
#Endocrinologist. Passionate about #obesity as a medical disease and a social misunderstanding. Tweets are my own. | #health #medtwitter #weightloss #medicine |
How to get URL link on X (Twitter) App


 Here's the study method:
Here's the study method:

 This is such an excellent talk that I don’t have much commentary to add. Just sharing high yield slides!
This is such an excellent talk that I don’t have much commentary to add. Just sharing high yield slides! 
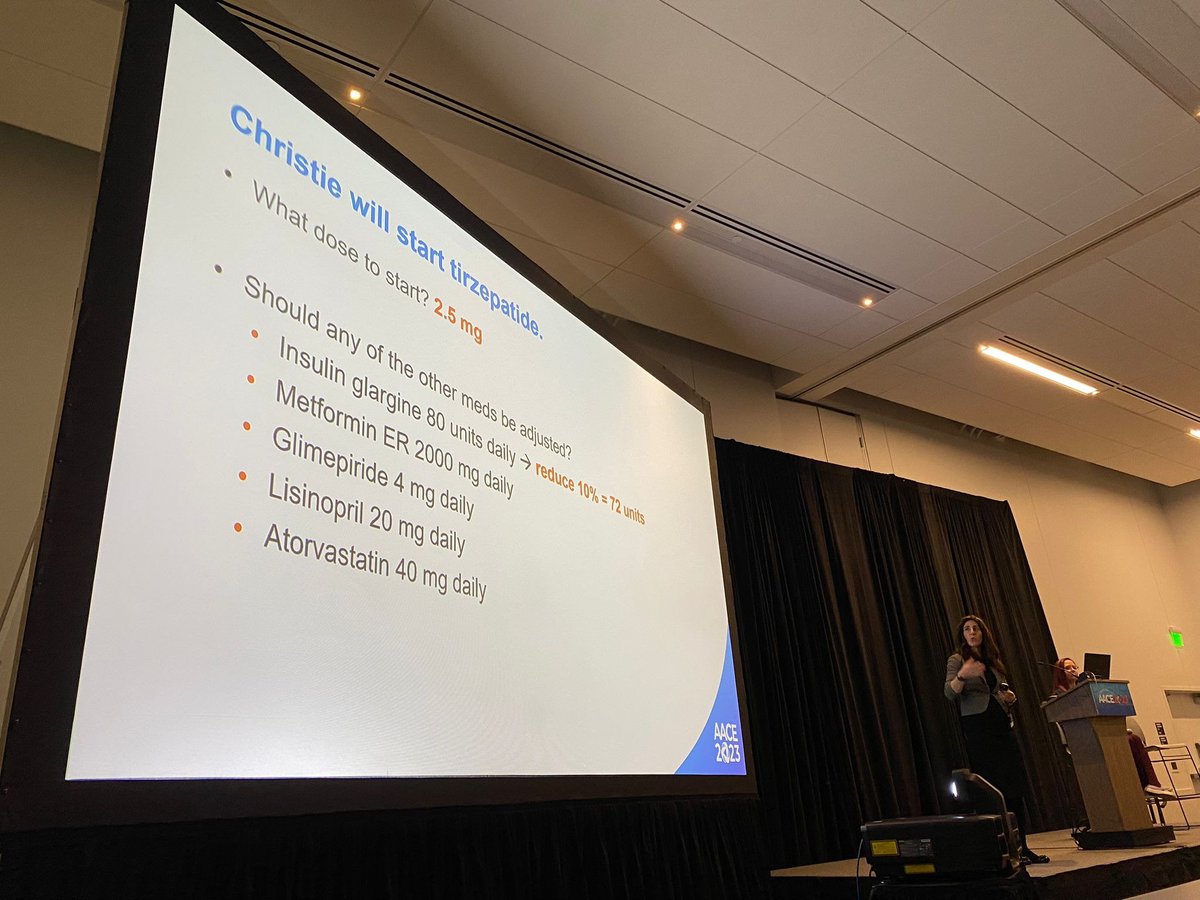
https://twitter.com/endojorm/status/1654224072979660800- "Tirzepatide is a dual agonist"

 👉Reduce #WeightStigma
👉Reduce #WeightStigma 

 @alpanashuklamd et al examined the effect of macronutrient sequencing (carbs first vs carbs last) in ppl with diabetes, prediabetes, or gestational diabetes
@alpanashuklamd et al examined the effect of macronutrient sequencing (carbs first vs carbs last) in ppl with diabetes, prediabetes, or gestational diabetes
 Many people remember his 14-day study of ultra processed foods (UPF) vs unprocessed foods (n=20) that found energy intake was ~500 kcal/d LESS with unprocessed meals
Many people remember his 14-day study of ultra processed foods (UPF) vs unprocessed foods (n=20) that found energy intake was ~500 kcal/d LESS with unprocessed meals 

 We often focus on slow or fast metabolism but there isn't enough talk on *energy efficiency*. See how much additional Δkcal is required (beyond that calculated) to effect 10% weight Δ: nejm.org/doi/full/10.10…
We often focus on slow or fast metabolism but there isn't enough talk on *energy efficiency*. See how much additional Δkcal is required (beyond that calculated) to effect 10% weight Δ: nejm.org/doi/full/10.10…

 Neurology:
Neurology: 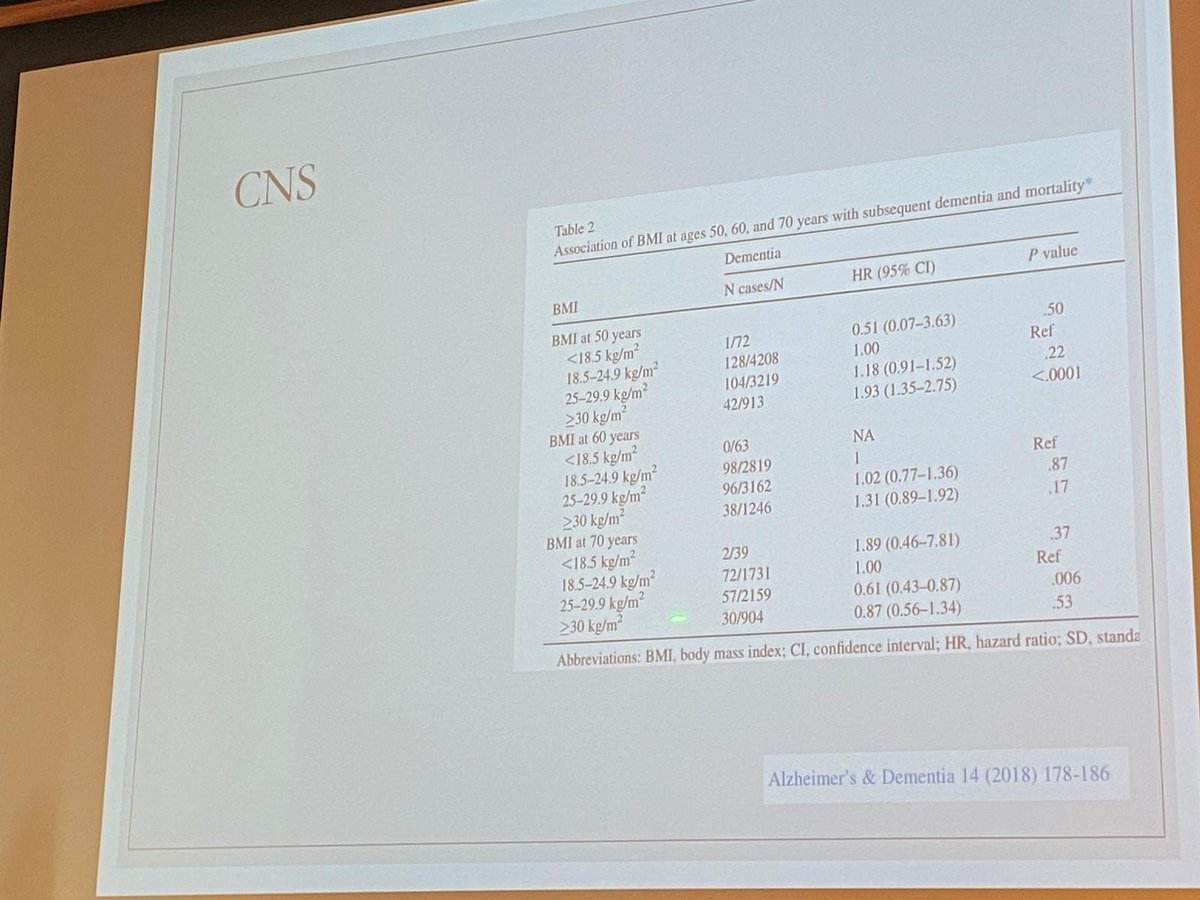

 For example:
For example: 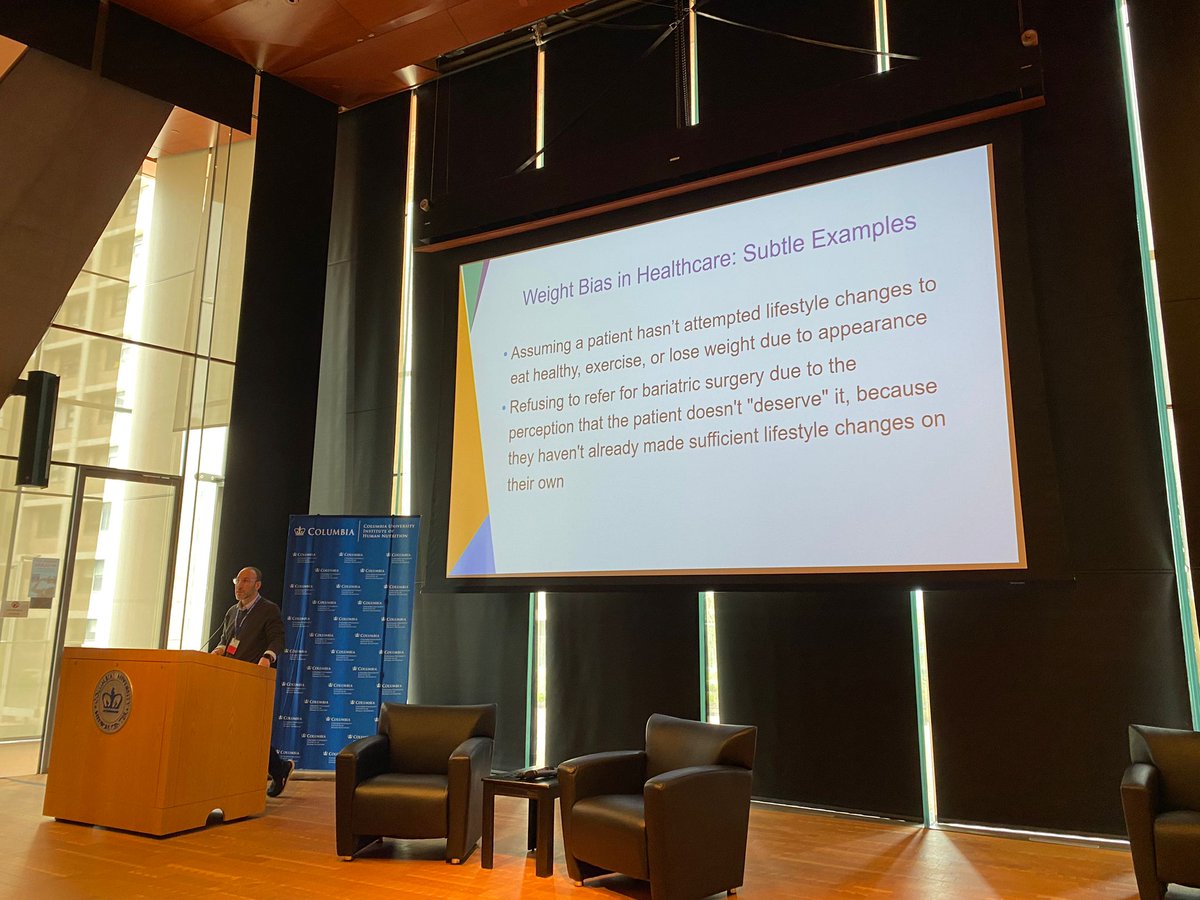

 Key quote:
Key quote:



 Satiation is the feeling of fullness WITHIN a meal while satiety is the feeling of fullness IN BETWEEN meals
Satiation is the feeling of fullness WITHIN a meal while satiety is the feeling of fullness IN BETWEEN meals