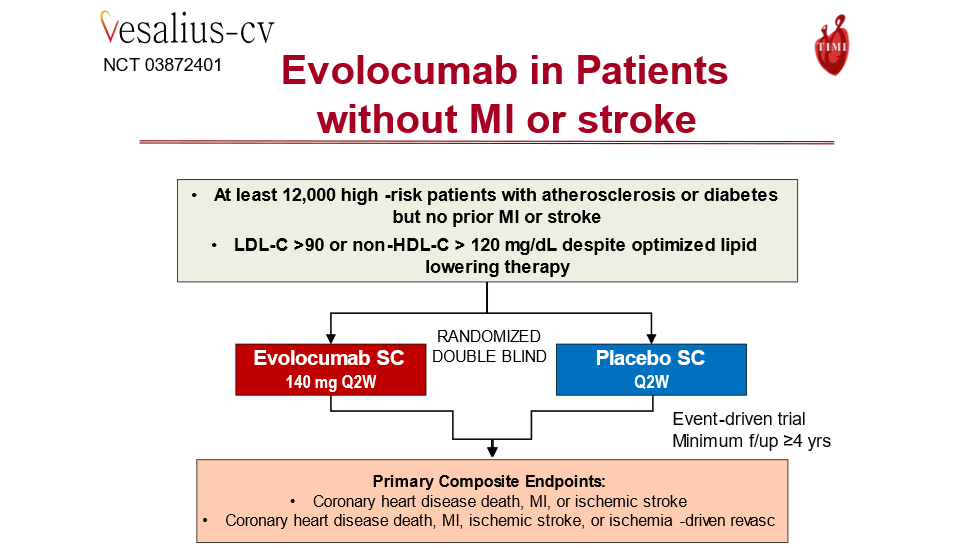
31) VESALIUS CV is a Ph 3 #CV outcomes trial of #evolocumab in >12,000 patients at high risk for ASCVD but no prior #MI or #stroke. It completed enrollment in 2021 and follow-up continues. 
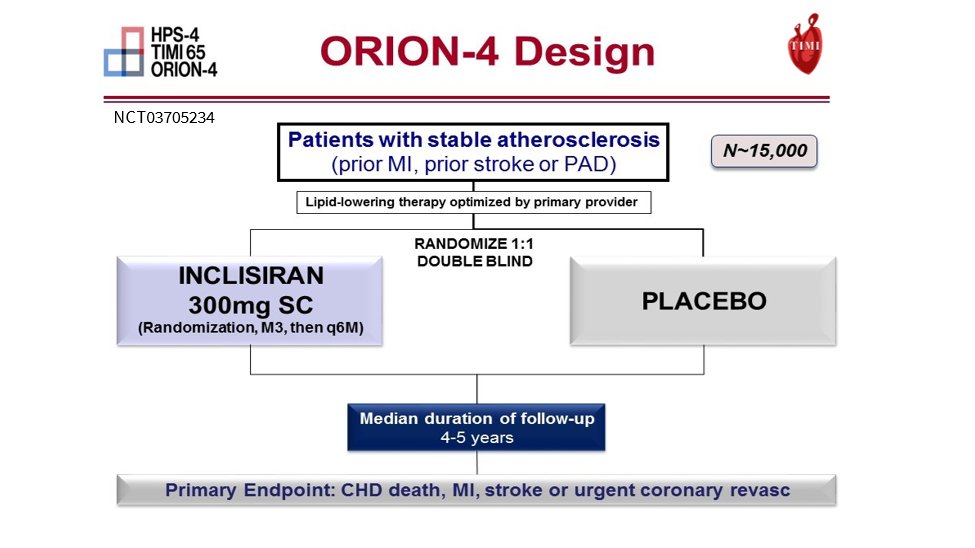
32) And ORION-4 is a Ph 3 CV outcomes trial of inclisiran in ~15,000 patients with stable #ASCVD on maximally tolerated #statin and continues to enroll in 2022. 
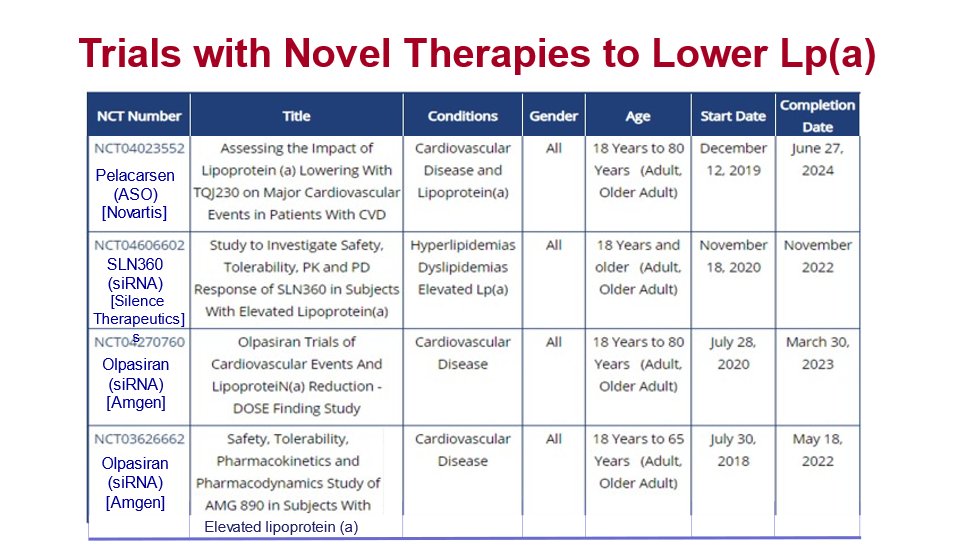
33) Several trials are ongoing with new therapies to lower #lipoprotein (a). Even if the LDL level is very low, high Lp(a) levels confer risk that is not addressed by proven LDL-lowering therapies or lifestyle modification. 
34) So now you know the new & emerging treatment options. You know that in terms of lowering #ASCVD risk, ⬇️LDL remains a central focus (lowest is best!). Despite statin+ezetimibe, LDL⬇️is often not optimal, so if further⬇️ needed, think #PCSK9i, #bempedoic acid, #evinacumab.
35) So there's just one topic left--how do we efficiently, and EARLY on, identify those who remain at residual risk? What do you think? Which of the following is NOT a feature of the highest risk pts?
36) Mark your answer and return TOMORROW for a wrap-up of this program--focusing on the DIAGNOSTICS--and your #CME/CE credit--#physicians #physicianassociate #NurseTwitter #Pharmacist.
Shout-outs to @EugeniaGianos @mvaduganathan @SOTHCardiology @KoushikReddyMD @Drlipid
Shout-outs to @EugeniaGianos @mvaduganathan @SOTHCardiology @KoushikReddyMD @Drlipid
37) Welcome back! You are just a few 🖱️clicks away from your🆓CE/#CME! I am @rgiugliano and we are wrapping up this discussion about pts who remain hyperlipidemic despite statin monotherapy.
Hi to @CardRenalForum @kaulcsmc @GoggleDocs @johnwmcevoy @PamelaBMorris @fjpinto1960
Hi to @CardRenalForum @kaulcsmc @GoggleDocs @johnwmcevoy @PamelaBMorris @fjpinto1960
38) Some patients do not have the expected response to statins, while others may experience side effects. Be sure to look for a #tweetorial in this series from @DrMarthaGulati on statin intolerance!
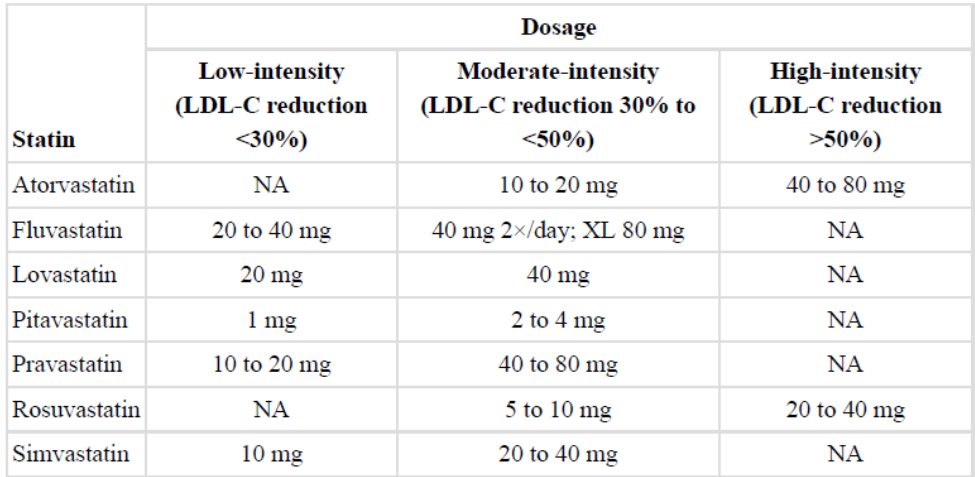
39) Here's the expected LDL-C level response to commonly used statins (from 🔓pubmed.ncbi.nlm.nih.gov/24239923/: 
40) "Statin resistance" is a term used to describe the failure to reach LDL-C target values despite statin therapy. Resistance to statins has been associated, among others, with polymorphisms in several genes.
41) Pseudo-resistance due to nonadherence is probably the main cause of insufficient LDL-cholesterol response to statins.
See sciencedirect.com/science/articl…
See sciencedirect.com/science/articl…
42) Statin intolerance is the inability to tolerate statin at all or to tolerate a full dose having adverse effects, mostly myopathy.
Statins may also cause transaminitis (usually dose-related and reversible) and rarely, renal failure due to rhabdomyolysis
Statins may also cause transaminitis (usually dose-related and reversible) and rarely, renal failure due to rhabdomyolysis
43) As we have discussed, for patients who are statin-resistant or statin-intolerant, several other treatment possibilities are nowadays available. Here's how we might evaluate: 
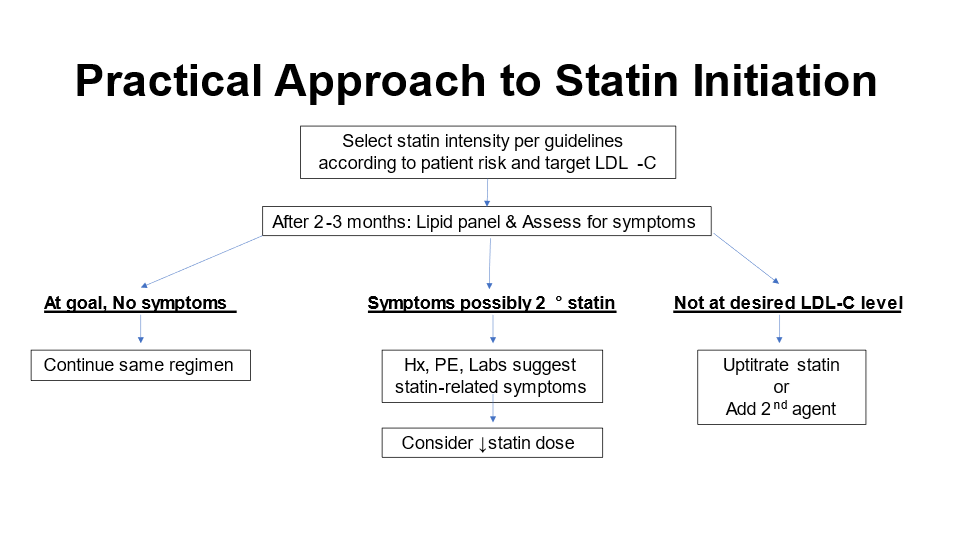
44) So what is the best approach to⬇️ residual risk?
--Assess LDL-C 2-3 months after starting statin
--Measuring non-HDL-C and Apolipoprotein B gives even more precise guidance
--Re-review and optimize lifestyle modification strategies as indicated
--Assess LDL-C 2-3 months after starting statin
--Measuring non-HDL-C and Apolipoprotein B gives even more precise guidance
--Re-review and optimize lifestyle modification strategies as indicated
45)
--Add 2nd agent (e.g., ezetimibe or combo ezetmimibe+bempedoic acid)
--Some patients even need a 3rd agent (e.g., PCSK9 inhibitor)
--Treat triglycerides if >150 mg/dL (e.g., icosapent ethyl)
--Add 2nd agent (e.g., ezetimibe or combo ezetmimibe+bempedoic acid)
--Some patients even need a 3rd agent (e.g., PCSK9 inhibitor)
--Treat triglycerides if >150 mg/dL (e.g., icosapent ethyl)
46) It's also important to assess and manage non-lipid factors, such as regular reviews of lifestyle mods, as above.
Also think about "if/then" strategies:
⬆️Inflammation? colchicine if CAD
Metabolic factors? #SGLT-2i's, #GLP-1 RAs
Also think about "if/then" strategies:
⬆️Inflammation? colchicine if CAD
Metabolic factors? #SGLT-2i's, #GLP-1 RAs
47) more If/Thens?
High risk ACS or complex PCI? Consider more intensive or longer duration of #antiplatelet therapies
Signs of #PAD too? Consider rivaroxaban 2.5 mg BID
Just always remember the LDL-C mantra: LOWEST IS BEST
High risk ACS or complex PCI? Consider more intensive or longer duration of #antiplatelet therapies
Signs of #PAD too? Consider rivaroxaban 2.5 mg BID
Just always remember the LDL-C mantra: LOWEST IS BEST
48) And that's it! You just earned 0.5h CE/#CME. Go to cardiometabolic-ce.com/lipids1/ to claim your credit! And FOLLOW US here on @cardiomet_CE for more #accredited #tweetorials. Expert education--brought to you! I am @rgiugliano
• • •
Missing some Tweet in this thread? You can try to
force a refresh