Should I consider atrial fibrillation a risk factor for pulmonary embolism?
If the right atrium is fibrillating, can’t thrombus form? And if it does, can’t it migrate to the pulmonary vasculature, leading to a pulmonary embolism?
Let's examine these questions...
We’ll start with a couple questions.
Q1: Do YOU currently consider atrial fibrillation (AF) to be a risk factor for pulmonary embolism (PE)?
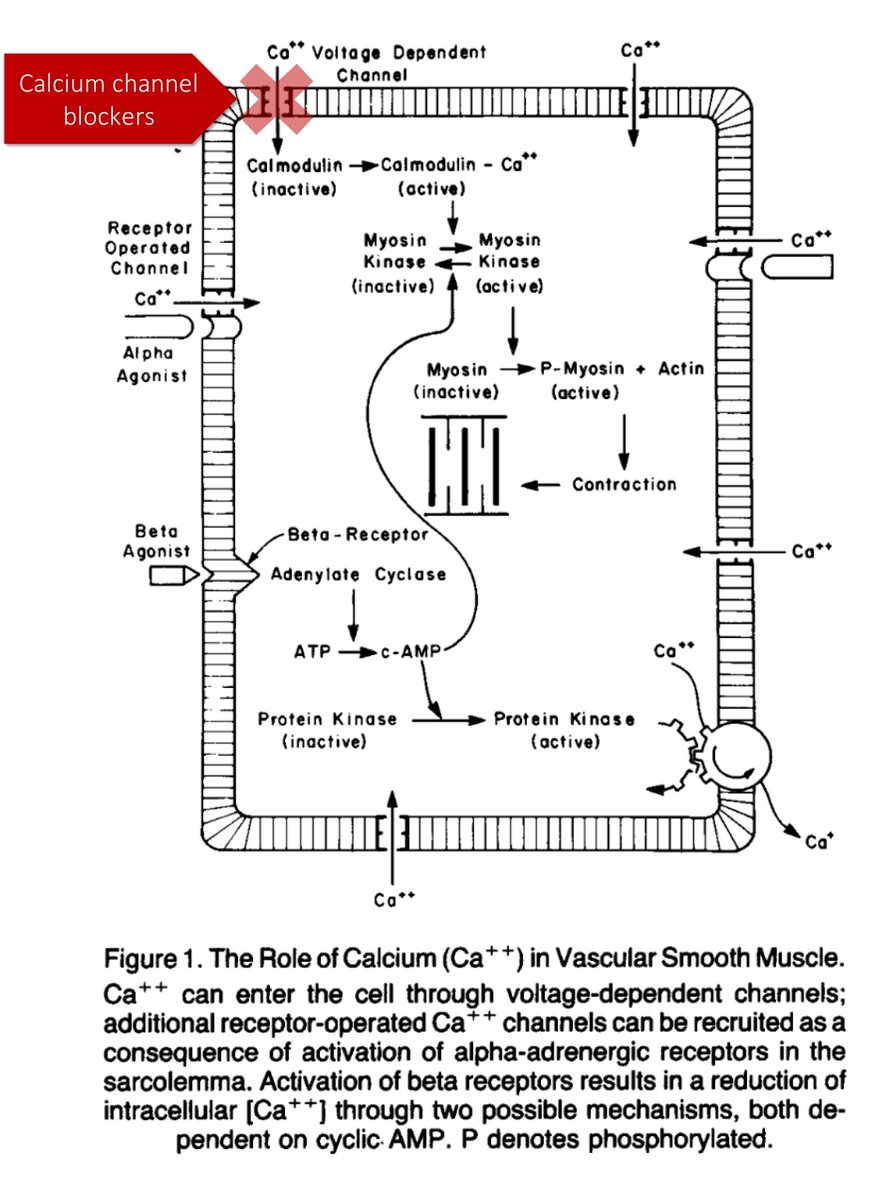
In order to answer my opening question, it will be helpful to understand how thrombus forms in the left atrium (LA).
Q2: Which of the components of Virchow’s triad contribute to LA thrombus formation in AF?
Up until recently, I had a narrow ("stasis only") conception of thrombus formation in AF:
*LA fibrillates ➡️ stasis of blood flow (particularly in the LA appendage) ➡️ thrombus formation
It's not just stasis though. The other two components of the triad are active too!
re: Stasis.
We likely all presume the chaotic LA contractions lead to blood stasis. On echocardiogram this manifests as spontaneous echo contrast (SEC), also known as “smoke”.
SEC is correlated with both thrombus in the LA and thromboembolism.
ncbi.nlm.nih.gov/pubmed?term=18…
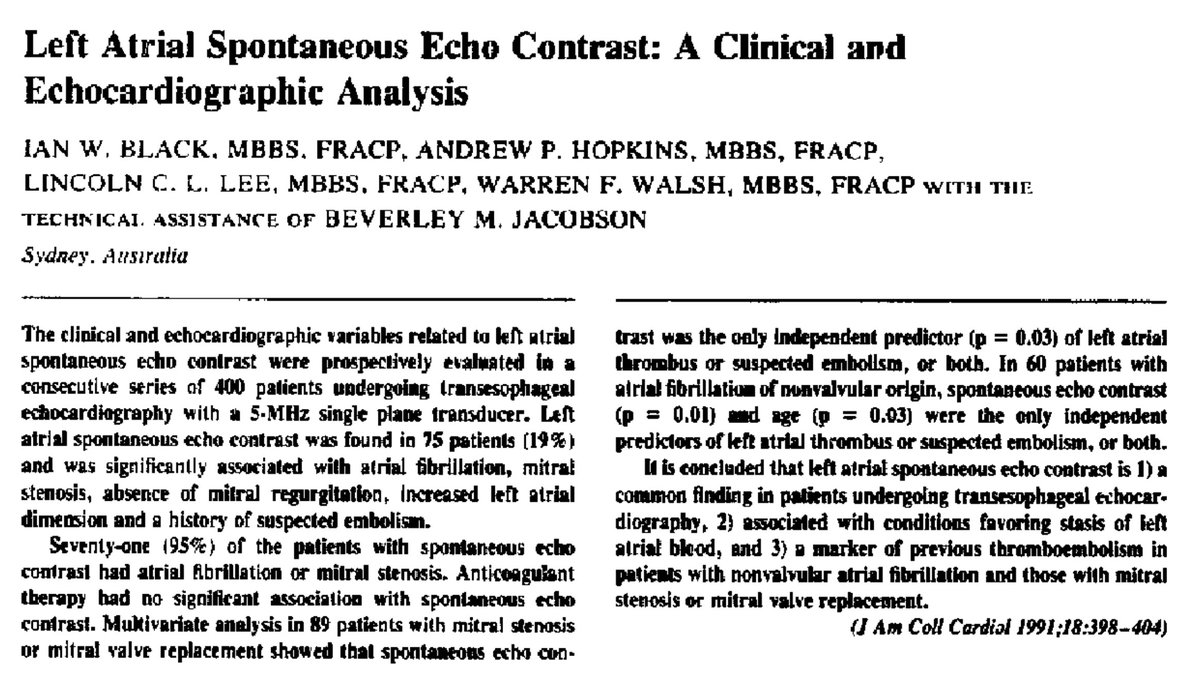
SEC is a product of RBC aggregation in the setting of low shear rates. This is seen in the LA, particularly the LA appendage.
What promotes RBC aggregation? Fibrinogen!
RBC are negatively charged. Fibrinogen crosslinks them (just like in an ESR).
ncbi.nlm.nih.gov/pubmed/8426010
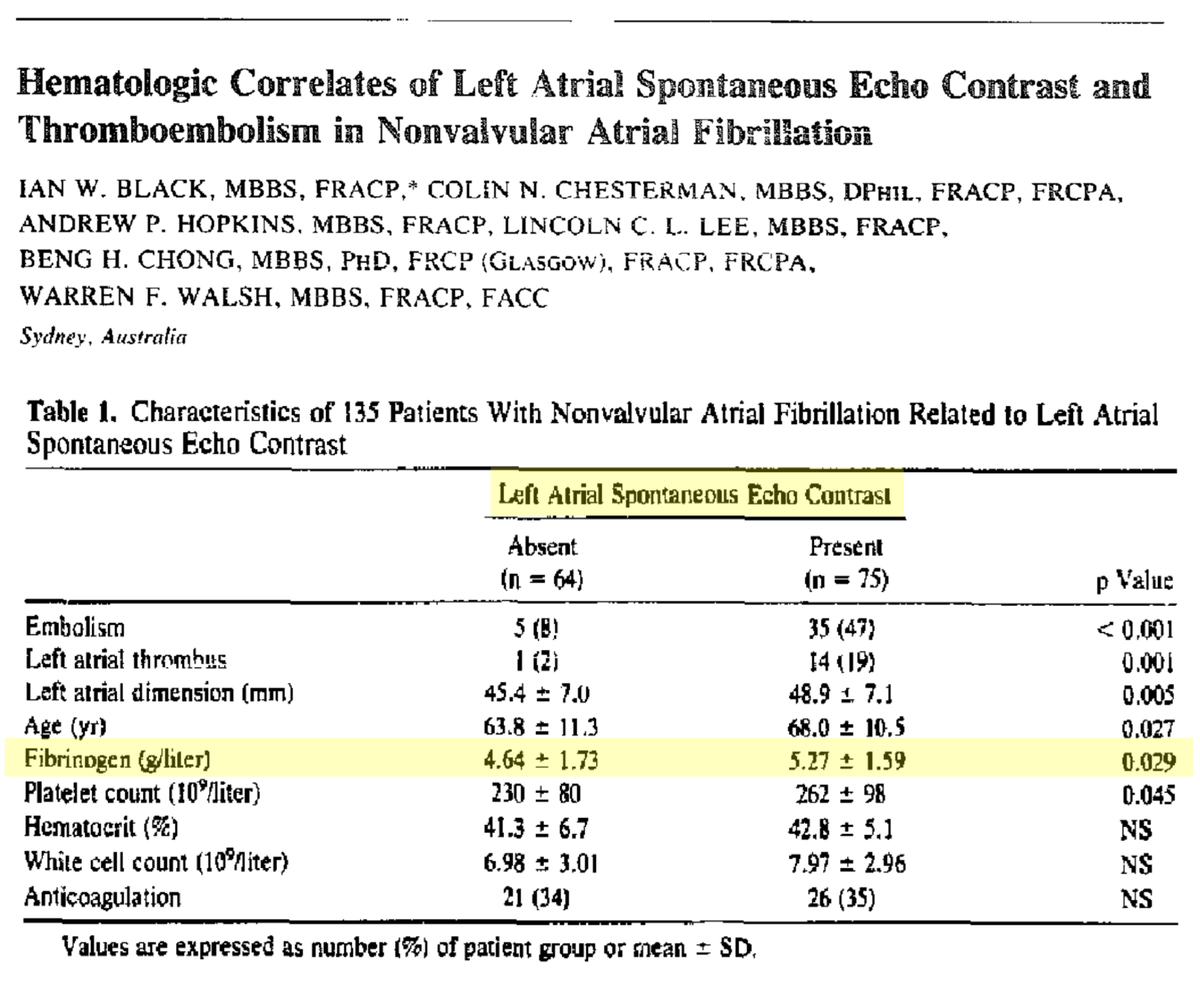
This is some of the evidence of the hypercoagulable state of AF.
Again, fibrinogen promotes RBC crosslinks, leading to SEC and subsequent thrombus formation. Turns out, patients with AF have more fibrinogen.
ncbi.nlm.nih.gov/pubmed/8721646
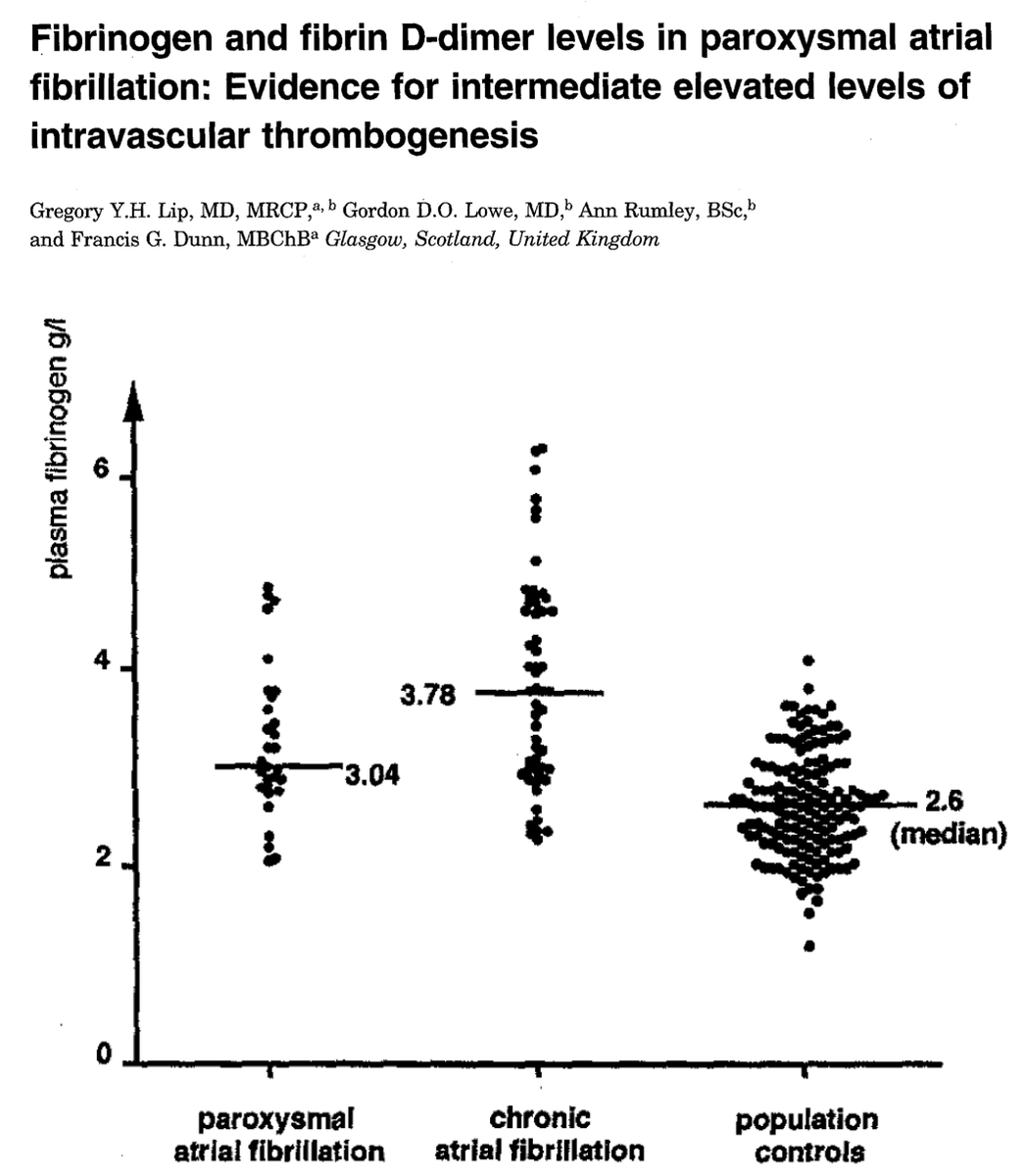
There are increased levels of other markers suggesting hypercoagulability (e.g., d-dimer).
And, both vWf and tissue factor are overexpressed in the atrial endothelium in patients with AF, supporting the idea that endothelial injury is also at play.
ncbi.nlm.nih.gov/pubmed/19135613
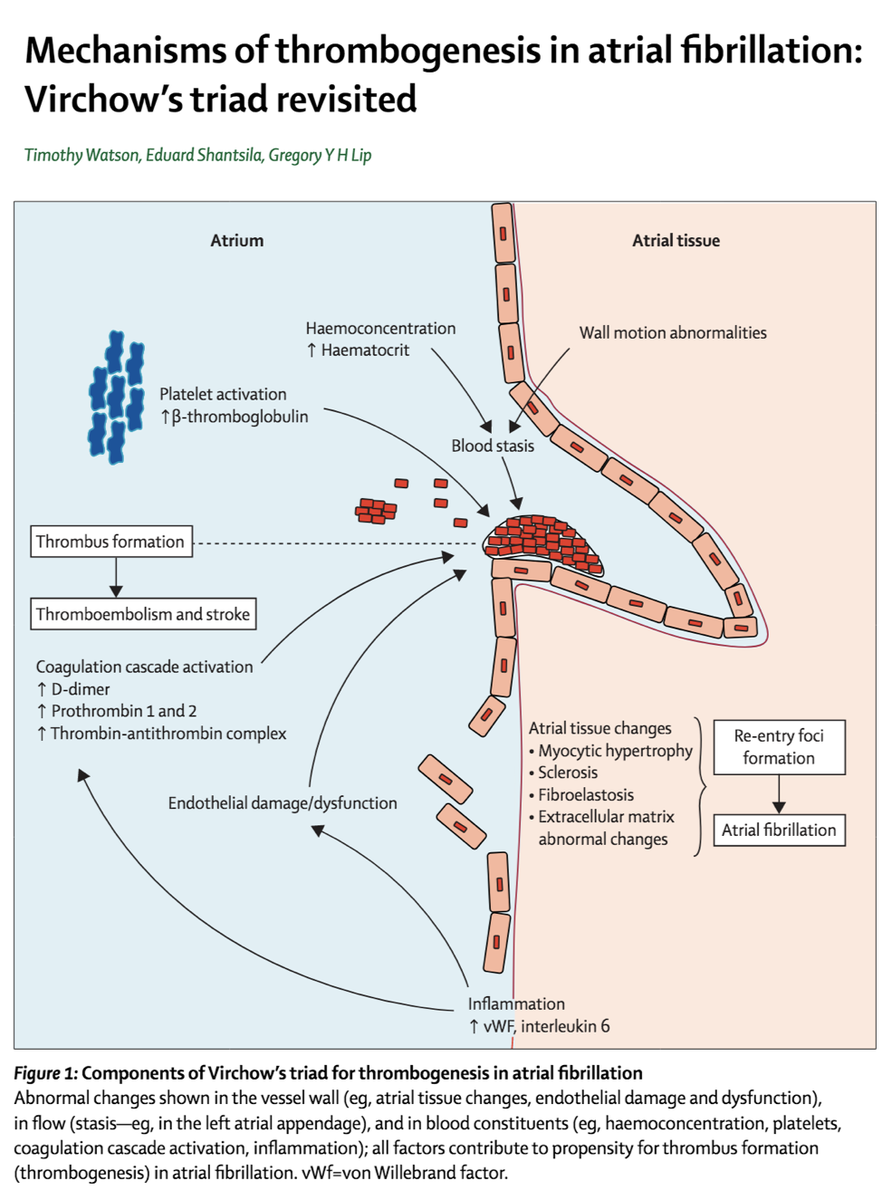
So, in patients with atrial fibrillation, LA thrombus is a product of stasis, hypercoagulability, and endothelial injury. The latter two shouldn’t be any different in the RA. But, is the RA as susceptible to stasis?
Wait, does the right atrium even have an appendage?
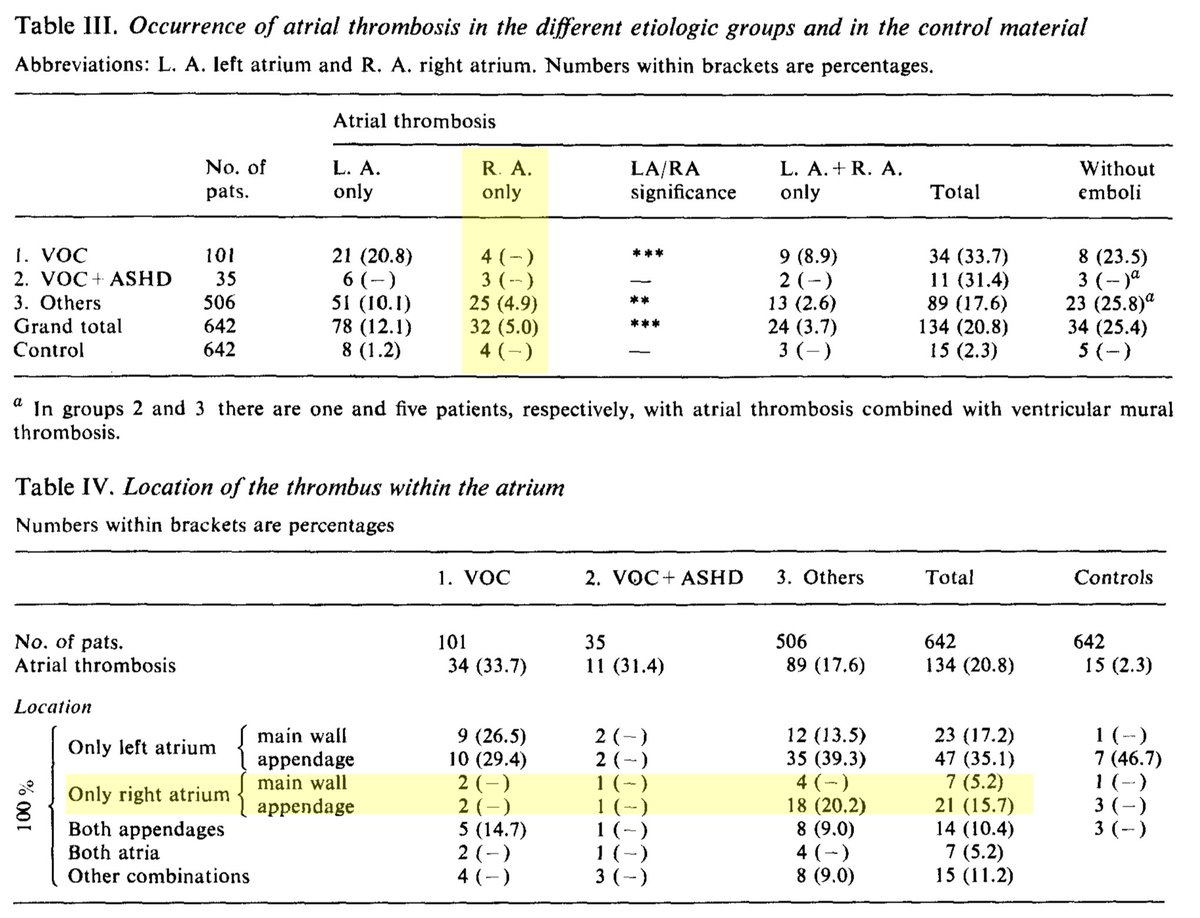
The right atrium DOES have an appendage! And thrombus is seen in the RA, particularly in the appendage. We’ve known this for decades with a famous 1969 autopsy study providing early proof.
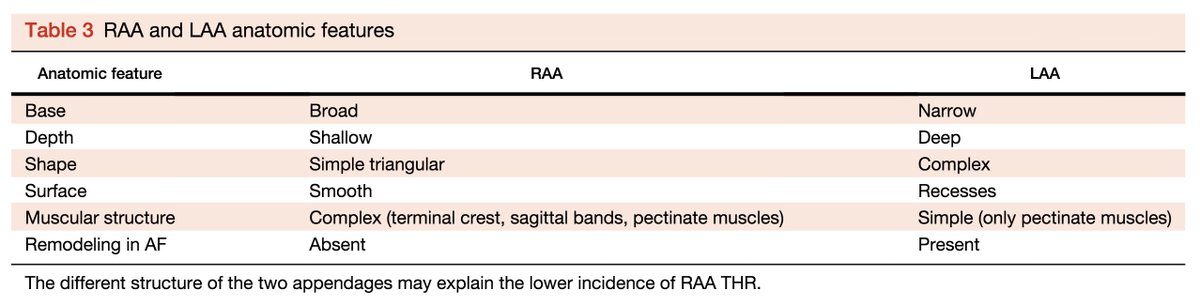
Note that rates of RA thrombus are lower than LA thrombus.
ncbi.nlm.nih.gov/pubmed/5808636
Interim summary:
*AF thrombus formation relates to stasis, hypercoagulability, and endothelial injury
*thrombus can form in both the LA and RA, particularly in the appendages
*RA thrombus is less common than LA thrombus
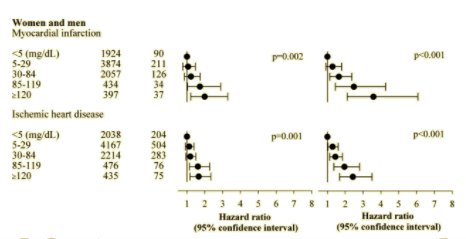
We’re finally ready to address the original question: is AF associated with (a risk for) pulmonary embolism?
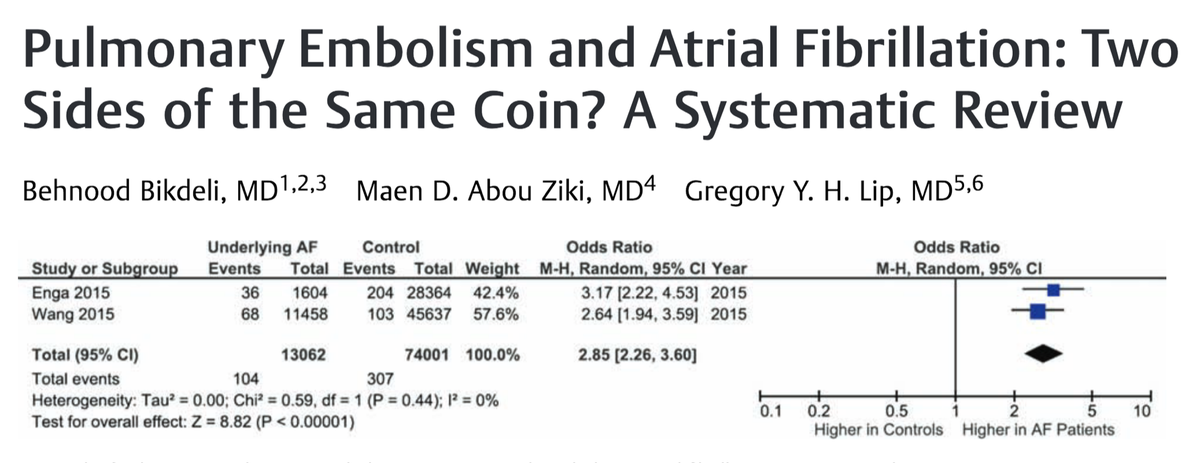
A number of studies have examined this. While not all of them show an association, it seems that the preponderance of evidence supports one.
ncbi.nlm.nih.gov/pubmed/28196379
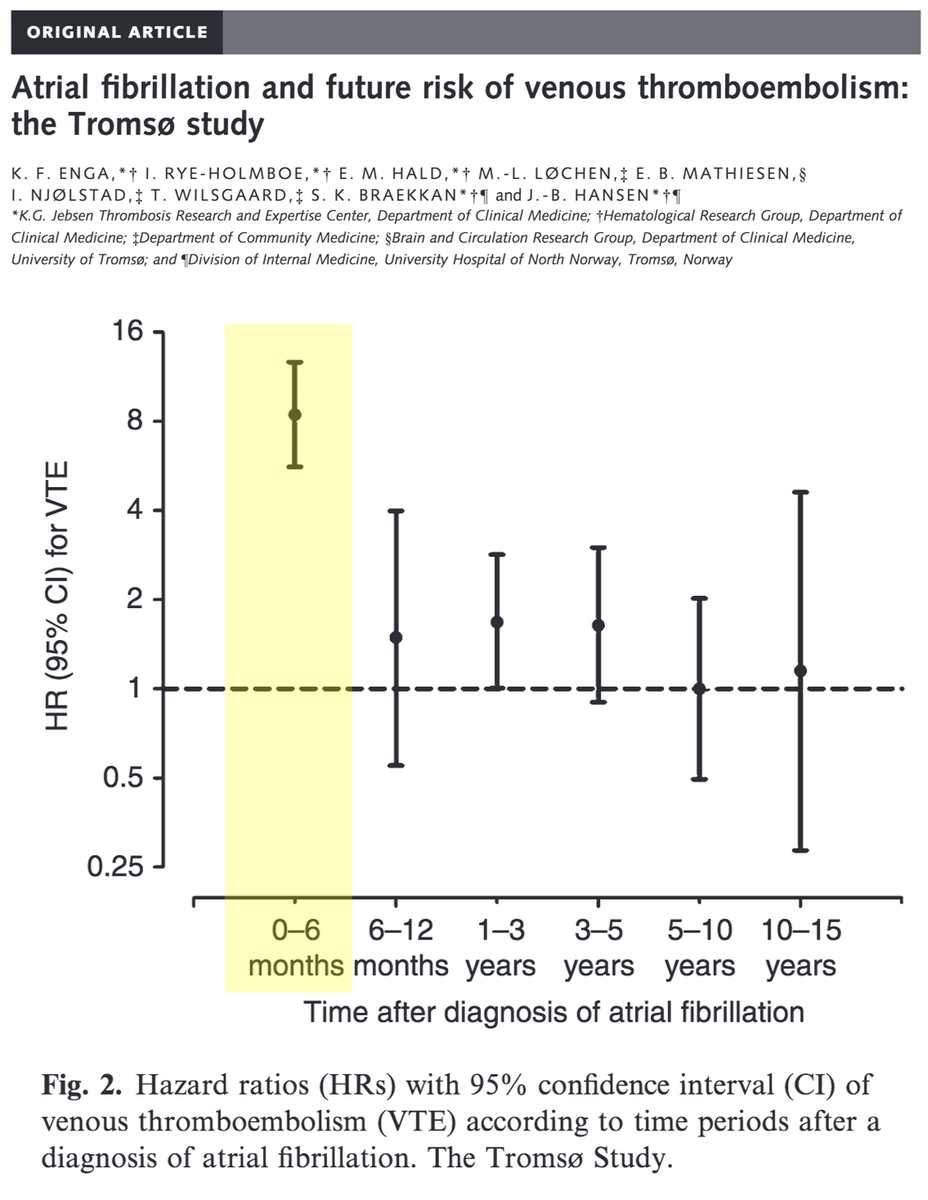
The risk of pulmonary embolism seems to be strongest in the months immediately after a diagnosis of AF is made.
I wonder if some of these patients have RA thrombus at the time of AF diagnosis (i.e., before they're on anticoagulation).
ncbi.nlm.nih.gov/pubmed/25330989
One explanation may be the anatomic differences between the RA appendage and LA appendage (the most common sites of thrombus formation). These anatomic differences may lead to different propensities to thrombus formation.
ncbi.nlm.nih.gov/pubmed/25240491
If some PEs are the result of AF and RA thrombus, this may partly explain two observations:
*not all patients with PE have evidence of DVT (~50%)
*recurrent VTE after PE are usually PE (~60%)
ncbi.nlm.nih.gov/pubmed/16162763
ncbi.nlm.nih.gov/pubmed/12814982
Let's close with versions of our original questions, in reverse:
Q2 (repeat): Which of the components of Virchow’s triad contribute to LA thrombus formation in AF?
Q1 (repeat): Do you NOW consider atrial fibrillation (AF) to be a risk factor for pulmonary embolism (PE)?