H pylori #tweetorial for resistant H pylori
#AGA released CPU in 4/21 revisiting topic of resistance/treatment failures, not a guideline, but the expert opinion @BradSpellberg loves! (1/x)
gastrojournal.org/article/S0016-…
@ABsteward @RushCCH_ID #MedEd #medtwitter #idtwitter
#AGA released CPU in 4/21 revisiting topic of resistance/treatment failures, not a guideline, but the expert opinion @BradSpellberg loves! (1/x)
gastrojournal.org/article/S0016-…
@ABsteward @RushCCH_ID #MedEd #medtwitter #idtwitter
As GN bacteria go, it's an interesting bug:
Highly motile, curved, GNR, #Urease-positive, catalase-positive, oxidase-positive
Related to Campylobacter, for family fun
Nice crossover with our #Gastroenterology colleagues, eh #IDtwitter and @IDSAInfo
(2/x)
Highly motile, curved, GNR, #Urease-positive, catalase-positive, oxidase-positive
Related to Campylobacter, for family fun
Nice crossover with our #Gastroenterology colleagues, eh #IDtwitter and @IDSAInfo
(2/x)
GN, and as such should be sensitive to most #antibiotics that target GN with pretty good susceptibilities over time for:
#amoxicillin #tetracycline #aminoglycoside #nitroimidazole #macrolide
(3/x)
#amoxicillin #tetracycline #aminoglycoside #nitroimidazole #macrolide
(3/x)
Historically, we've grown up as a species together, and it seems that during #evolution, we've both benefited.
Data suggest reduction in #asthma of childhood, and other atopic syndromes like #eczema (gotta be some #Pediatrics #Pulmonary folks interested, right?)
(4/x)
Data suggest reduction in #asthma of childhood, and other atopic syndromes like #eczema (gotta be some #Pediatrics #Pulmonary folks interested, right?)
(4/x)
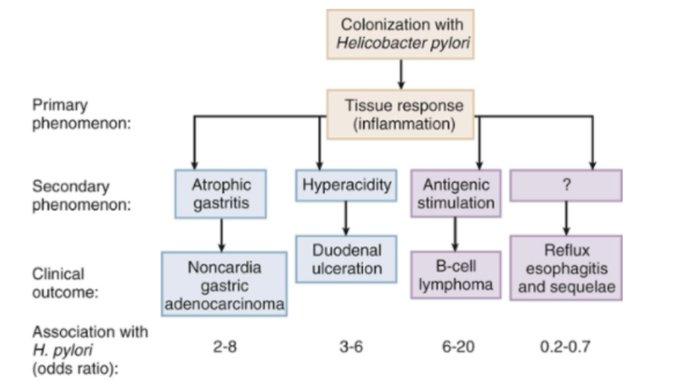
Though thriving in acidic environments, it's not the cause of #GERD, but instead of chronic #gastritis, and subsequently #ulcers (duodenal > gastric, thanks #NSAIDs) given increased gastrin production (5/x)
They also have 2 Lewis #antigens that perform molecular mimicry thereby promoting H pylori persistence, as T-regulatory cells downregulate inflammatory responses, hence why over time you have less acute symptoms, but risk of #cancer etc
Look for CagA + for CA
(6/x)
Look for CagA + for CA
(6/x)
Also affects our #leptin #ghrelin pathways, so may drive metabolic presentations of satiety and weight gain, with eradication leading to more weight gain as less satiety (7/x)
Often missed with acute infection:
n/v/epigastric pain x3-14d w/ intense #gastritis weeks later, & up to one year of hypochlorhydria (#gastrin overdrive leading to burnout of production)
(please #Gastroenterology chime in whenever, or some ID/GI guru if differing thoughts!) (8/x)
n/v/epigastric pain x3-14d w/ intense #gastritis weeks later, & up to one year of hypochlorhydria (#gastrin overdrive leading to burnout of production)
(please #Gastroenterology chime in whenever, or some ID/GI guru if differing thoughts!) (8/x)
So, as #infectiousdiseases when do we get called? Doesn't #Gastroenterology handle this? Or #primarycare ? First let's look at indications, and initial management (10/x)
Indications: #PUD #MALToma (eradication causes tumor regression) high risk gastric CA patients, s/p early resection of gastric CA
Rarely and as diagnosis of exclusion: ITP, B12 def, IDA
Only small improvement benefit in non-ulcerative dyspepsia, so not recommended
(11/x)
Rarely and as diagnosis of exclusion: ITP, B12 def, IDA
Only small improvement benefit in non-ulcerative dyspepsia, so not recommended
(11/x)
Principles of treatment
1.Monotherapy drives down prevalence, but not useful for eradication
2.Low pH makes #antibiotics ineffectual
3.Lots of acquired resistance (FLQ, macro, Flagyl)
4.Check #eradication 1m after tx with bx, UBT, HpSA, or 6m after with serological titers
(12/x)
1.Monotherapy drives down prevalence, but not useful for eradication
2.Low pH makes #antibiotics ineffectual
3.Lots of acquired resistance (FLQ, macro, Flagyl)
4.Check #eradication 1m after tx with bx, UBT, HpSA, or 6m after with serological titers
(12/x)
First, gotta have #diagnosis!
Invasive vs Non-Invasive
#EGD/#biopsy with stains and cultures and possibly PCR
or
Serum #serology, #urease breath test, fecal #antigen test
(13/x)
Invasive vs Non-Invasive
#EGD/#biopsy with stains and cultures and possibly PCR
or
Serum #serology, #urease breath test, fecal #antigen test
(13/x)
Serology #IgG based, as #IgM dropped off after ~21 days
Not vetted in peds
Can check after treatment 6m for low titer to no titer marker
Rapid #hpyloritestkit have low SENS/SPEC
Use in appropriate clinical settings/picture
(14/x)
Not vetted in peds
Can check after treatment 6m for low titer to no titer marker
Rapid #hpyloritestkit have low SENS/SPEC
Use in appropriate clinical settings/picture
(14/x)
#urease breath test UBT
take in some carbon 13 and 14 urea, then breathe out an hour later and find the CO2 with the 13 and 14
NEEDS TO BE OFF #protonpumpinhibitors for minimum 14 days! Otherwise false negative
Also, prior abx use for any condition may give false (-)
(15/x)
take in some carbon 13 and 14 urea, then breathe out an hour later and find the CO2 with the 13 and 14
NEEDS TO BE OFF #protonpumpinhibitors for minimum 14 days! Otherwise false negative
Also, prior abx use for any condition may give false (-)
(15/x)
Stool #Antigen Test (HpSA)
monoclonal Ab in test bind HpAg
Off PPIs again for 14 days to avoid false results!
Some patient avoidance of test given need to obtain sample themselves
(16/x)
monoclonal Ab in test bind HpAg
Off PPIs again for 14 days to avoid false results!
Some patient avoidance of test given need to obtain sample themselves
(16/x)
First line treatment!
Triple
- clarithro, amox, PPI
or
Quadruple therapy
- Bismuth, metro, tetra, PPI
- Non-Bismuth = amox, PPI, metro, clarithro
(17/x)
Triple
- clarithro, amox, PPI
or
Quadruple therapy
- Bismuth, metro, tetra, PPI
- Non-Bismuth = amox, PPI, metro, clarithro
(17/x)

#Bismuth is #bactericidal here, and interrupts mucosal adherence
#PPIs inhibit #urease activity and improve #antibiotics #efficacy by raising #pH!
(18/x)
#PPIs inhibit #urease activity and improve #antibiotics #efficacy by raising #pH!
(18/x)
Initial management has 10-20% failure rate!
#AntimicrobialResistance
#Fluoroquinolone resistance occurs after first exposure
#metronidazole has known 20-40% resistance rate esp in F w/ prior exposure
#clarithromycin resistance after exposure
Consider colonized, so⬆️exp
(19/x)
#AntimicrobialResistance
#Fluoroquinolone resistance occurs after first exposure
#metronidazole has known 20-40% resistance rate esp in F w/ prior exposure
#clarithromycin resistance after exposure
Consider colonized, so⬆️exp
(19/x)
Tenets for Failure:
1.Don't reuse clarithromycin in second or third line therapy!
2. No amoxicillin resistance, increase dosing/timing to have high troughs, 2-3g q6-q8h (PCN allergy testing PRN)
3. 14 days >10 days @BradSpellberg #longerisbetter
4.PPI adherence paramount!
(20/x)
1.Don't reuse clarithromycin in second or third line therapy!
2. No amoxicillin resistance, increase dosing/timing to have high troughs, 2-3g q6-q8h (PCN allergy testing PRN)
3. 14 days >10 days @BradSpellberg #longerisbetter
4.PPI adherence paramount!
(20/x)
Studies show #empiric treatment #noninferior to in vitro resistance testing
May reuse FLQ, and metro; avoid clarithro!
AGA CPU 2021 update below!
(21/x)
May reuse FLQ, and metro; avoid clarithro!
AGA CPU 2021 update below!
(21/x)

So, that's the upfront! First true #tweetorial attempt...
Lemme know if there are questions!
#MedEd #medtwitter #IDtwitter #hpylori #Gastroenterology #pepticulcerdisease #AntimicrobialResistance
@ABsteward @BradSpellberg @RushCCH_ID
(22)
Lemme know if there are questions!
#MedEd #medtwitter #IDtwitter #hpylori #Gastroenterology #pepticulcerdisease #AntimicrobialResistance
@ABsteward @BradSpellberg @RushCCH_ID
(22)
@mohammad from a GI perspective, leave your thoughts throughout!
@emilytemplewood any cases in your FP residency you’ve come across?
@briden_danielle in the GMO world?
@briden_danielle in the GMO world?
• • •
Missing some Tweet in this thread? You can try to
force a refresh