Let’s start with a question.
Which of the following components of the Starling Equation is altered in those with calcium channel blocker associated edema?
[Pc = capillary hydrostatic pressure; Pi = interstatitial hydrostatic pressure; Πc = capillary oncotic pressure]
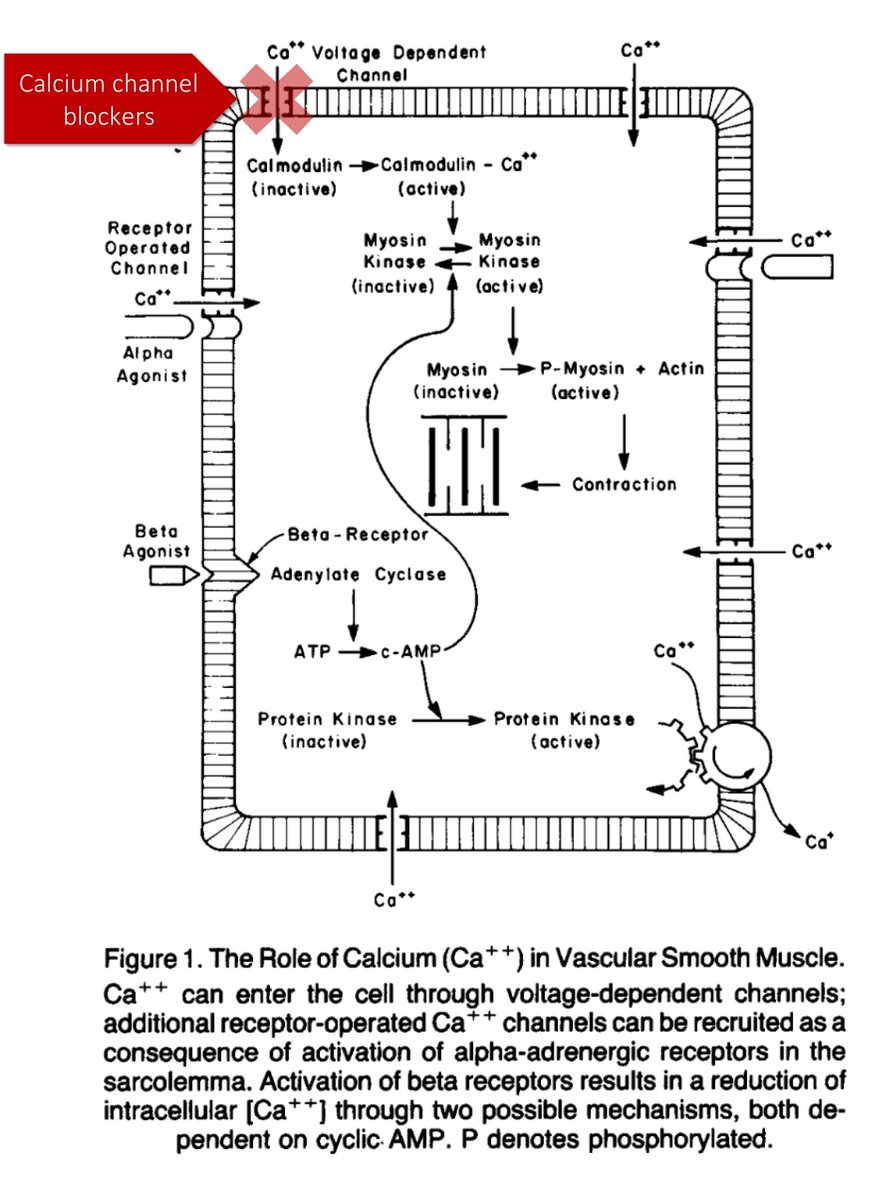
In order to understand the answer (↑Pc), we must review the mechanism of calcium channel blockers (CCBs).
By decreasing intracellular [Ca], CCBs lead to arterial vasodilation. This, in turn leads to a decrease in blood pressure.
ncbi.nlm.nih.gov/pubmed/6292718
Based on this, a proposed mechanism for edema could be:
↓BP ➜ ↑Na reabsorption ➜ ↑Pc
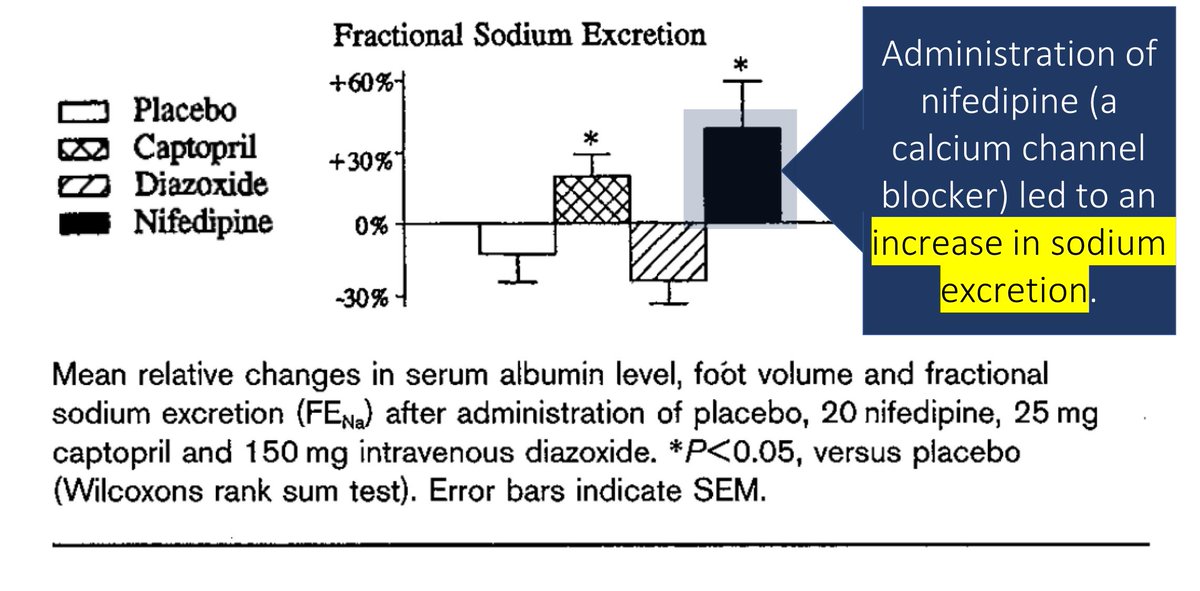
But CCBs don’t increase plasma volume. If anything, they cause natriuresis.
It isn't an increase in total fluid that's the problem; it's a SHIFT in the fluid.
ncbi.nlm.nih.gov/pubmed/8884561
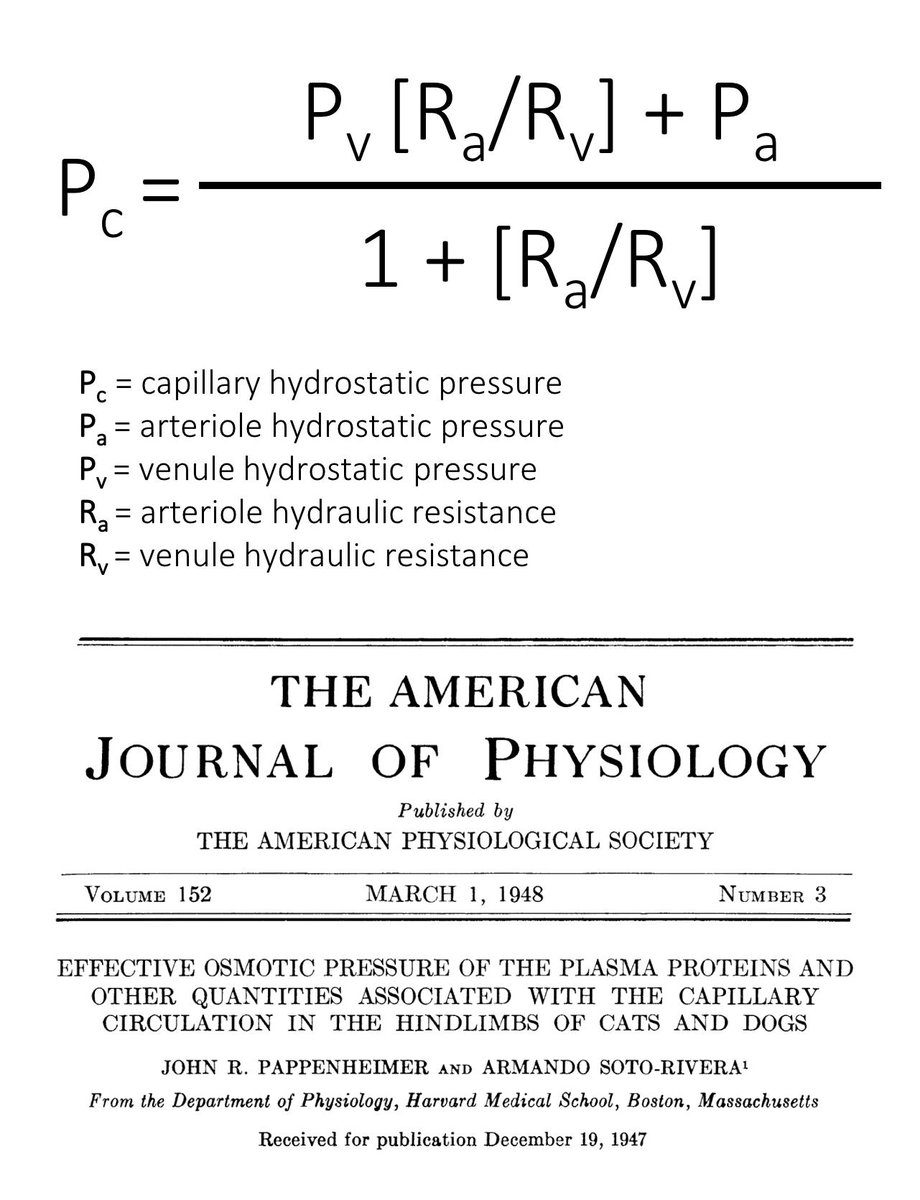
One hint to the mechanism of edema with CCBs comes from the Pappenheimer Soto-Rivera equation, first described in 1948.
This equation outlines the factors contributing to Pc.
ncbi.nlm.nih.gov/pubmed/18863145
The key component of the Pappenheimer Soto-Rivera is the Ra/Rv ratio.
As arterioles dilate (i.e., the Ra/Rv decreases), Pc increases.
As arterioles constrict (i.e., the Ra/Rv increases), Pc increases.
ncbi.nlm.nih.gov/pubmed/26985394
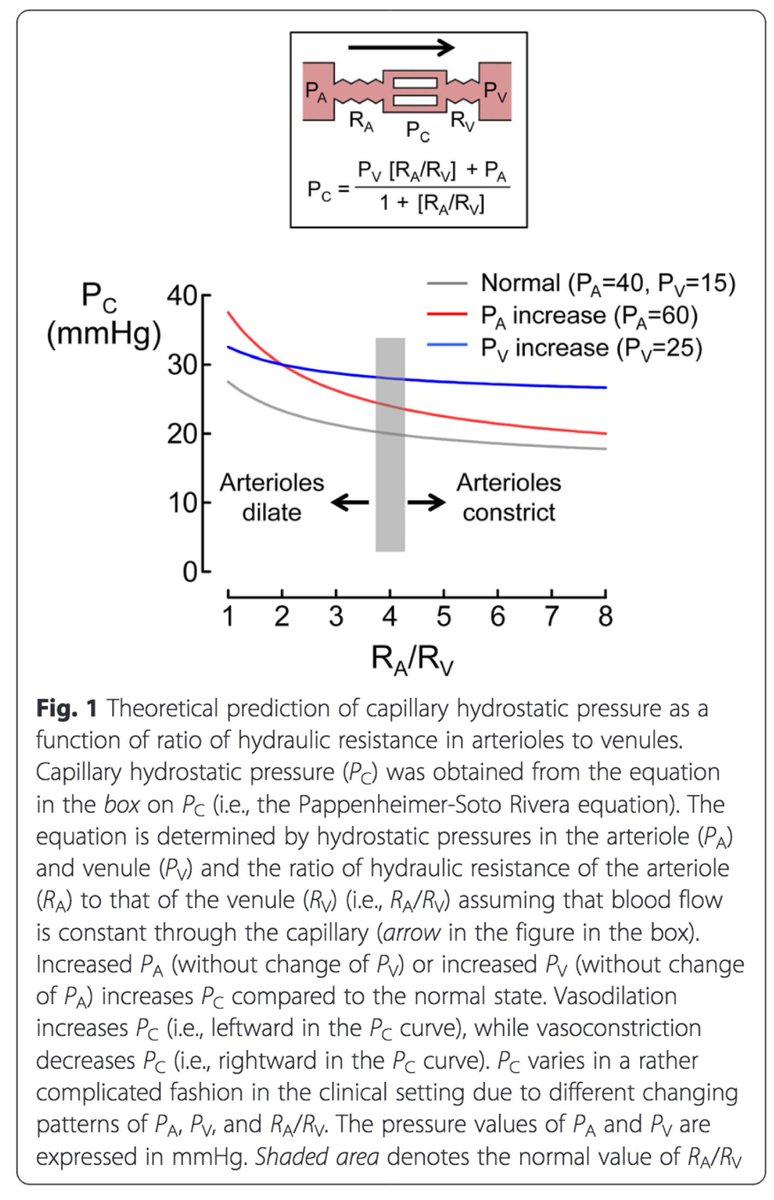
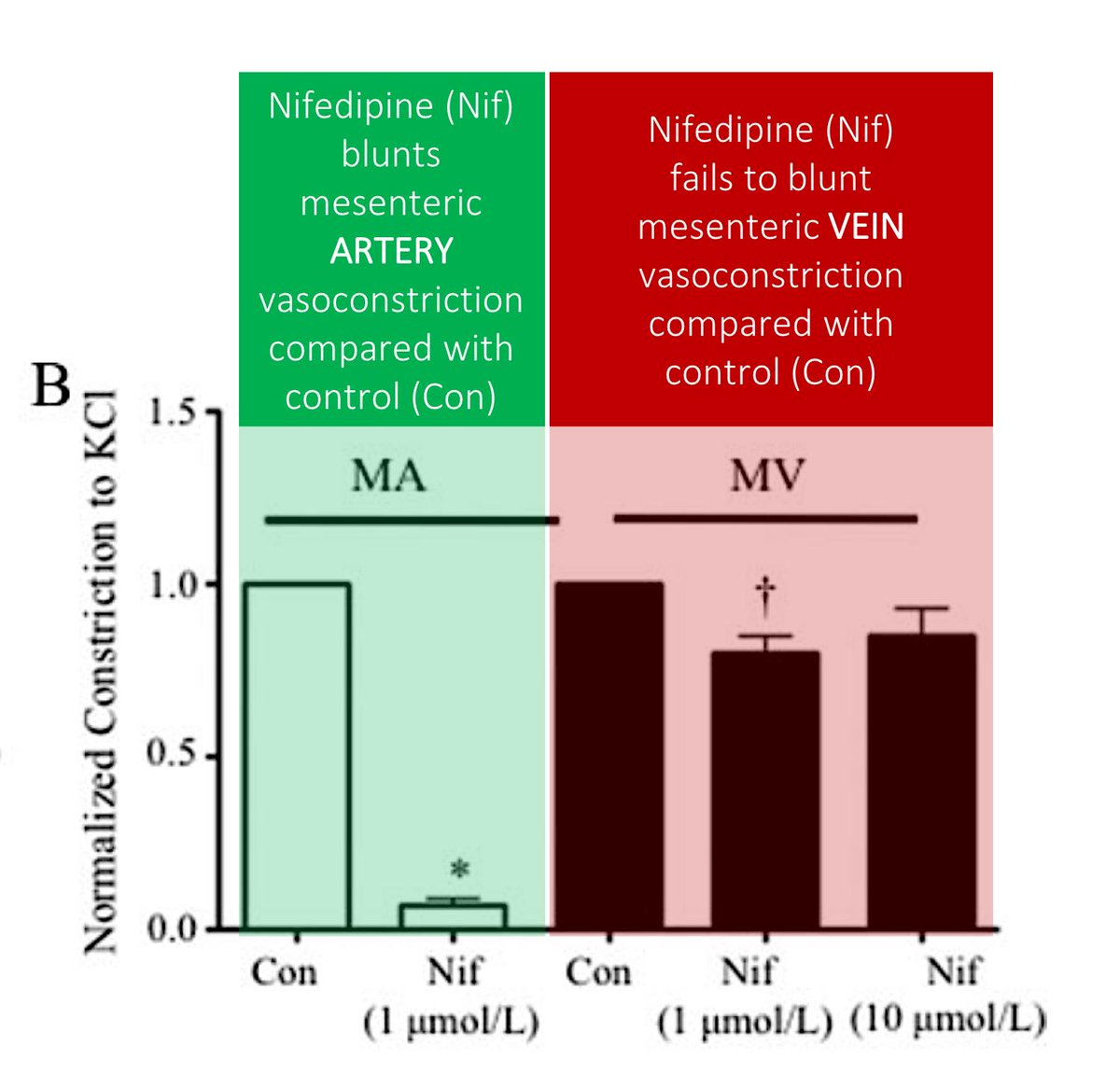
⭐️CCBs dilate precapillary arterioles (i.e., they decrease Ra a lot) and may not dilate postcapillary venules (i.e., they don’t change Rv).⭐️
↓Ra ➜ ↓Ra/Rv ➜ ↑Pc ➜ EDEMA!
ncbi.nlm.nih.gov/pubmed/20044515
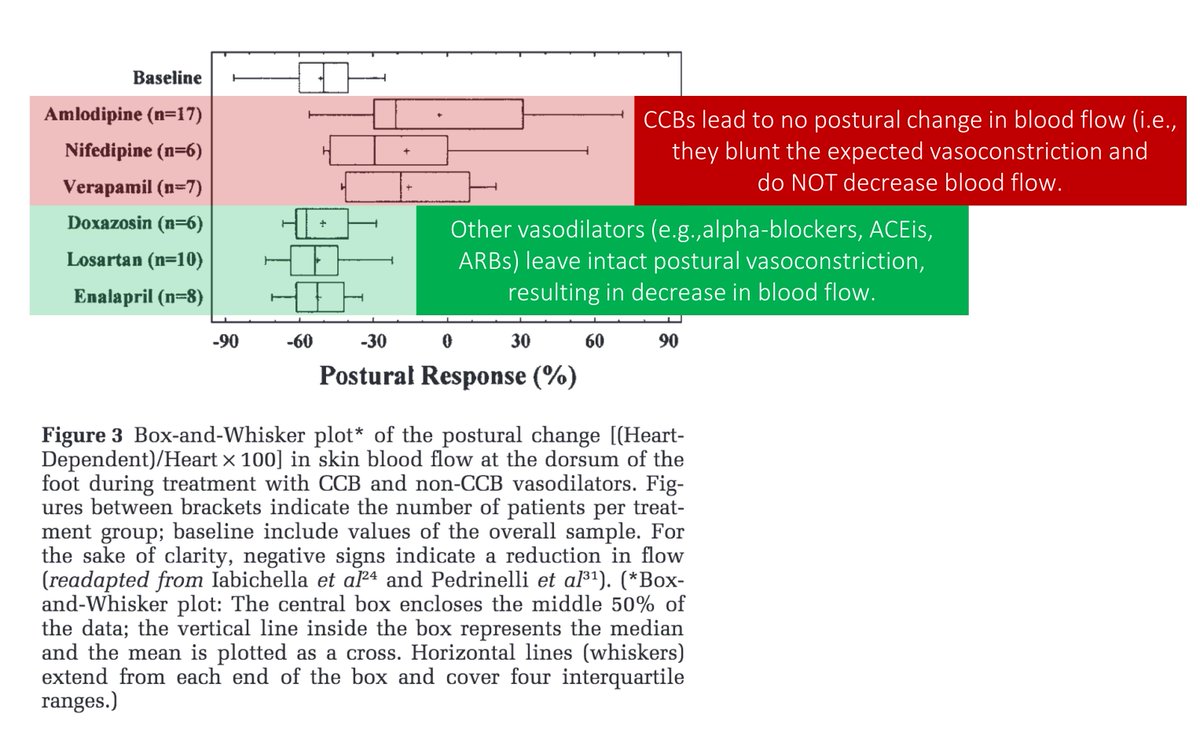
Another mechanism of CCB mediated edema is the loss of reflex vasoconstriction that occurs with standing.
In particular, CCBs may block the myogenic response (i.e., arteriolar vasoconstriction in response to increased transmural pressure).
ncbi.nlm.nih.gov/pubmed/11464254
Let’s apply the above to answer three questions.
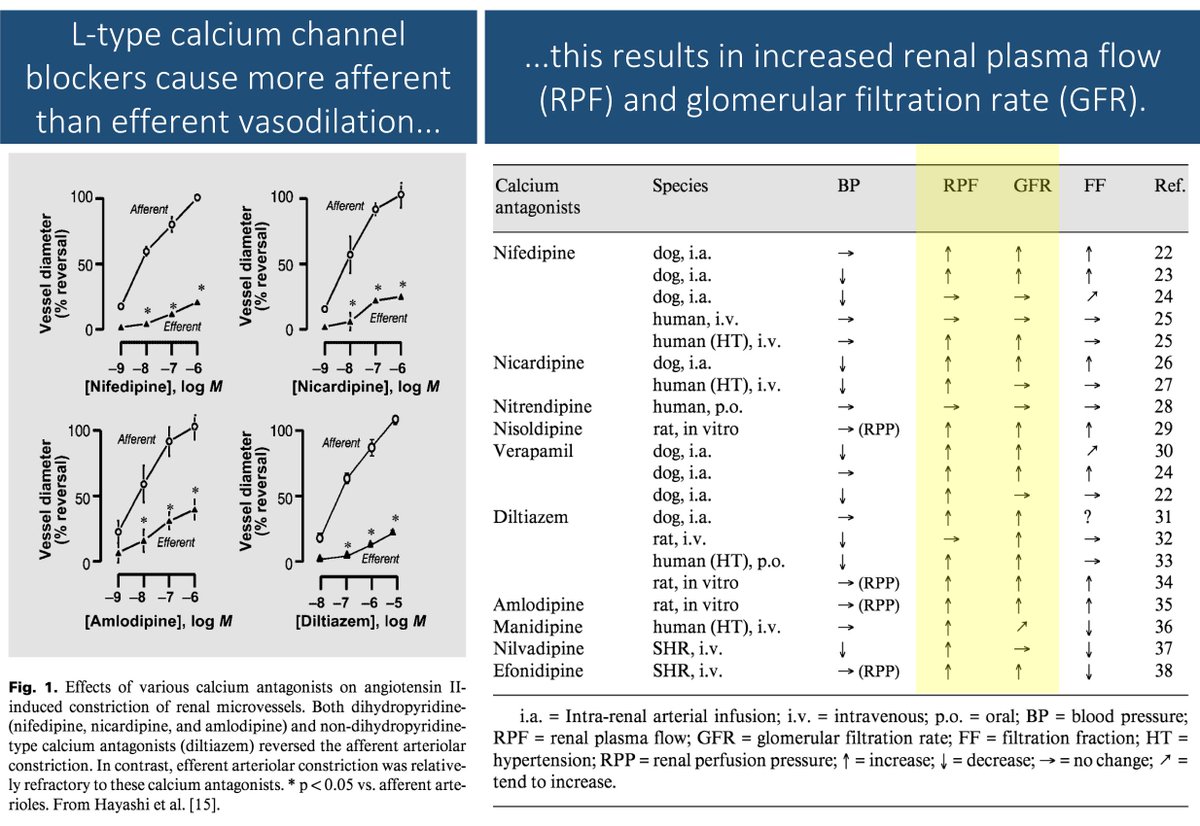
Q1: Based on their mechanism of action, how would you predict CCBs affect glomerular filtration rate?
Because CCBs preferentially dilate precapillary arterioles, they should increase GFR. There is evidence suggesting exactly this.
This study found more afferent than efferent dilation with L-type CCBs.
Result: ↑renal plasma flow and ↑GFR.
ncbi.nlm.nih.gov/pubmed/12840599
Q2: In what season would you expect patients to experience more edema?
One super cool 2016 looked at Google searches for edema symptoms (e.g., "swollen feet").
In the US, the peak searches were in June.
In Australia, the peak searches were in December.
These are mid-summer months for each country.
ncbi.nlm.nih.gov/pubmed/27401424
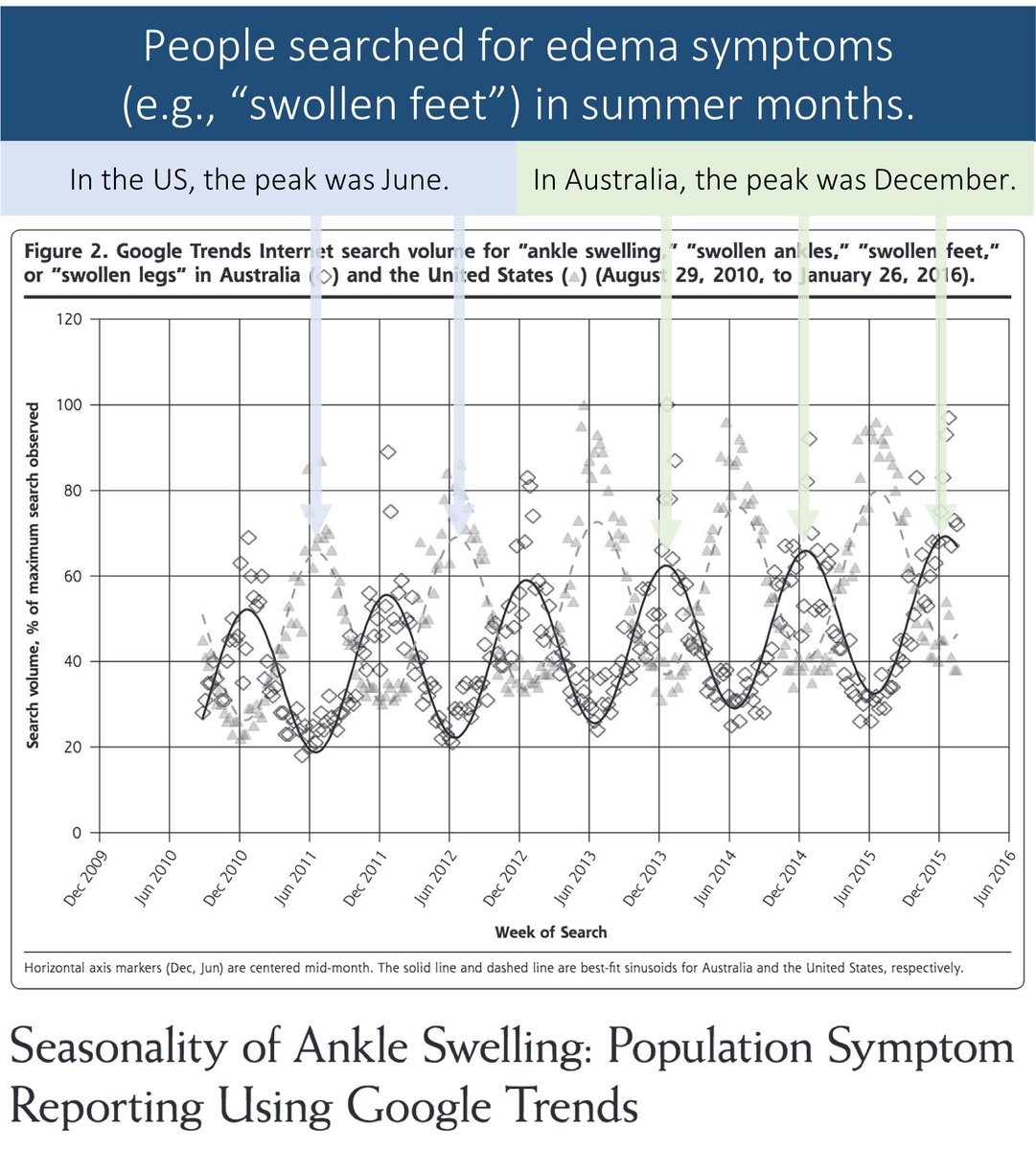
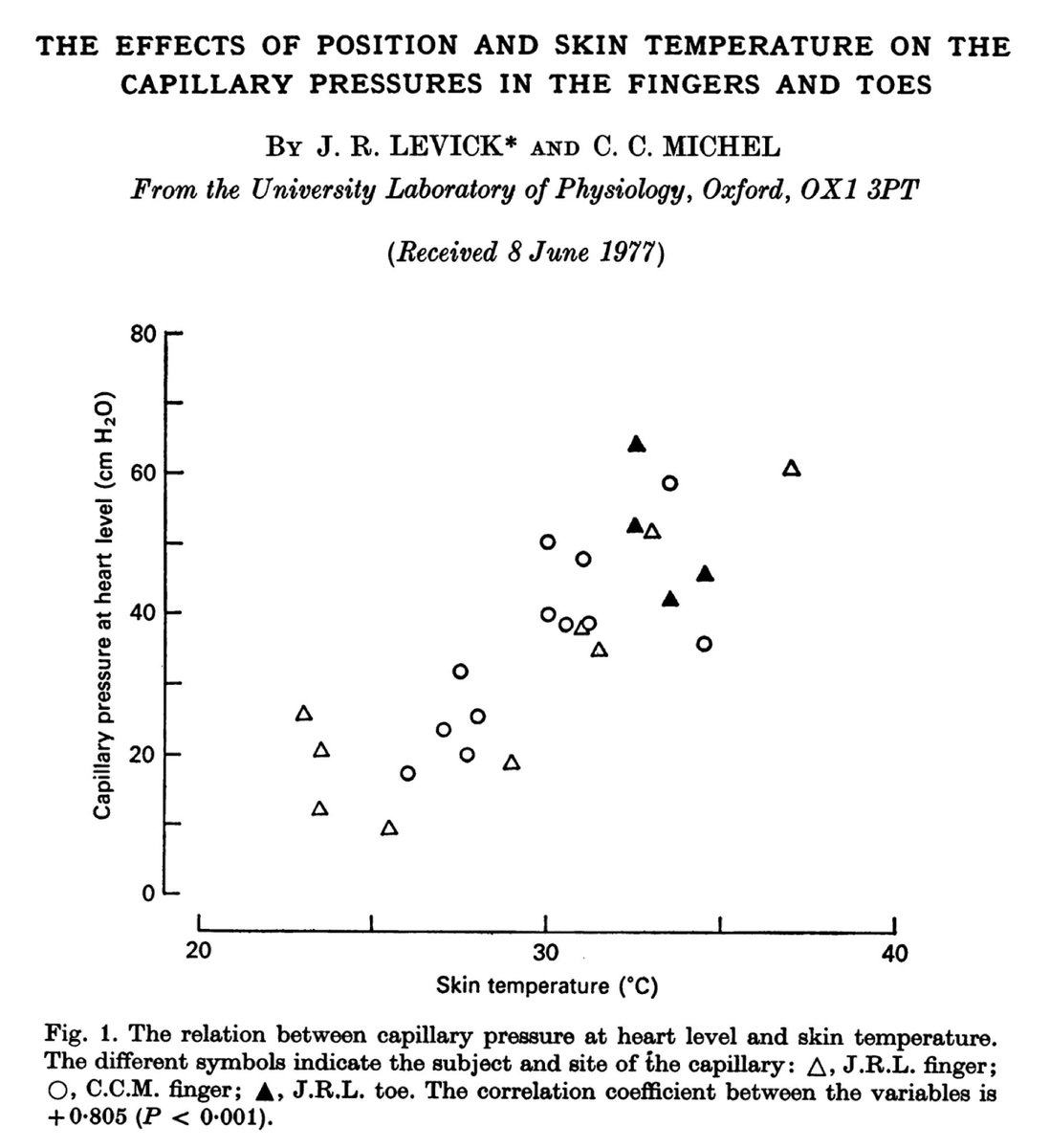
These findings may be explained by the fact that warm temperatures lead to arteriolar vasodilation.
And, as noted above, arteriolar vasodilation leads to edema.
Some have suggested that amlodipine-mediated edema may have similar seasons variation.
ncbi.nlm.nih.gov/pubmed/625016
Q3: Which medication is more likely to prevent CCB-mediated edema?
Because the edema of CCBs is not mediated by sodium retention (see tweet 4), pre-treatment with diuretics may not mitigate this side effect.
At least one study supports this.
ncbi.nlm.nih.gov/pubmed/15076203
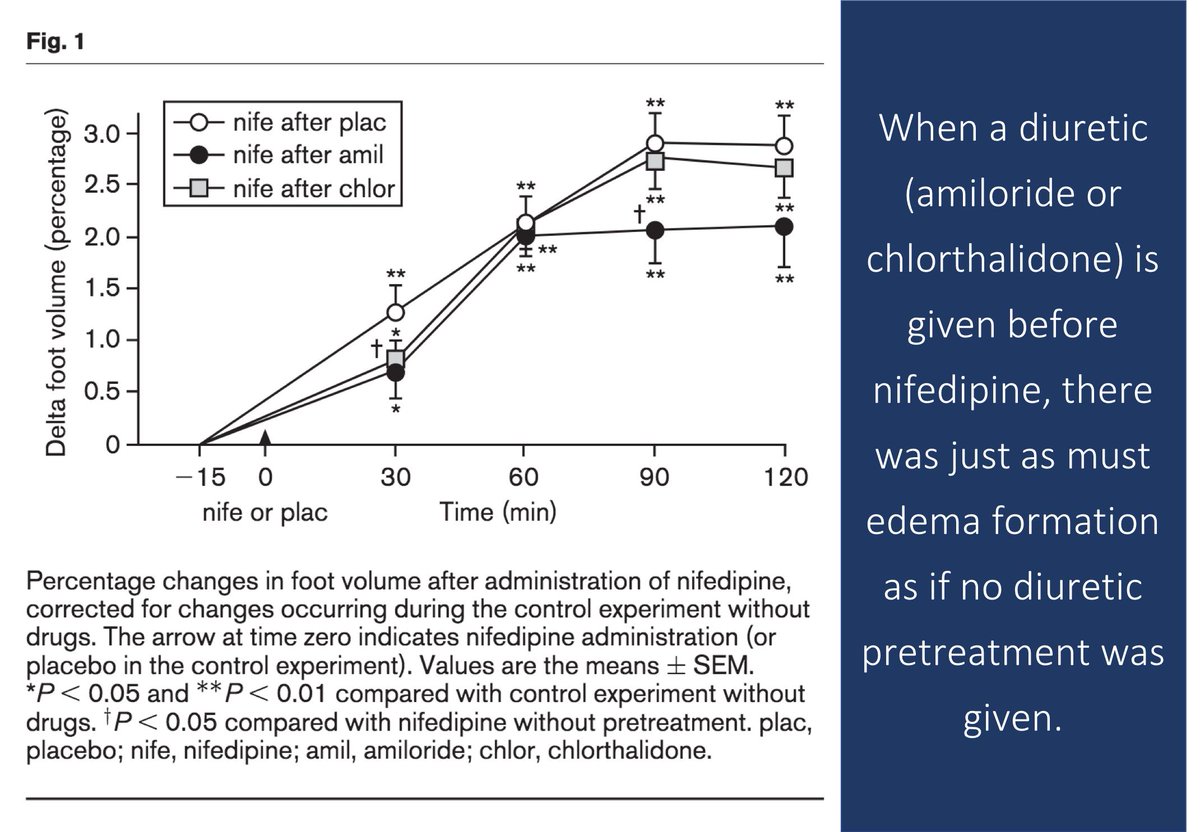
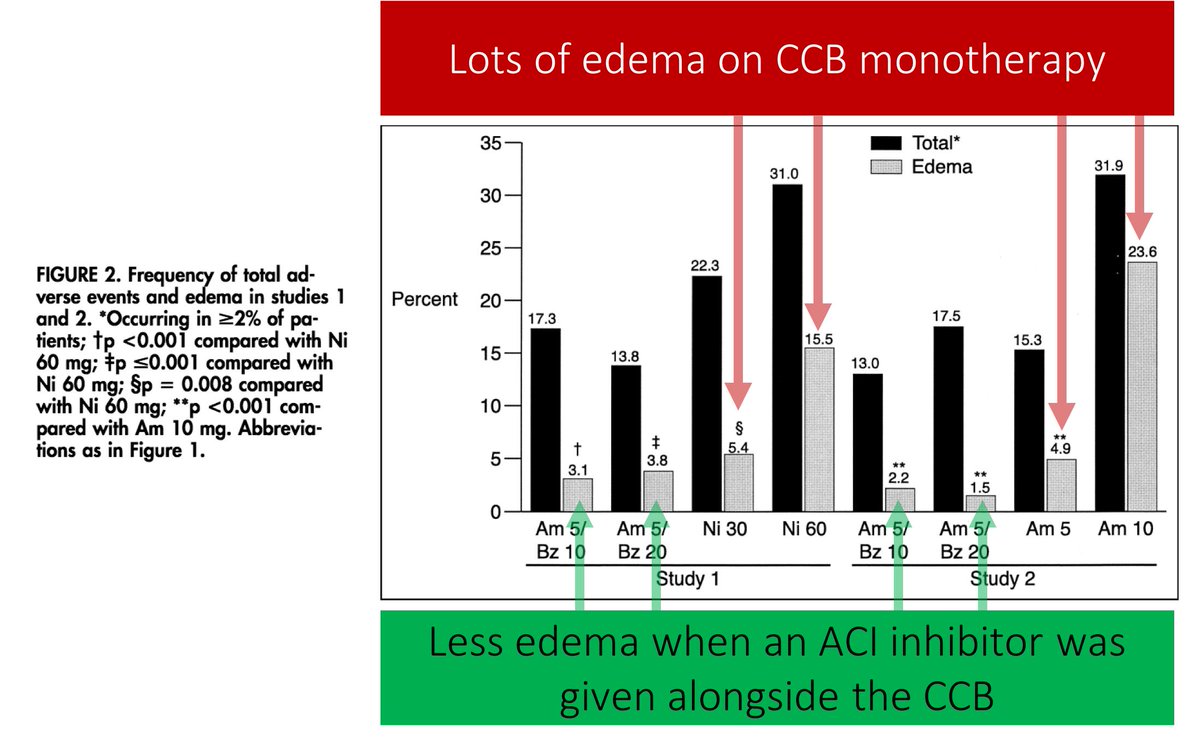
ACE inhibitors, on the other hand, produce vasodilation in the pre AND post-capillary vessels. As a result, they are able to mitigate the increase in Pc seen with CCBs.
Result: edema is less common when ACE inhibitors are given alongside CCBs.
ncbi.nlm.nih.gov/pubmed/11090788
➢Because CCBs cause a natriuresis, sodium retention isn't the problem
➢CCBs dilate precapillary arterioles and don't dilate postcapillary venules
➢This leads to increased Pc and EDEMA
➢ACE inhibitor may mitigate this
As a few people have pointed out, tweet 6 should read:
"As arterioles constrict (i.e., the Ra/Rv increases), Pc DECREASES."