2/
The crisis is the #PPE shortage that many U.S. medical centers face
(due to abject failure of federal leadership).
3/
I am following @CDC and @WHO. We docs lecture #antivaxxers and other purveyors of snake oil saying “believe the experts”... well, CDC & WHO are the experts.
5/
6/
A systematic review “Infection Prevention in the Emergency Department” w/ Dr. Stephen Liang
7/
ncbi.nlm.nih.gov/pmc/articles/P…
8/
9/
11/
13/
14/
March 16 @AnnalsofIM “COVID-19 & Risk to Health Care Workers: A Case Report”
15/
annals.org/aim/fullarticl…
16/
“All 41 health care workers were placed under home isolation for 2 weeks, with daily monitoring for [Sx]. In addition, they had NP swabs scheduled on day 1 of home isolation, & 2nd swab on day 14 after exposure.”
17/
“NONE of the exposed health care workers developed symptoms, and all PCR tests were negative
18/
??? remain
20/
March 17, @NEJM letter “Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1”
This was NOT a clinic study. It was an experiment in a lab.
21/
nejm.org/doi/full/10.10…
22/
??? remain
24/
25/
March 26, “Transmission Potential of SARS-CoV-2 in Viral Shedding Observed at the University of Nebraska Medical Center”
NOTE: ***pre-print = no peer review, meaning anything besides methods is sorta like this thread***
26/
medrxiv.org/content/10.110…
…let’s dig deeper
27/
For airborne transmission they collected “high volume air samples, and low volume personal air samples”
What about infectivity? They did cell-culture
28/
29/
“Taken together, these data indicate significant environmental contamination in rooms where patients infected w SARS-CoV-2 are housed & cared for, regardless of the degree of symptoms or acuity of illness.”
need cleaning & HH!
31/
The 2 studies suggesting airborne transmission showed RNA particles can be amplified from air, but didn't infect live cells or humans.
Verdict: not enough evidence=uncertainty
32/
@AtulGawande wrote an article “Keeping the Coronavirus from Infecting Health-Care Workers: What Singapore’s and Hong Kong’s success is teaching us about the pandemic” in which he reviewed the infection prevention practices in Singapore & HK.
key passage:
33/
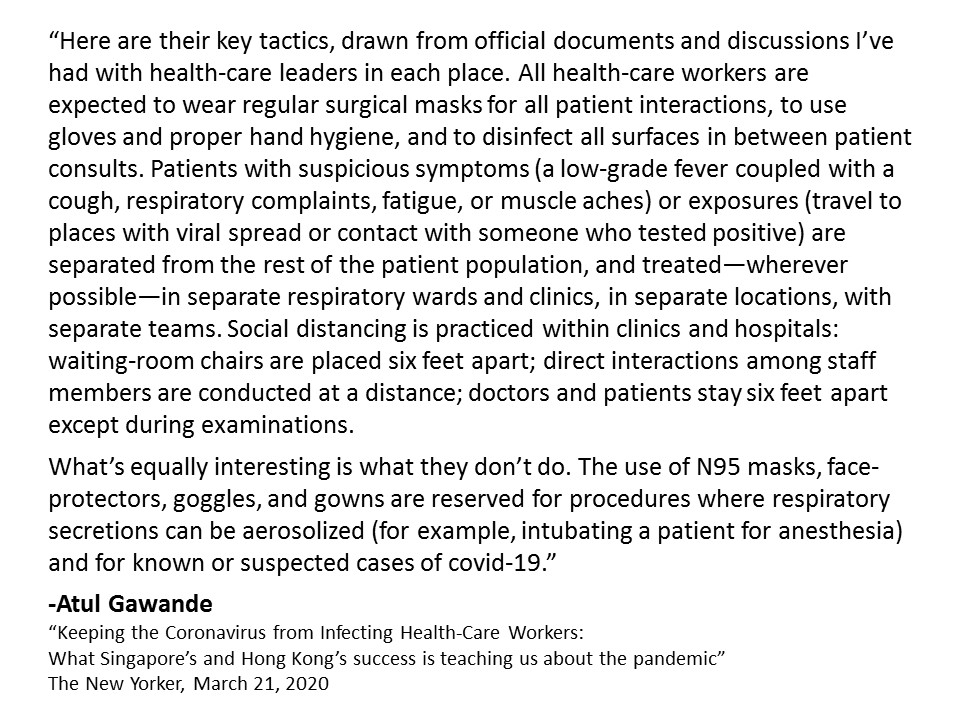
Why so important? Bc in U.S. we are conserving N95 masks, so WE DON”T RUN OUT.
34/
35/
37/
GREAT QUOTE! HCW psychology key
but what N95 shortage?
38/
39/
We want someone to blame.
There are people to blame --the federal leaders who did not do their jobs preparing our country, and delayed us locally in doing ours.
40/
So we are now left to choose between Bad option A and Bad option B. (HT @GovRaimondo)
#getusPPE
41/
When me get more masks, I will re-examine.
end/
good short article about what to do if you face N95 article
"This One Is for the Health Workers at the Front Lines"