
1) Welcome to an #accredited #tweetorial on a unique emerging (in Ph3 now) option for specifically reversing the #antiplatelet effects of #ticagrelor: it's #bentracimab. Expert faculty is antithrombotic agent reversal guru @md_pollack of @UMMCnews, working to create #AHealthierMS
2) This program is intended for #healthcare professionals and is supported by an educational grant from PhaseBio Pharmaceuticals. Faculty disclosures are listed at cardiometabolic-ce.com/disclosures/, and prior programs are available for 🆓CE/#CME credit at cardiometabolic-ce.com.
3) It is an unfortunate fact of life that one cannot prescribe #anticoagulant or #antiplatelet (together, #antithrombotic) therapy without increasing a patient's #bleedingrisk. That is why it should be an individualized risk:benefit decision, ideally . . . 
4) . . . as part of a #shared decisionmaking process with the patient/caregivers, when initiating therapy. For most patients--those without a baseline ⬆️bleeding risk--the use of #aspirin & a #P2Y12i in a patient with severe #CAD, or who has received a coronary stent, or who ... 
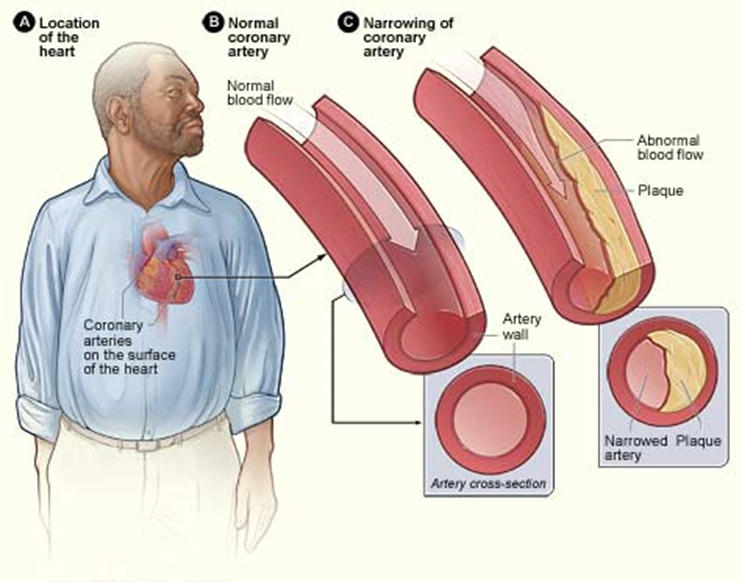
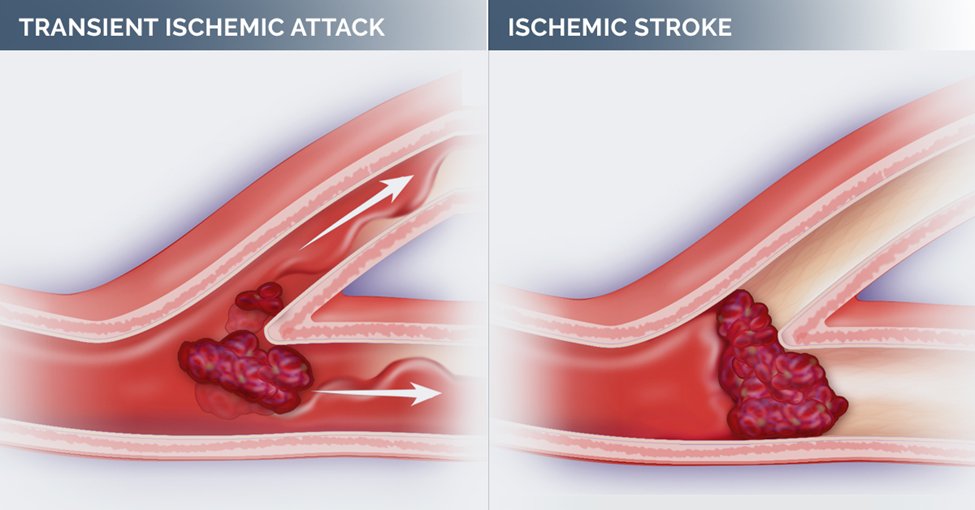
5) ... has just had an ischemic #stroke or #TIA, is likely to offset in atherothrombotic events whatever elevated bleeding risk might accrue due to therapy. 
6) Similarly, most patients with #atrialfibrillation derive a net clinical benefit from well-controlled anticoagulation in terms of ⬇️thromboembolic stroke and systemic embolism compared to elevated bleed risk. 

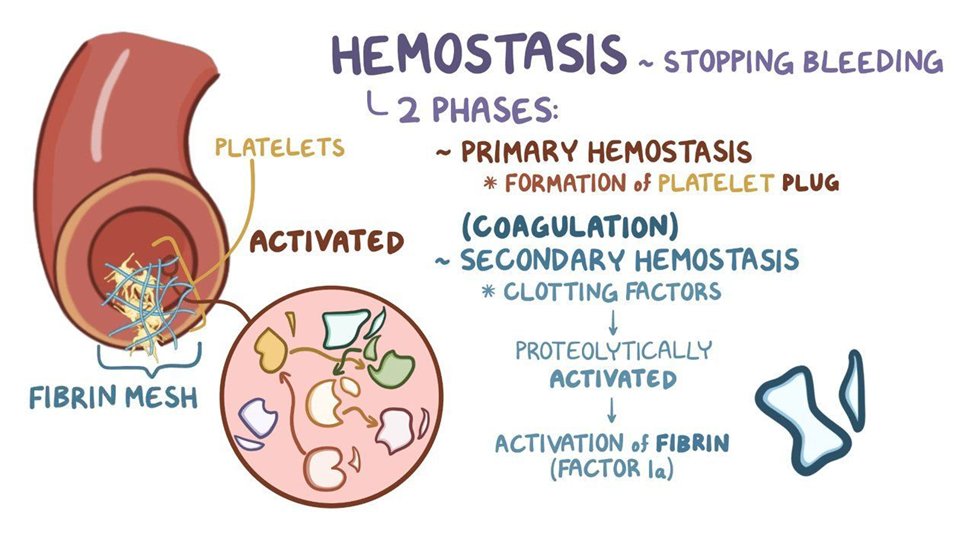
7) All the same, bleeding events, which can be major or life-threatening, do sometimes occur in patients taking antithrombotic meds. When that happens, the iatrogenic obstacles to abnormal thrombosis that were Rx'd now become iatrogenic obstacles to achieving normal #hemostasis. 
8) Similarly, patients taking #antithrombotics sometimes require urgent or emergent surgery or other invasive procedures, which may be substantially more risky in the face of impaired hemostasis as compared to a patient NOT taking antithrombotics.
9) The same reasoning applies to pts w/traumatic injuries, whose speed & volume of blood loss may be ⬆️⬆️when a patient has iatrogenically impaired hemostasis, no matter how sound the reasoning that prevention/treatment of pathologic thrombosis/atherothrombosis was indicated.
10) BTW, which of the following agents is NOT an immediate reversal strategy for an antithrombotic agent?
11) It must always keep in🧠that vitamin K is NOT an emergency reversal strategy for warfarin-related hemorrhage . . . it only helps initiate the manufacture of 🆕vitamin-K dependent clotting factors.
12) For reversal of #dabigatran in the hemorrhaging patient, we have #idarucizumab. See 🔓nejm.org/doi/full/10.10… for the full Ph 3 supporting data. 
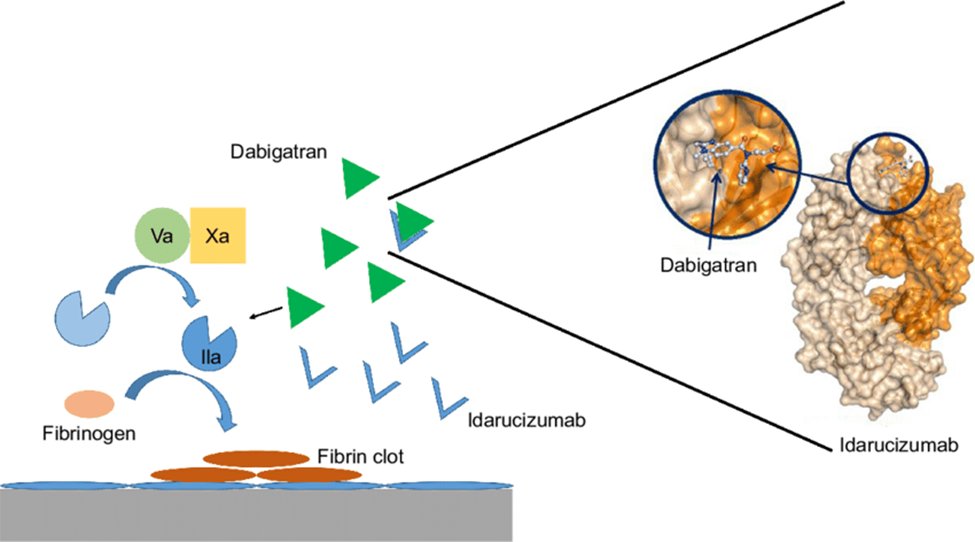
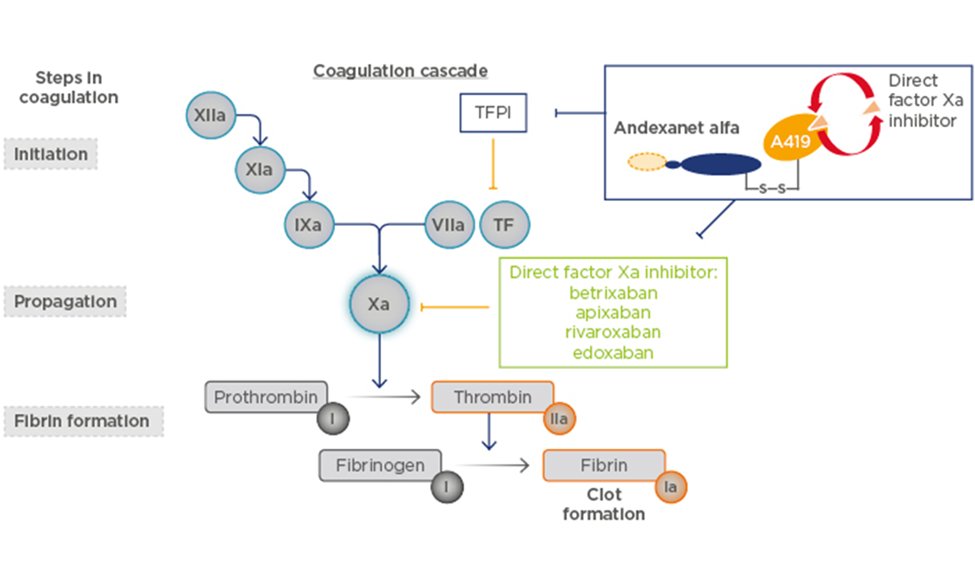
13) Meanwhile, for reversal of anti-#FXa #DOACs (#apixaban & #rivaroxaban per label) in the hemorrhaging patient, we have #andexanate alfa. See primary data at 🔓nejm.org/doi/full/10.10…. Though off-label, there is also anecdotal use of 4F-#PCC to reverse DOACs. 
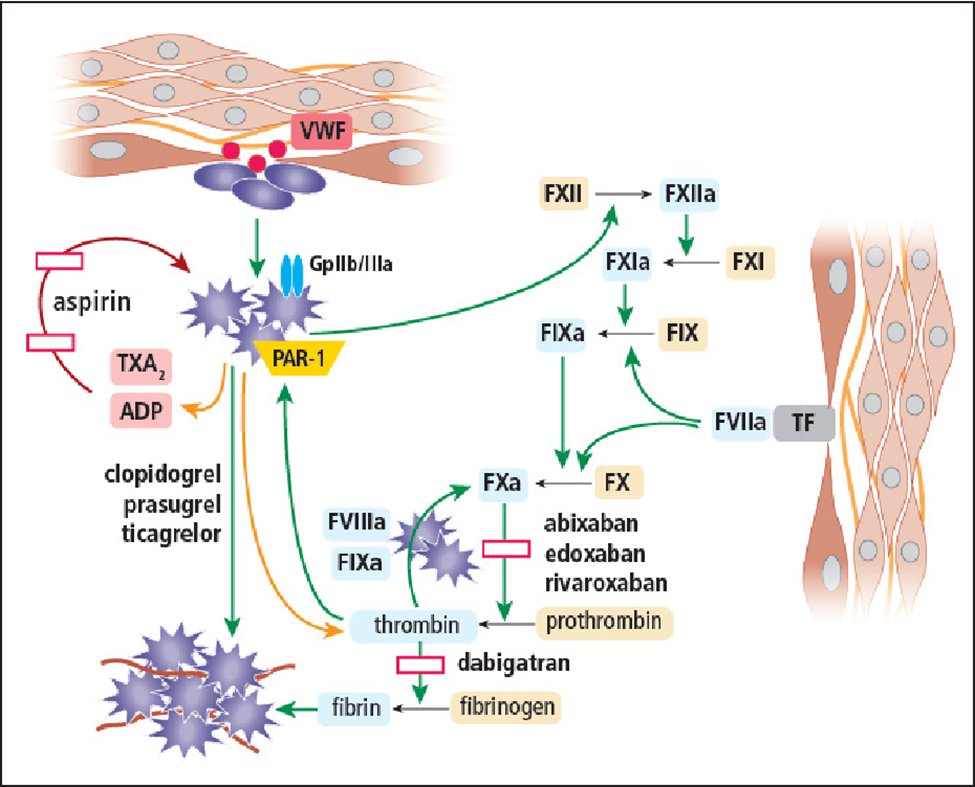
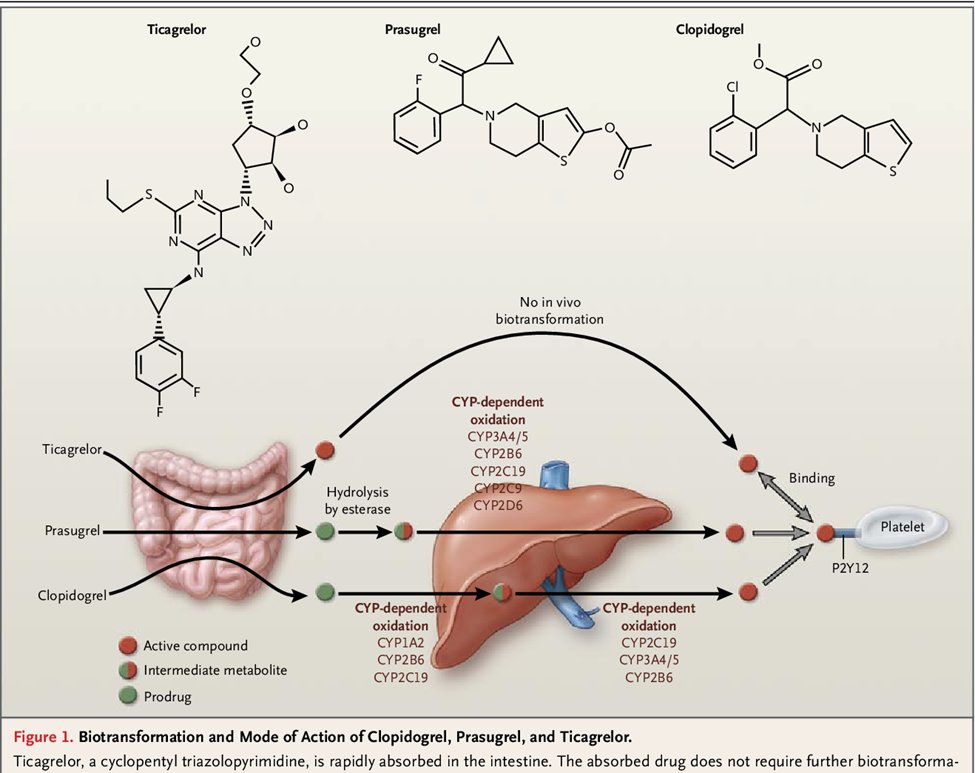
14) But what about antiplatelets? The antiplatelet effects of #aspirin, #clopidogrel, & #prasugrel can all be largely overcome by #platelet #transfusions. This is because their inhibitory effects are permanent for the platelets on which they act.
15) Giving more platelets means that the antiplatelet effect can be overwhelmed and the platelet contribution to hemostasis can be restored despite there being an antiplatelet medication on board. It's different for #ticagrelor, which unlike prasugrel & clopidogrel is not . .
16) . . . a #thienopyridine (for you chemistry geeks out there, it's a cyclopentyl-#triazolopyrimidine) &, more importantly, is a #reversible #Platelet inhibitor. This means that administering exogenous platelets is not very effective, because the inhibitor can "jump off" ...
17) ... the patient's platelets and "jump on" the transfused platelets, meaning much of the inhibition of "normal" hemostatic platelet function persists. Therefore, unlike the other #P2Y12i's, a specific reversal strategy is needed for #ticagrelor. 
18) So why might this be so important?
-- ticagrelor is a potent antiplatelet. This is always a doubled-edged ⚔️. More potency ➡️more effective at preventing unwanted #thrombosis, but also more likely to be assoc'd with ⬆️#bleedingrisk.
-- use of ticagrelor is ⬆️ing 🌎🌍🌏
-- ticagrelor is a potent antiplatelet. This is always a doubled-edged ⚔️. More potency ➡️more effective at preventing unwanted #thrombosis, but also more likely to be assoc'd with ⬆️#bleedingrisk.
-- use of ticagrelor is ⬆️ing 🌎🌍🌏
19)
-- patients Rx'd #ticagrelor are older & have more comorbidities, many of which are already assoc'd with ⬆️#bleedingrisk.
-- older patients are more active 👟than ever, ➡️risk of injury that may produce bleeding.
-- older patients are more likely to need urgent surgery
-- patients Rx'd #ticagrelor are older & have more comorbidities, many of which are already assoc'd with ⬆️#bleedingrisk.
-- older patients are more active 👟than ever, ➡️risk of injury that may produce bleeding.
-- older patients are more likely to need urgent surgery
20) And there's the special case of 🫀surgery. The #prescribinginformation for all 3⃣ #P2Y12i's recommends delaying surgery for up to 5-7 days for pts taking these drugs to allow their #antiplatelet activity to decay naturally. But is a patient w/#CAD is loaded with one of ... 

21) ... these drugs in or before going to #coronarycath, and THEN it's discovered that #CABG is needed, or if there is a complication requiring immediate surgery such as #coronary artery #dissection, what do you do? You give #platelets--but in the case of #ticagrelor, that's ...
22) ... not so helpful. What about an intracranial hemorrhage #ICH in a patient taking ticagrelor? We have to be concerned that impaired platelet activity will contribute to #hematoma expansion. And that pt from the freeway crash with blunt thoracic injury & internal hemorrhage? 

23) And that patient with the massive #GIbleed?
In all of these cases, there is a need for a reliable means of restoring platelet activity to support hemostasis while the treating clinicians do what they can to prevent or staunch bleeding.
In all of these cases, there is a need for a reliable means of restoring platelet activity to support hemostasis while the treating clinicians do what they can to prevent or staunch bleeding.
24) So what is needed is a SPECIFIC #reversal strategy for the #antiplatelet effects of #ticagrelor. Being developed for that very reason is #bentracimab, a #monoclonal #antibody #Fab fragment directed at ticagrelor and its active metabolite #TAM.
25) BTW, you can learn about Fab strategies and earn more🆓CE/#CME credit at cardiometabolic-ce.com/pharmacology1/, also from @md_pollack. It's a remarkable approach to specific neutralization of a drug, because a well-designed Fab has no off-target biological activity.
26) We'll focus on that tomorrow. Please COME BACK and complete this program so you can earn your 🆓CE/#CME! #FOAMed #CardioTwitter @DLBHATTMD @ToddVillinesMD @gabrielsteg @SnayCardsPharmD @beaverspharmd @DrMauricioCohen @GoggleDocs @mirvatalasnag @aayshacader @CardioNerds
27) Welcome back! We're talking about #reversal agents for #antithrombotics and are about to shine a 🔦on an investigational agent that appears to reverse the #antiplatelet effects of #ticagrelor, while you earn CE/#CME! I am @md_pollack.👏to @CMichaelGibson @cpcannon
28) So, about bentracimab: Formerly known both as #PB2452 & #MEDI2452, the artist now known as #bentracimab is a neutralizing monoclonal antibody fragment that binds ticagrelor & TAM with high affinity. The mechanism of action is shown in this cartoon: 
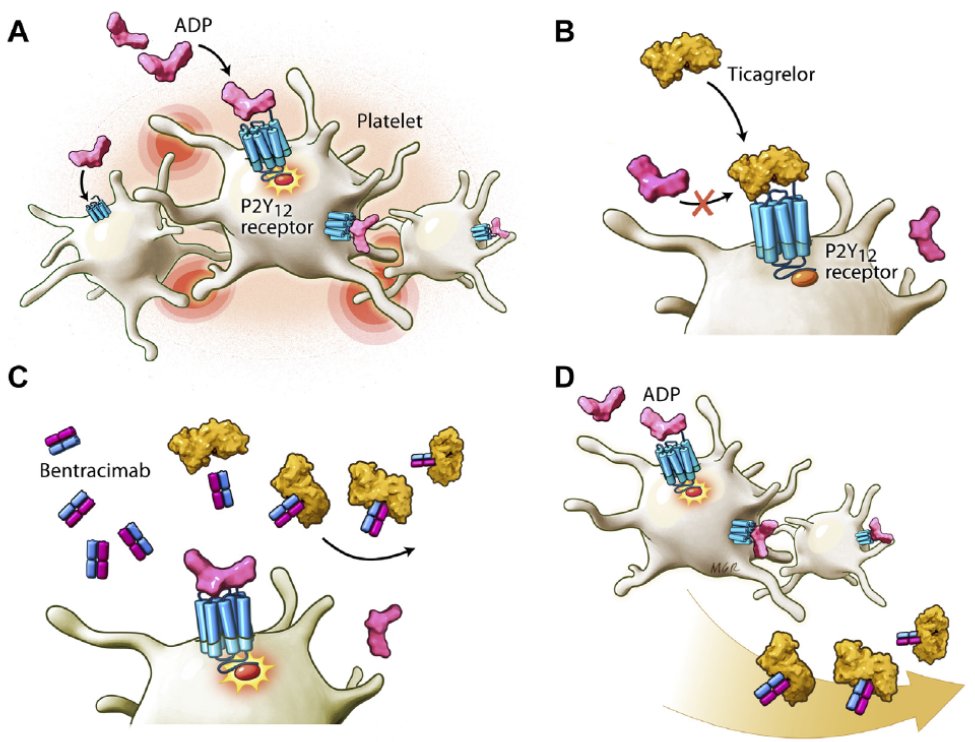
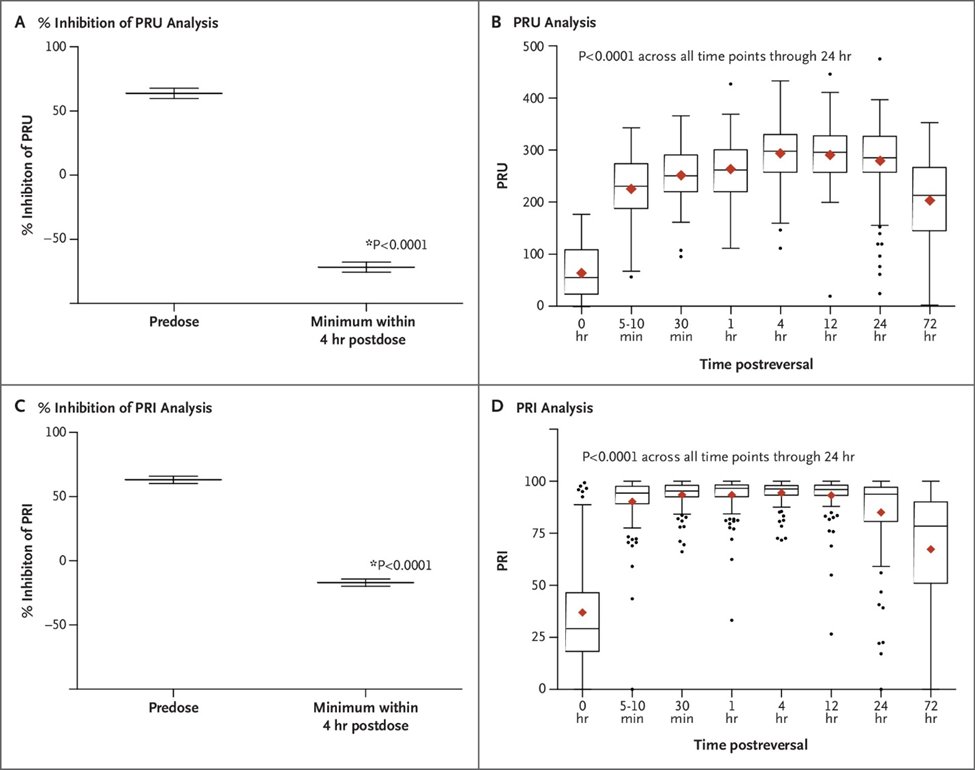
29) A Phase 1 study 🔓nejm.org/doi/full/10.10… showed several important points:
-- PB2452 via initial IV bolus followed by a prolonged infusion (8, 12, or 16h) was associated w/a significantly greater increase in platelet function than placebo, per multiple assays. (EFFECTIVE)

-- PB2452 via initial IV bolus followed by a prolonged infusion (8, 12, or 16h) was associated w/a significantly greater increase in platelet function than placebo, per multiple assays. (EFFECTIVE)

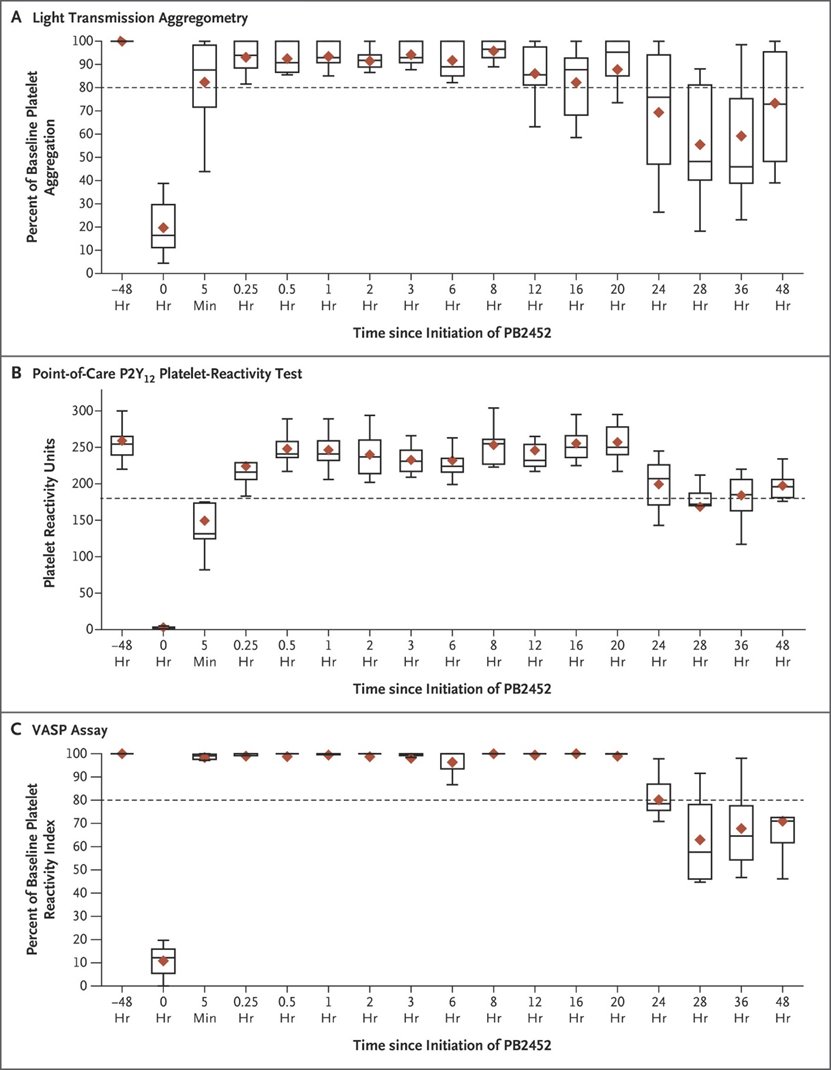
30)
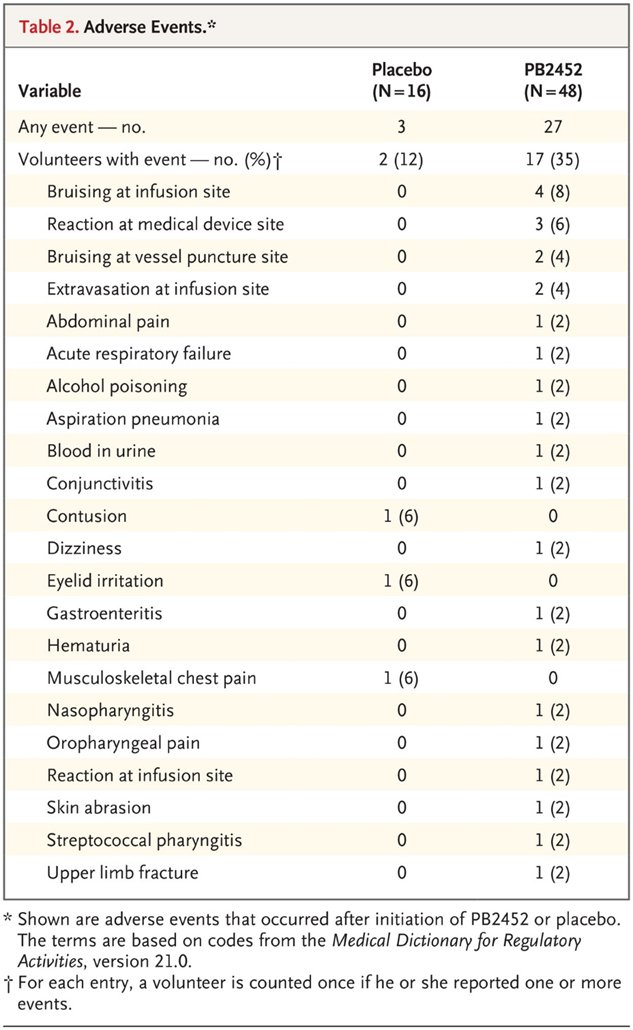
-- Ticagrelor reversal occurred within 5 minutes after the initiation of #bentracimab (RAPID) . . .
-- and was sustained for more than 20 hours (DURABLE, PREDICTABLE).
-- Adverse events were limited mainly to issues involving the infusion site (SAFE x1)
-- Ticagrelor reversal occurred within 5 minutes after the initiation of #bentracimab (RAPID) . . .
-- and was sustained for more than 20 hours (DURABLE, PREDICTABLE).
-- Adverse events were limited mainly to issues involving the infusion site (SAFE x1)
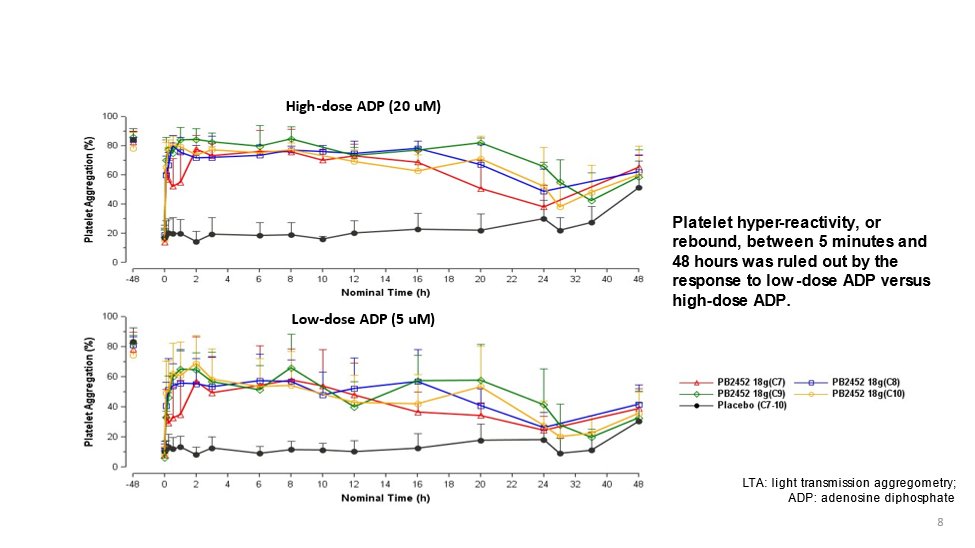
31) There was no evidence of a rebound in platelet activity after drug cessation (SAFE x2). Now that's 🔑because there is always the concern for the thrombotic events for which the ANTIthrombotic drug was being given to prevent might occur after reversal.
32) Such events would not be an unexpected sequala. Pts are prescribed ticagrelor in response to the evaluation that they are at increased risk of acute atherothrombotic disease (MI or stroke). These are high-risk outcomes & represent the benefit of ...
33) ... ticagrelor’s potent inhibition of platelet activation, which is required for platelet aggregation & thrombosis. Thrombotic events that occur after sudden and complete removal of antithrombotic protection reflect either: (cont⤵️)
34) a #prothrombotic effect of the reversal strategy,
or
the “unmasking” or “disinhibition” of the patient’s abnormal thrombophilic pathology
or
the “unmasking” or “disinhibition” of the patient’s abnormal thrombophilic pathology
35) So as per the graphs below, platelet hyper-reactivity, or rebound, between 5 minutes & 48 hours after administration of #bentracimab was ruled out by the response to low-dose #ADP versus high-dose ADP. Thanks @DLBHATTMD 
36) Reassuring . . . but these are Ph 1 data from healthy volunteers. So it'd be great to know that the drug works as well, is as safe, and isn't prothrombotic in real patients being reversed for bleeding or prior to an invasive procedure.
37) Enter the ongoing Ph 3 REVERSE-IT study. You can learn all about that study from @DLBHATTMD & @md_pollack and earn even more🆓CE/#CME by viewing the program at academiccme.com/courses/platel….
38) Per @US_FDA labeling, ticagrelor should be interrupted how many days prior to surgery that has a major risk of bleeding? Answer before you scroll ⤵️!
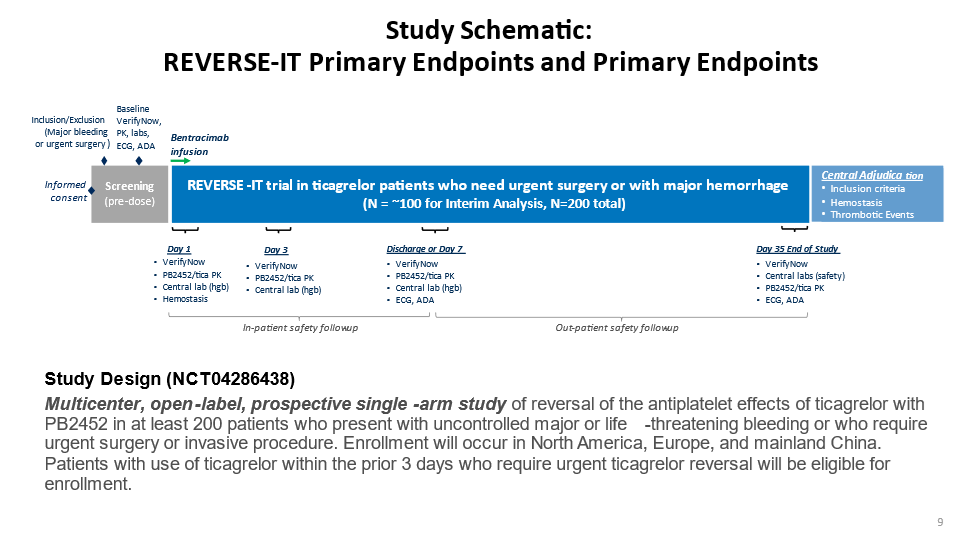
39) It's 5 days--part of the rationale for the REVERSE-IT study (clinicaltrials.gov/ct2/show/NCT04…) to enroll both hemorrhaging and pre-procedural pts who are on ticagrelor and per the opinion of the treating clinician 🤔would benefit from reversal and restoration of platelet function. 
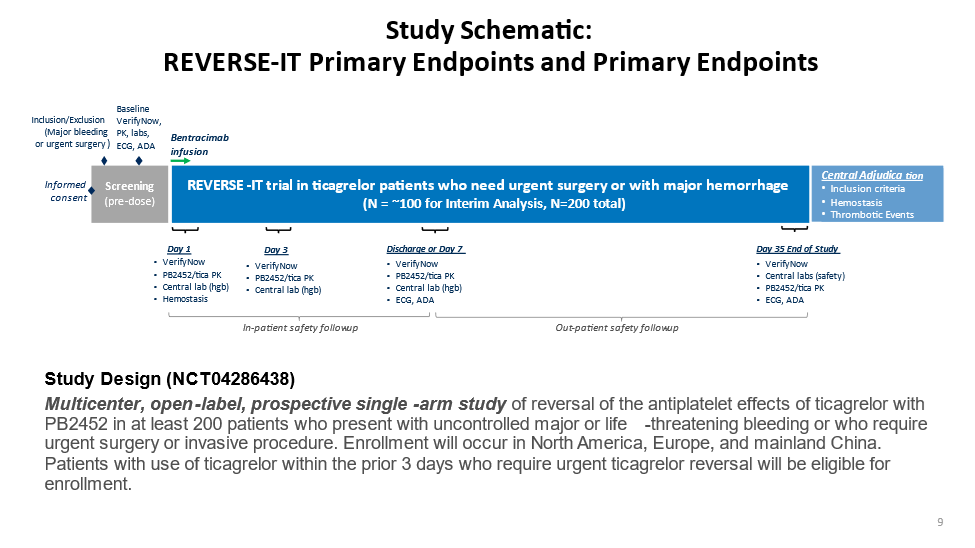
40) In the case of bleeding, the clinician must feel that conventional bleeding mgt is unlikely to be successful with impaired platelets. In the case of an urgent/emergent need for an invasive procedure, the clinician must feel that . . .
41) . . . the procedure would likely be unsafe for the patient either (a) if it proceeds with impaired platelets or (b) is delayed until the effect of ticagrelor "naturally" decays.
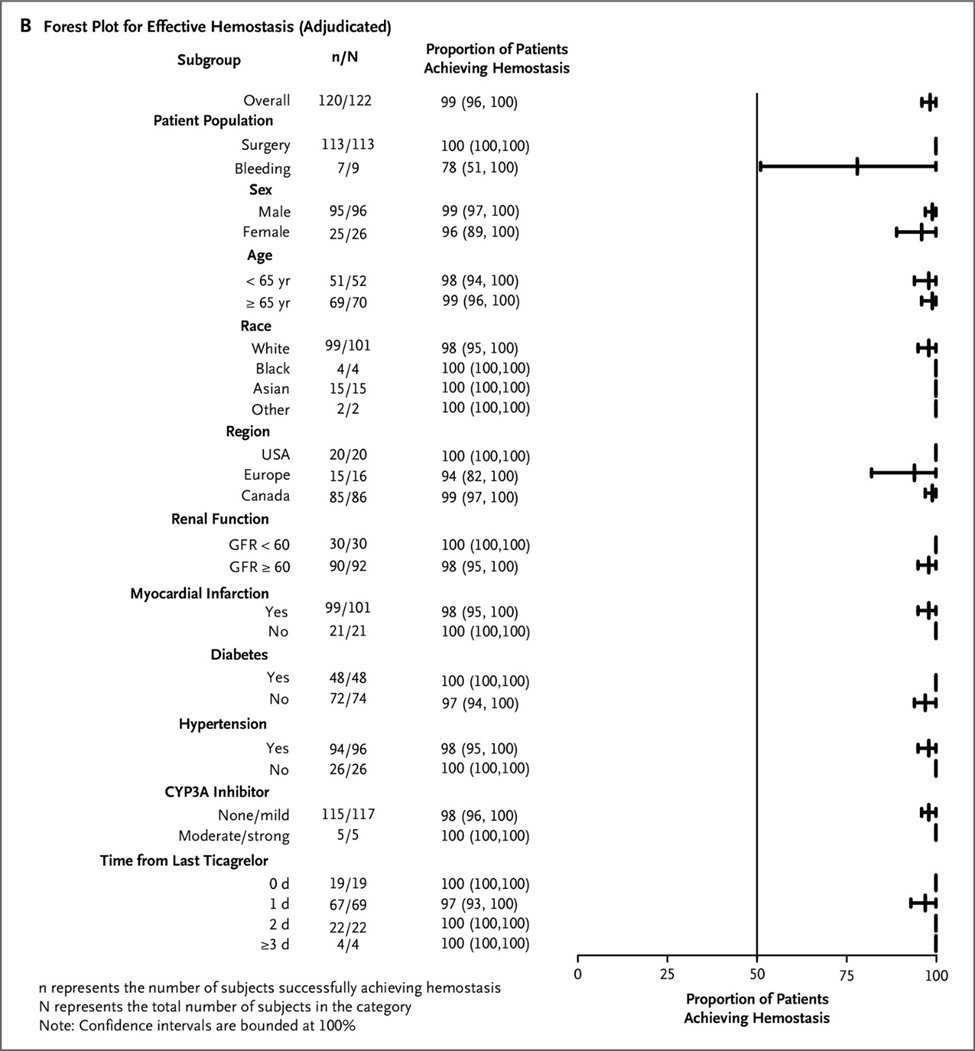
42) And exciting news came out of the #LBCT session of #AHA21 where @DLBHATTMD shared the interim analysis of REVERSE-IT, including data from 150 patients: 8 with hemorrhage and 142 pre-procedural (the majority of the latter being pre-#CABG). 
43) The interim Ph 3 data on the drug's activity in these at-risk patients closely paralleled the Ph 1 experience (published 🔓evidence.nejm.org/doi/full/10.10…): 



44) Safety events were again largely limited to infusion site reaction and the incidence of post-reversal #thrombotic #thromboembolic events was quite small, with NONE of these events attributed to any prothrombotic effect of #bentracimab by the independent #DSMB: 
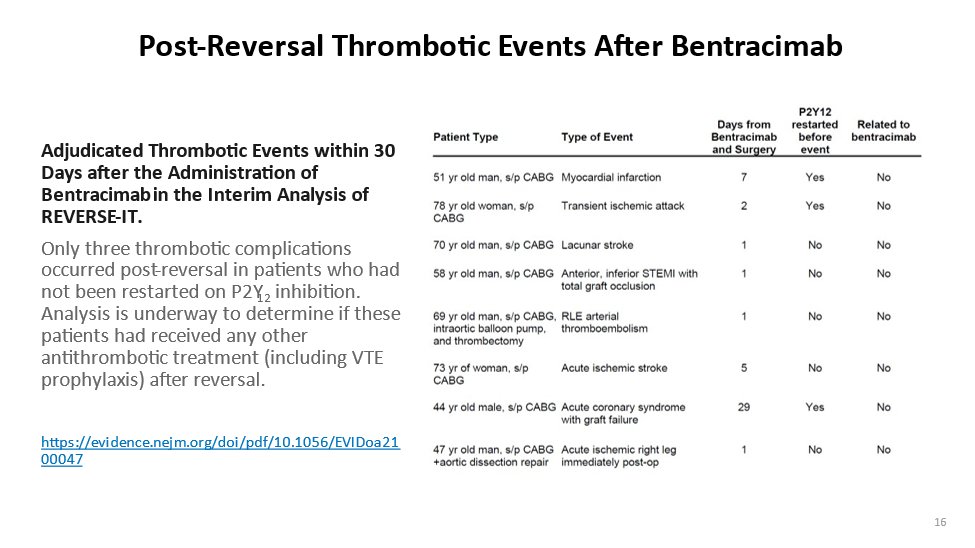
45) How could the DSMB been so confident? Well, they relied on the Ph 1 data on the high-vs-low-dose #ADP exposure that showed no platelet hyperreactivity (tweet 33). But even more compelling, they now had interim Ph 3 data, which indicated . . .
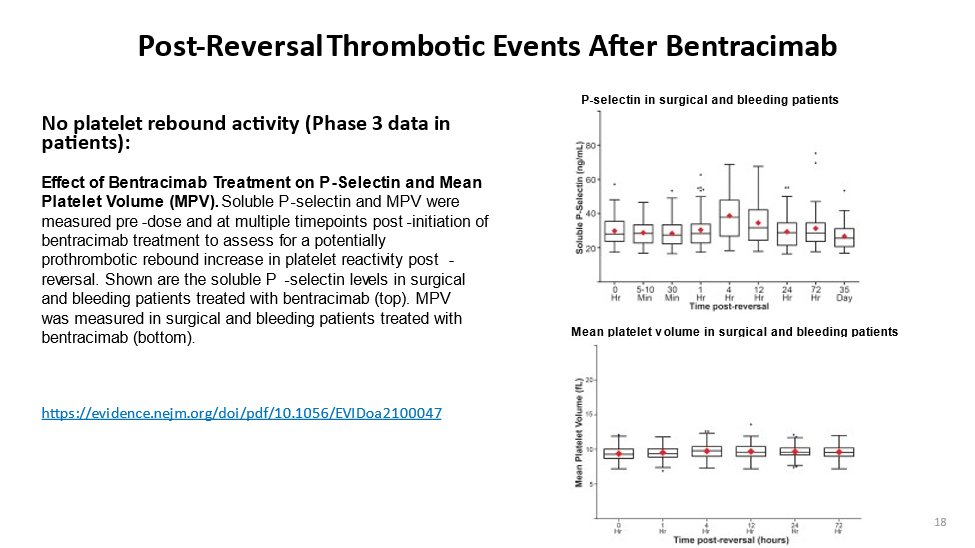
46) . . . that both #Pselectin levels and mean platelet volume (#MPV) assays indicated no evidence of ⬆️platelet activity or "sensitivity" after reversal: 
47) The Ph 3 REVERSE-IT study continues, w/exclusive focus now on enrolling pts in the hemorrhage arm. The conclusion of the interim analysis: Bentracimab provided immediate, safe, sustained reversal of the antiplatelet effects of ticagrelor in pts undergoing surgical procedures
48) The biggest potential impacts of those data on this still-investigational drug?
-- make the "neutralization" process to restore platelet function a consistent approach
-- shave days off hospitalization currently spent supporting pts while ticagrelor's effects "wear off"
-- make the "neutralization" process to restore platelet function a consistent approach
-- shave days off hospitalization currently spent supporting pts while ticagrelor's effects "wear off"
49) Time will tell. Still, this is an exciting development that extends the "reversal" strategy to yet another antithrombotic agent, which is key to future practice, given the aging of the population and⬆️use of antithrombotic strategies. Make 'em safer!
50) And there you have it! You just earned 0.5h CE/#CME for #physicians #physicianassociate #nurses #nursepractitioners #pharmacists. Go claim it at cardiometabolic-ce.com/antithrombotic…. And follow us on @cardiomet_ce and @ckd_ce for more 🆓programs from expert authors. This is @md_pollack!
51) Please click that FOLLOW button, just as have @ProfKausikRay @DBelardoMD @dr_benoy_n_shah @GoggleDocs @ferbottero @stephanamayer @michellebr00ks @SVRaoMD @KardiologieHH @sbrugaletta @HarryDauerman @Lross246 @mmamas1973 @SABOURETCardio @SantosGallegoMD @ErinMichos @hvanspall
• • •
Missing some Tweet in this thread? You can try to
force a refresh









