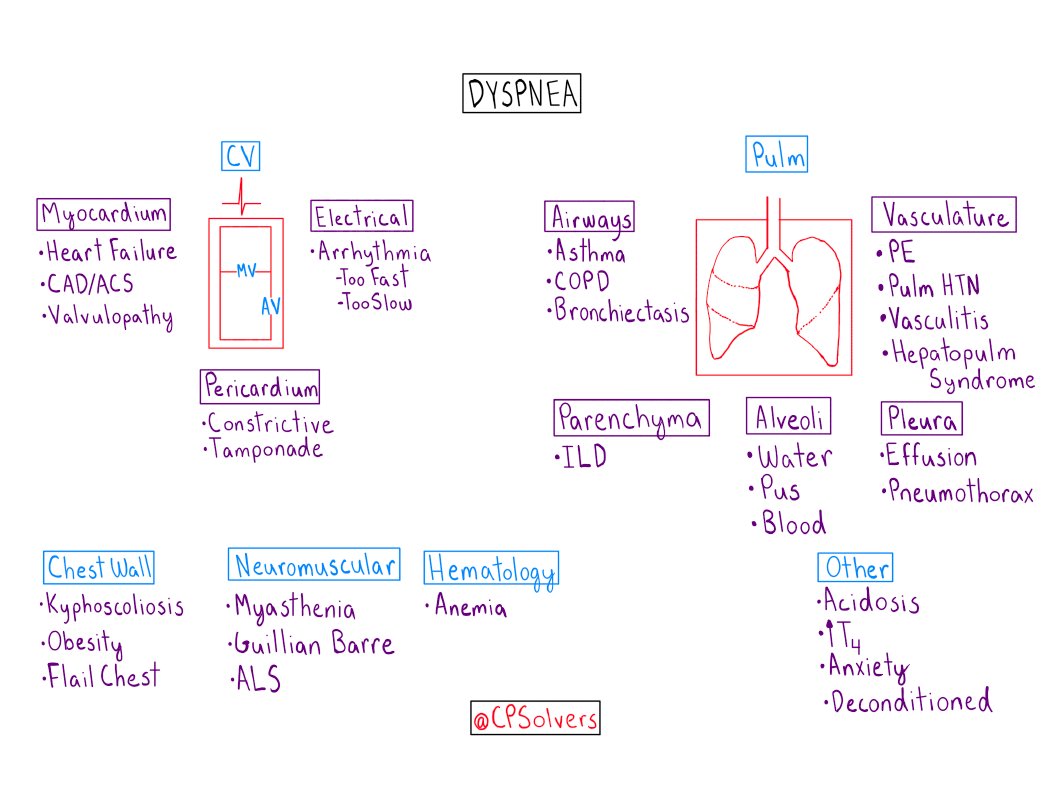
67F w/ HTN, HFpEF & RA (on chronic prednisone & PCP PPx) p/w 3 days of progressive dyspnea, malaise & productive cough.
Epidemiology (e.g. the base rate of PNA), background info (e.g. HFpEF & ongoing immunosuppression), and lack of obvious risk factors for DVT/PE may also shift HF and PNA higher in your mind.
She has⬆️work of breathing. JVP is not visible while sitting up at 45 deg. No S3 or S4. Coarse crackles are present in the bilateral, middle lung fields. She has no lower extremity edema.
CXR is shown below (Image courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 17327)

Please share your reasoning with us by replying to this tweet in addition to answering below!
It can be extremely difficult to tease out PNA from HF. Often, the exam, CXR, and BNP help make the dx.
She has many findings that point against HF as the cause of her dyspnea.
Which one(s) made the biggest difference for you?
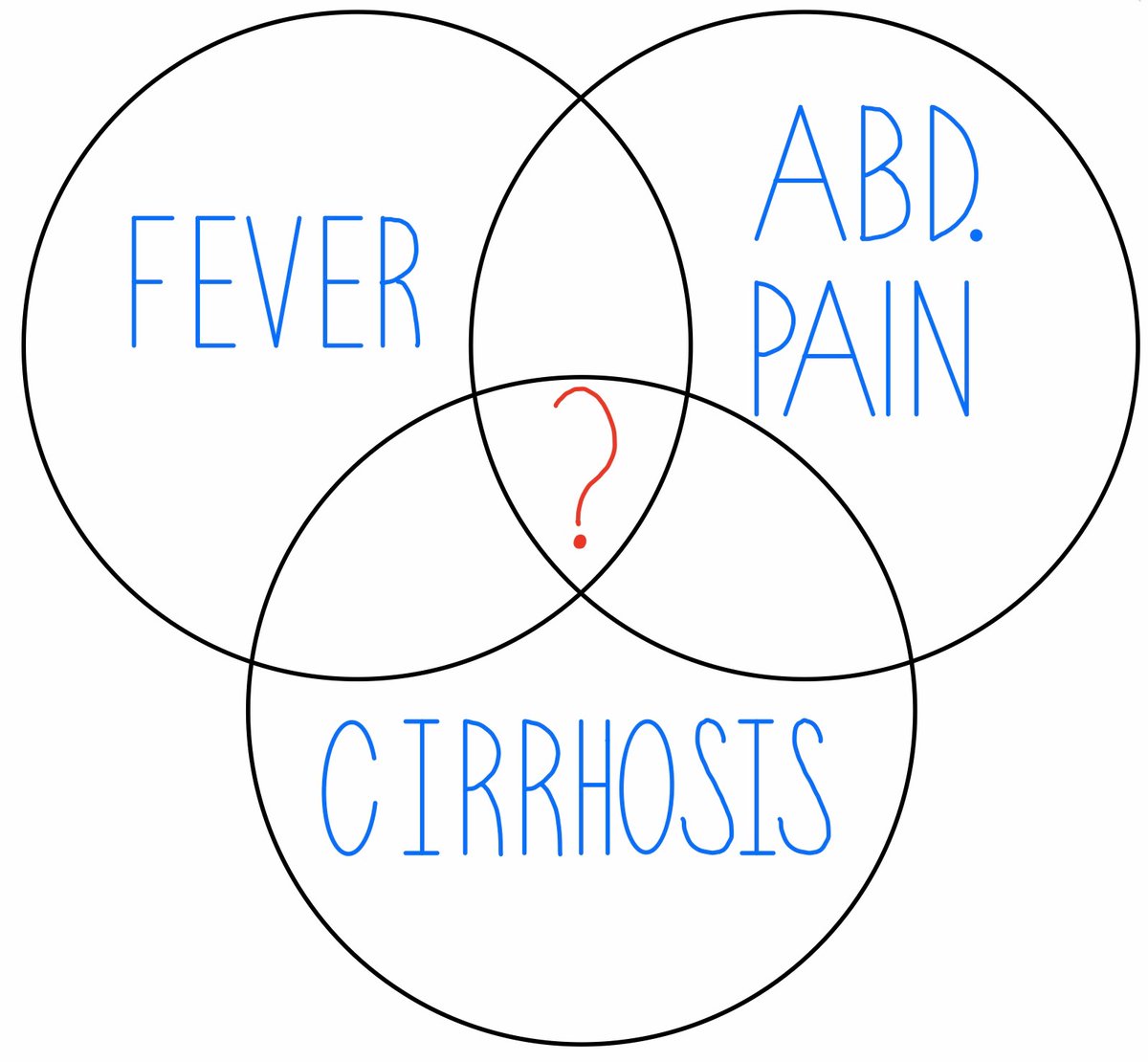
An acute pulmonary infection (e.g. community acquired pneumonia) is a very common cause of that clinical syndrome.
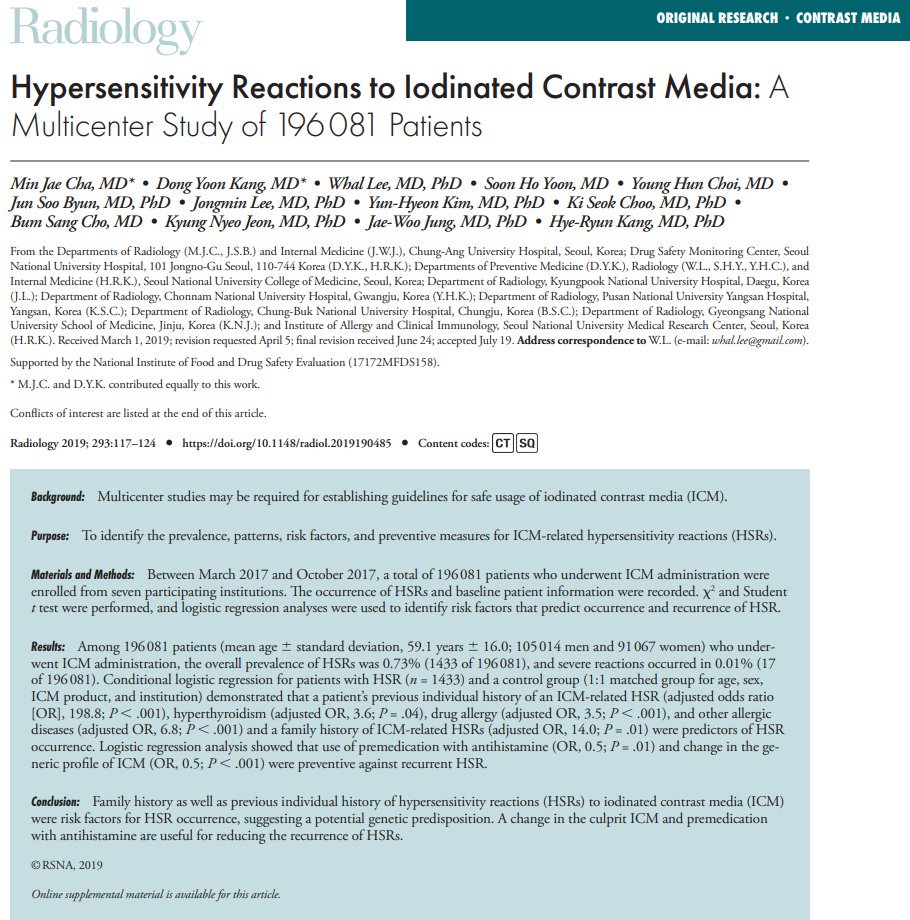
There are many unquantifiable factors in this case (e.g., the appearance of the consolidations on CXR, the fact that she is on chronic prednisone) that change the way we weigh diagnostic probabilities.
Thank you for reasoning with us, and be sure to check out @jackpenner’s article to review and reinforce these concepts! bit.ly/2Stzh1e