
So this has been making the rounds. I realize it’s probably meant to be a thought experiment & deliberately provocative, but still, philosophical arguments should be rooted in at least some amount of reality.
I will now rage tweet about everything wrong w/ this concept. Enjoy🧵
I will now rage tweet about everything wrong w/ this concept. Enjoy🧵

Let’s start w/ the author’s premise: if we’re ok w/ #organdonation after brain death, then we should be ok w/ “whole body gestational donation” (WBGD).
Even putting aside the part about this sounding like a horrifying, dystopian baby farm, they’re not even remotely comparable.
Even putting aside the part about this sounding like a horrifying, dystopian baby farm, they’re not even remotely comparable.

Here’s why:
#Organdonation after brain death typically happens very quickly (a few days or less). This is not simply because we’re uncomfortable keeping someone’s organs alive longer; it’s because it’s incredibly challenging & often not possible, despite the authors assertions
#Organdonation after brain death typically happens very quickly (a few days or less). This is not simply because we’re uncomfortable keeping someone’s organs alive longer; it’s because it’s incredibly challenging & often not possible, despite the authors assertions
The author also makes several other statements that are patently false:
➡️ The amount of time on a ventilator is inconsequential (LOL)
➡️ Patients on ventilators look “warm” & have a “healthy color”
➡️ Ventilated organ donors won’t “decompose” unless some intervention occurs

➡️ The amount of time on a ventilator is inconsequential (LOL)
➡️ Patients on ventilators look “warm” & have a “healthy color”
➡️ Ventilated organ donors won’t “decompose” unless some intervention occurs


I mean…she actually does a great job of telling me she’s never been in an #ICU without actually telling me she’s never been in an ICU.
I am not usually this scathing, but there are just so many things wrong here.
I am not usually this scathing, but there are just so many things wrong here.
So what actually happens after #braindeath?
The #brain does not function in isolation. It affects every other organ in the body.
The #brain does not function in isolation. It affects every other organ in the body.
Cardiovascular system 🫀:
➡️ Initial catecholamine surge followed by loss of autonomic regulation, often leading to shock
➡️ Translation: vital organs do not get enough blood flow
⚠️ Common cause of organs becoming unsuitable for transplant
➡️ Initial catecholamine surge followed by loss of autonomic regulation, often leading to shock
➡️ Translation: vital organs do not get enough blood flow
⚠️ Common cause of organs becoming unsuitable for transplant
Lungs 🫁:
➡️ Neurogenic pulmonary edema, meaning fluid accumulates in the lungs
➡️ Longer time on the ventilator also increases the risk of pneumonia
➡️ Both issues make it harder to get enough oxygen to the body
➡️ Neurogenic pulmonary edema, meaning fluid accumulates in the lungs
➡️ Longer time on the ventilator also increases the risk of pneumonia
➡️ Both issues make it harder to get enough oxygen to the body
Endocrine system 🦋:
➡️ Hypothalamus & pituitary gland stop working
➡️ Loss of temperature regulation (development of fevers & hypothermia)
➡️ Diabetes insipidus often develops, causes high volume, dilute urine, resulting in dehydration & worsening shock
Among other things
➡️ Hypothalamus & pituitary gland stop working
➡️ Loss of temperature regulation (development of fevers & hypothermia)
➡️ Diabetes insipidus often develops, causes high volume, dilute urine, resulting in dehydration & worsening shock
Among other things
And what’s the impact of the body being completely immobile for months? You get things like:
➡️ Blood clots 🩸
➡️ Infections of all kinds 🦠
➡️ Skin, bone, & muscle breakdown
So yeah, the body does still “decompose” despite being ventilated
➡️ Blood clots 🩸
➡️ Infections of all kinds 🦠
➡️ Skin, bone, & muscle breakdown
So yeah, the body does still “decompose” despite being ventilated
It also takes a huge #ICU team to keep this going.
With everything we’ve seen during the pandemic, how can you not also think about resource allocation?
Especially in a journal about bioethics?
With everything we’ve seen during the pandemic, how can you not also think about resource allocation?
Especially in a journal about bioethics?
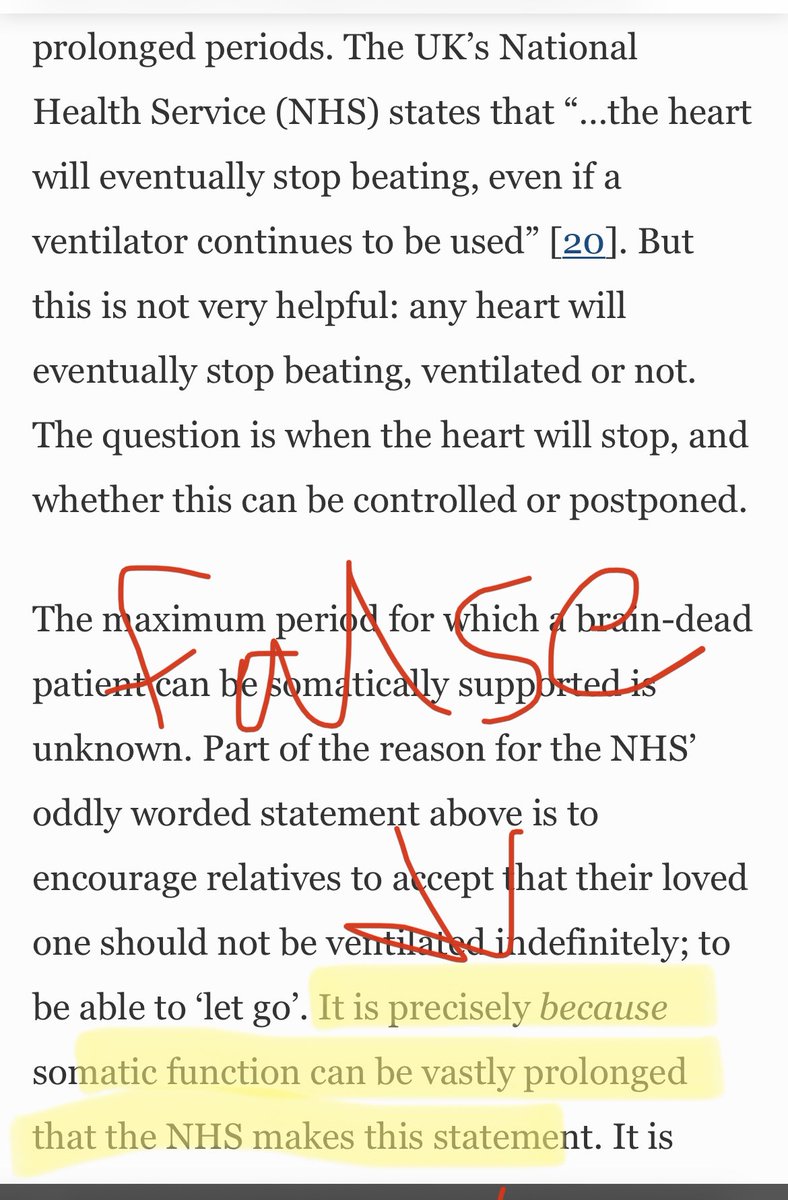
The author also claims that we don’t actually know how long the body can be sustained after brain death.
That’s fair - I can’t give you an exact # of days this can continue. But I do know how many things we’d be fighting against. So no, 9 months is not particularly realistic.
That’s fair - I can’t give you an exact # of days this can continue. But I do know how many things we’d be fighting against. So no, 9 months is not particularly realistic.
So what about the “organ recipient”? I would argue that this would include the baby born under these circumstances How would the baby do?
Based on a case series of 10 post-brain death gestations published 20 years ago, the author claims that these babies could do well.
Based on a case series of 10 post-brain death gestations published 20 years ago, the author claims that these babies could do well.
To be fair, there’s not a lot of data out there, but there is more than she cites. This systematic review looked at perinatal outcomes after brain death. Of 35 cases, one-third of the fetuses died or otherwise had poor outcomes.
doi.org/10.1016/j.ajog…
doi.org/10.1016/j.ajog…
There’s a bit more data about fetal outcomes in critically ill pregnant pts:
⚠️ Fetal death rate ~20%. Shock (which happens in brain death) significantly ⬆️ this risk
⚠️ High risk of prematurity & critical illness. We saw this in #COVID - >40% were premature, 50% needed NICU
⚠️ Fetal death rate ~20%. Shock (which happens in brain death) significantly ⬆️ this risk
⚠️ High risk of prematurity & critical illness. We saw this in #COVID - >40% were premature, 50% needed NICU
Some sources:
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
Another absurdly false claim made by the author: gestational age doesn’t limit fetal prognosis because of “advances in critical care.”
I guess every single neonatologist in the world missed that memo 😳🤯
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
Another absurdly false claim made by the author: gestational age doesn’t limit fetal prognosis because of “advances in critical care.”
I guess every single neonatologist in the world missed that memo 😳🤯

It gets next level nutty when she tries to argue that health equity shouldn’t be a concern here because the prospect of brain dead men getting pregnant isn’t actually science fiction because some guy said it was possible in 1999.
(Note: she is not talking about trans men)
(Note: she is not talking about trans men)

And that we should strive to eradicate pregnancy just as we try to eradicate measles since pregnancy is even more risky.
She’s not wrong that substantial risks come with pregnancy. But equating it to a disease? Just wow.
She’s not wrong that substantial risks come with pregnancy. But equating it to a disease? Just wow.

There’s more, but I’ve let my blood boil enough.
Perhaps people writing pieces like this should actually, you know, talk to an intensivist or obstetrician or neonatologist? Or at least just do a lit search?
How this got published in a peer-reviewed journal is mind-boggling.
Perhaps people writing pieces like this should actually, you know, talk to an intensivist or obstetrician or neonatologist? Or at least just do a lit search?
How this got published in a peer-reviewed journal is mind-boggling.
What bothers me most is not just that this is sloppy & full of factually incorrect claims, it’s also completely irresponsible. There already aren’t enough organ donors. Reading crap like this will (understandably) scare even more people away.
Ok, that’s enough for now. I think I need to looks at photos of puppies to make myself feel better after reading that horror show of a journal article.
But you found this thread interesting, please retweet.
But you found this thread interesting, please retweet.
https://twitter.com/nidaqadirmd/status/1621941742676377600
• • •
Missing some Tweet in this thread? You can try to
force a refresh






