This #tweetorial is meant to complement the recent publication of the same name in @JHospMedicine
journalofhospitalmedicine.com/jhospmed/artic…
Let’s start with two questions...
First: Do you use prealbumin as a “marker” of malnutrition?
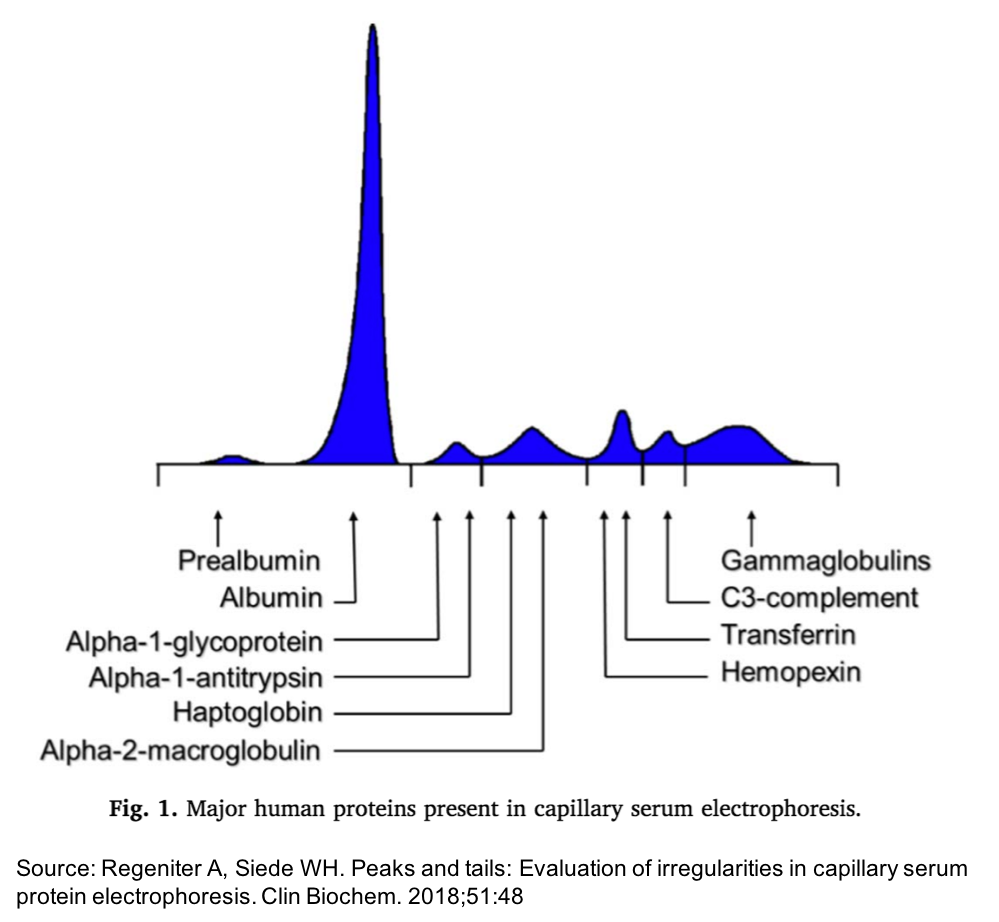
Second: How did prealbumin get its name?
[GE = gel electrophoresis]
Two reasons why you might think prealbumin offers value:
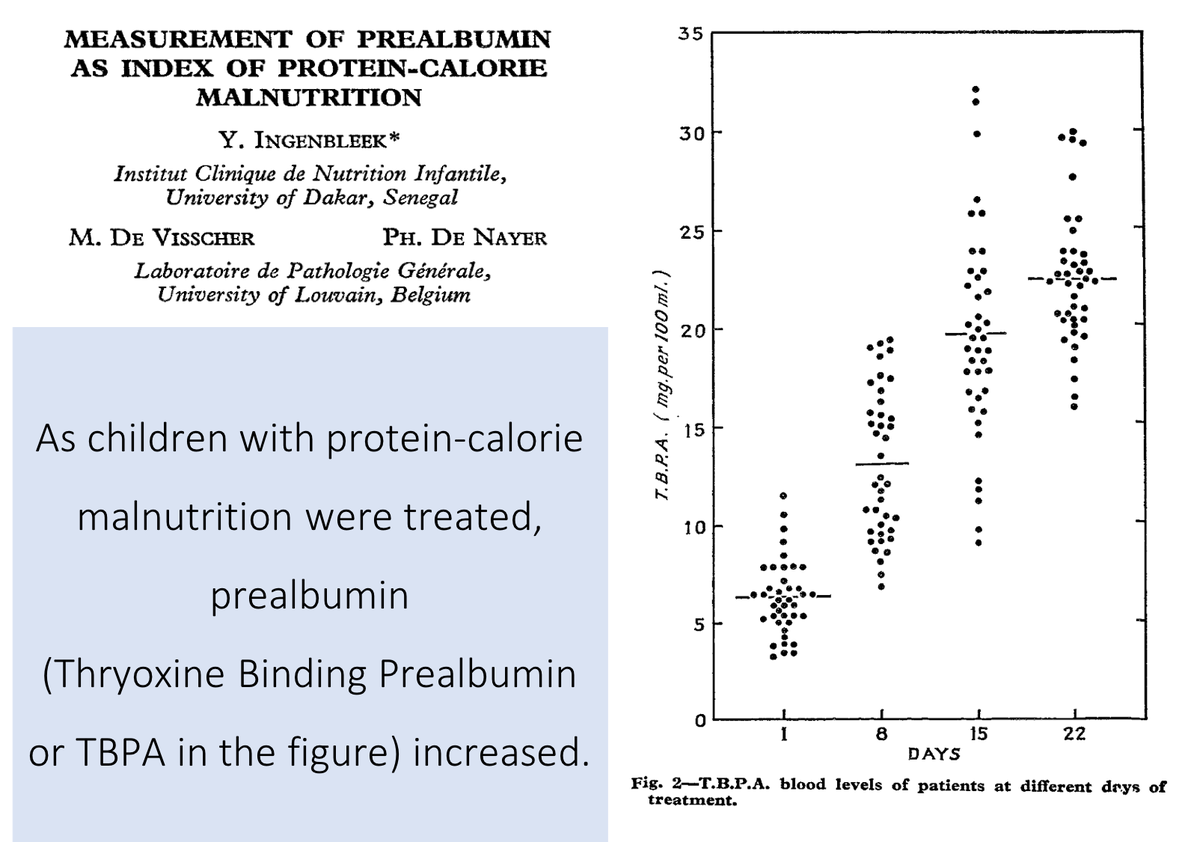
✔️it's shorter half-life (3d vs 3w for albumin) means it may reflect rapid changes in nutrition
✔️early studies of children with protein-calorie malnutrition suggested a correlation
ncbi.nlm.nih.gov/pubmed/4113892
But, as Lacy, Roesch, and Langsjoen discuss, recent literature suggests that prealbumin is:
✔️not sensitive/specific for malnutrition
✔️not always responsive to nutritional interventions
✔️not always correlated with health outcomes
For this thread, I'll discuss the first.
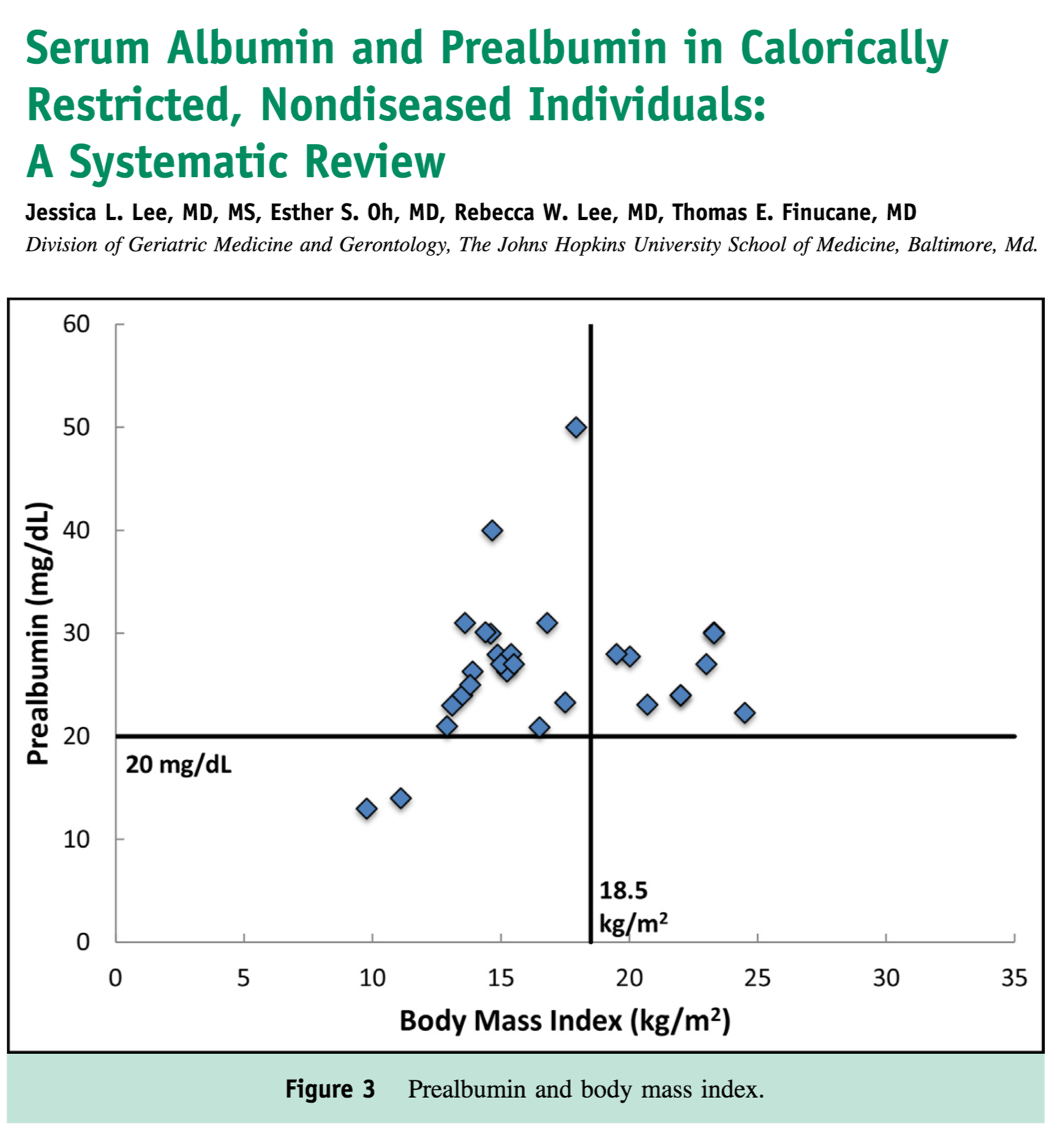
re: Sensitivity
As noted in a systematic review by Lee et al, in patients WITHOUT inflammatory conditions, prealbumin may be normal until one has severe malnutrition (e.g., the BMI falls below 12).
ncbi.nlm.nih.gov/pubmed/25912205
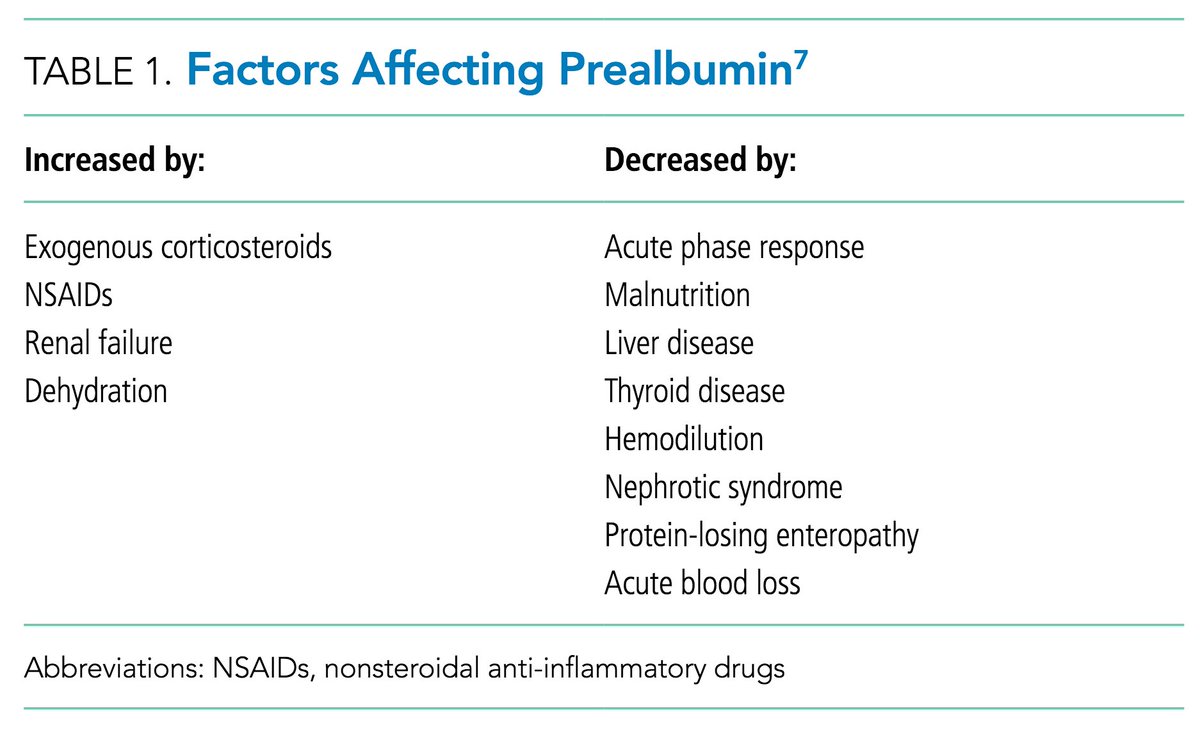
re: Specificity
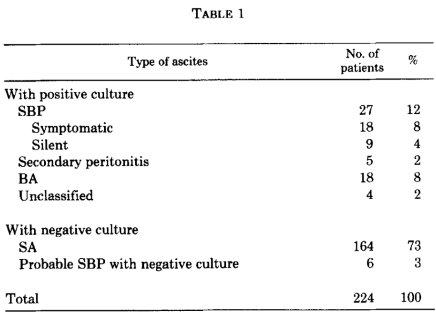
As shown in Table 1 of the #TWDFNR paper, there are many things (other than nutritional status) that affect prealbumin.
One key example: just like albumin, prealbumin is a negative acute phase reactant (i.e., it decreases in many inflammatory states).
Before closing, let's ask a version of one of the original question.
Do you use prealbumin as a “marker” of malnutrition?
To summarize, though many of us have used prealbumin (transthyretin!) as a marker of nutritional status, it fails on many counts. As a result, it is a #TWDFNR.
For more information, have a look at the recent paper published in @JHospMedicine
journalofhospitalmedicine.com/jhospmed/artic…