1) Welcome to an #accredited #tweetorial on optimizing the use of #SGLT2i in the management of #T2D. This program is accredited for 0.50 🆓credits for #physicians #nurses #physicianassociates #nursepratcitioners #pharmacists by @academiccme! I am @tmodarressi of @HeartDoctorNJ.
@AndrewJSauer @DrMichaelShapir @MichaelJBlaha @dramitkhera @pnatarajanmd @PamTaubMD @DrMarthaGulati @DrRaniKhatib @AAgarwalaMD @RpratleyMD @drricardocorrea @AliceYYCheng @SantosGallegoMD @SABOURETCardio @hvanspall @DLBHATTMD @cpcannon
2) This program is intended for healthcare professionals and is supported by an educational grant from Boehringer Ingelheim Pharmaceuticals Inc. and Eli Lilly Company. See archived programs, all by expert authors, still available for credit at cardiometabolic-ce.com.
3) Hot on the heels of cardiology legend Eugene Braunwald’s @NEJM review, in this tweetorial we will discuss the role of Sodium-glucose co-transporter 2 inhibitors (#SGLT2i) in the treatment of type 2 diabetes (#T2D).
See pubmed.ncbi.nlm.nih.gov/35613023/
See pubmed.ncbi.nlm.nih.gov/35613023/

4) See our previous tweetorials for extensive discussions of #T2D and the prevention and management of #heartfailure, foundations and management of #DKD, and role of #SGLT2i in #cardiometabolic medicine.
cardiometabolic-ce.com/category/cardi…
ckd-ce.com/category/dkd/
Yes . . . even MORE🆓CE/CME!
cardiometabolic-ce.com/category/cardi…
ckd-ce.com/category/dkd/
Yes . . . even MORE🆓CE/CME!
5) First, let’s discuss T2D and the burden of disease in the United States. #Diabetes continues to be a growing public health challenge in the US. See
🔓cdc.gov/diabetes/data/…
🔓cdc.gov/diabetes/data/…
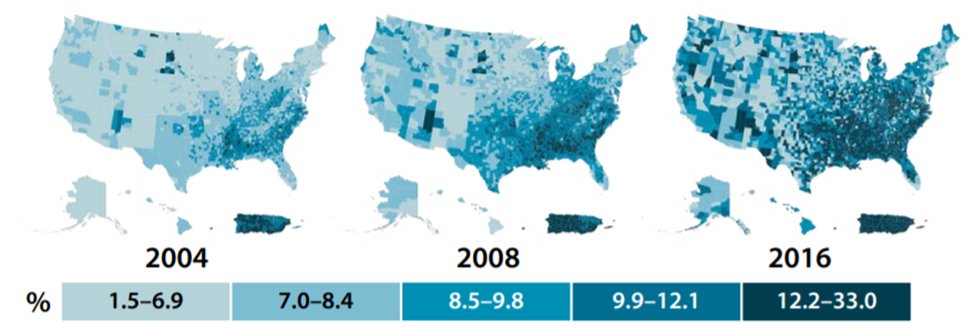
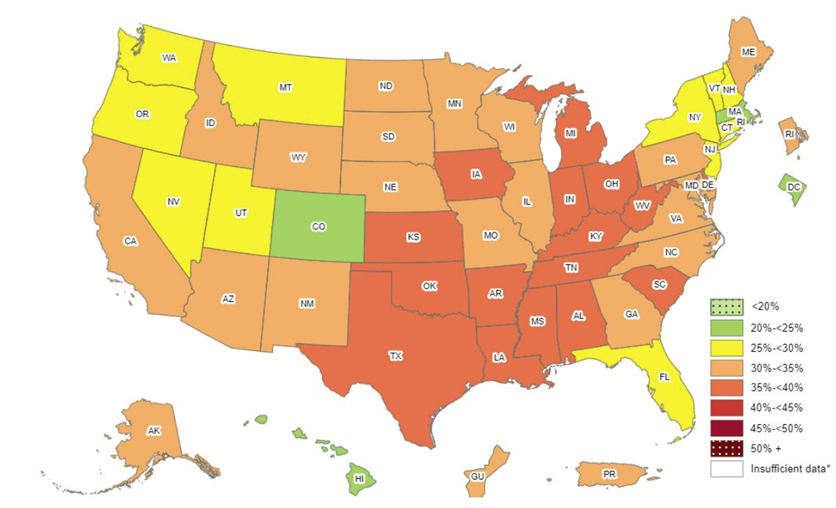
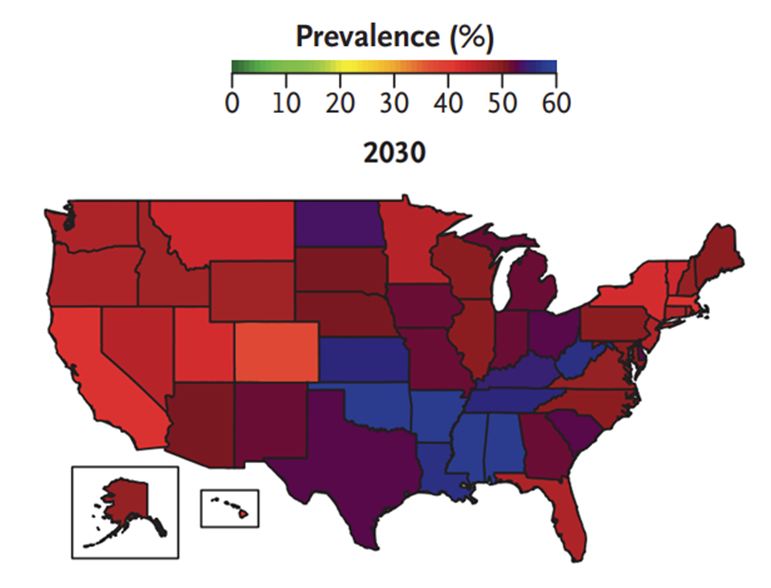
6) T2D does not begin with the 1st abnormal #A1c; it is often preceded by years/decades of #insulin resistance & other metabolic diseases. T2D prevalence is expected to 🔼🔼 given the tidal wave of #obesity in the 🇺🇸.
See 🔓cdc.gov/obesity/data/p… and 🔓doi.org/10.1056/NEJMsa…

See 🔓cdc.gov/obesity/data/p… and 🔓doi.org/10.1056/NEJMsa…
7) So what is T2D and how can SGLT2i help manage the hyperglycemia of this condition? A quick poll:
Type 2 diabetes is a disease related to:
a. ⬇️ b-cell insulin
b. Dysregulated hepatic function
c. ⬆️ renal glucose reabsorption
d. All of the above and more
Type 2 diabetes is a disease related to:
a. ⬇️ b-cell insulin
b. Dysregulated hepatic function
c. ⬆️ renal glucose reabsorption
d. All of the above and more
8) Answer *D*: Ralph DeFronzo famously described the “ominous octet” in 2009 and helped shift our understanding of T2D to a *multiorgan* process that leads to disordered energy metabolism. It is not simply a beta cell issue.
See 🔓doi.org/10.2337/db09-9…
See 🔓doi.org/10.2337/db09-9…

9) Another quick poll: while SGLT2i can affect multiple pathophysiologies involved in T2D, what organ is the primary target of its hypoglycemic effect?
10) It's B: While #SGLT2i actually help address multiple organ dysfunctions, their primary impact in glycemic control occurs at the #kidney. Let’s explore what happens to the kidney in the development of #T2D. 

11) A healthy kidney filters ~180 g of glucose daily, nearly all of which is reabsorbed (normal urine should be dipstick negative for glucose!). Most of this reabsorption (about 90%) occurs in the first segment of the proximal convoluted tubule by SGLT2. doi.org/10.1016/j.ejps… 
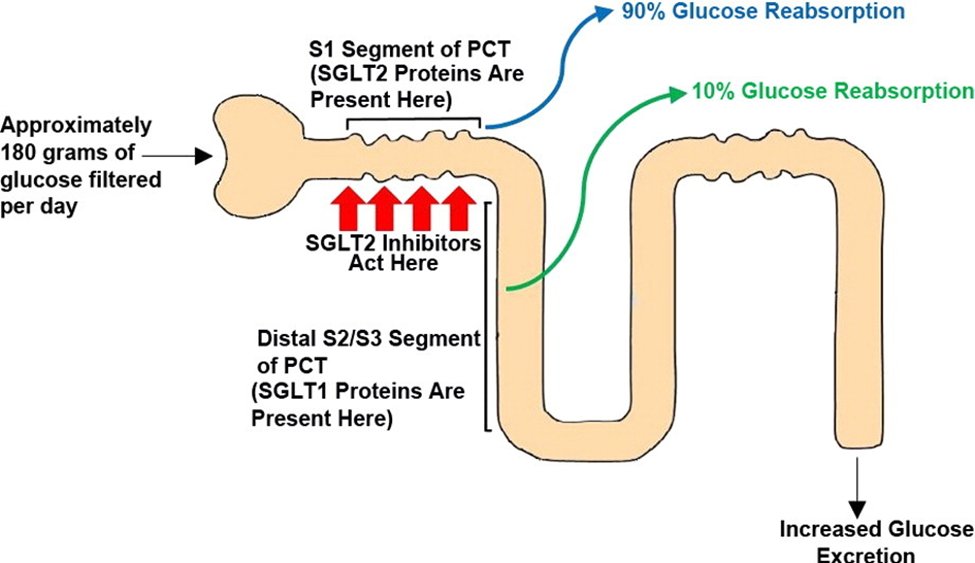
12) For those who 💕physiology: Sodium cotransport allows for glucose to be transported against an uphill gradient into the tubular epithelial cell. Glucose then leaves via facilitated diffusion using GLUT-2 on the basolateral membrane.
See 🔓doi.org/10.1007%2Fs001…
See 🔓doi.org/10.1007%2Fs001…

13) Typically, as long as plasma #glucose concentrations remain under about 180 mg/dL, essentially all filtered glucose undergoes reuptake. Only once this threshold is exceeded does a person experience #glucosuria.
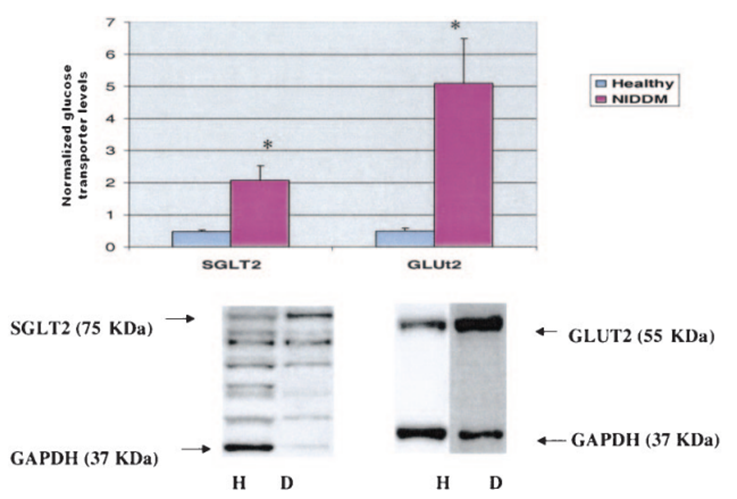
14) However, in #T2D, pathological maladaptations lead to an 🔼 renal threshold for glucosuria. This may be due to chronic 🔼 plasma glucose filtration leading to an adaptive 🔼 expression of SGLT2 and therefore 🔼 reuptake capacity and activity.
See 🔓doi.org/10.2337/diabet…
See 🔓doi.org/10.2337/diabet…
15) By blocking SGLT2, glucose remains in the tubular lumen, leading to vibrant glucosuria.
See 🔓doi.org/10.2337/dc13-0…
See 🔓doi.org/10.2337/dc13-0…

16) This medication class was developed and better understood thanks to work related to #phlorizin, a compound found in the root bark of 🍎🍏trees known to cause glucosuria, and the rare genetic disorder familial renal glucosuria. See 🔓doi.org/10.2337%2Fds16… 
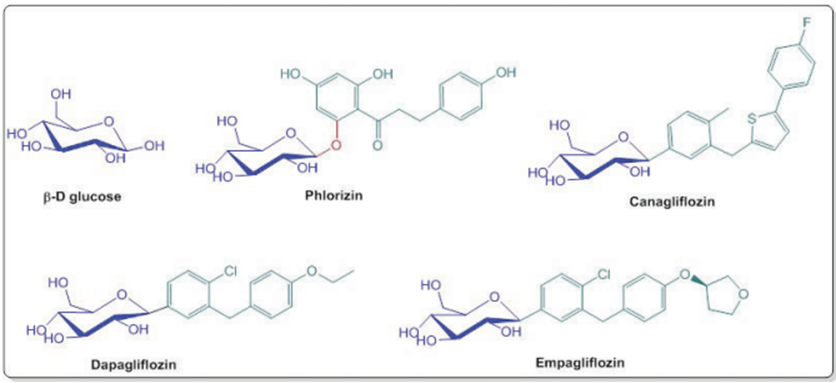
17) There are 4 SGLT2i’s commercially available in the United States (in alpha order, #canagliflozin, #dapagliflozin, #empagliflozin, & #ertugliflozin). Other agents are beyond the scope of this tweetorial. They also come in combos with #metformin and/or #DPP4 inhibitors.
18) Now a quick poll: How much #A1c lowering can be expected from this class?
19) Mark your best answer and return TOMORROW for the correct response and a link to your 🆓CE/#CME! 👍 @ChristosArgyrop @ShelleyZieroth @rajeshjain @DrMetabolism @SethShayMartin @didemturgut_ @GoggleDocs @MedTweetorials #FOAMed #CardioTwitter #endotwitter #NephTwitter
20) Welcome back! I am @tmodarressi, we are discussing standards of care for treating #T2D with #SGLT2i's, and YOU are earning 🆓CE/#CME! 

21) So as to yesterday's quiz . . . you DID answer, right? If not, scroll back ⬆️to tweet 18 and tell me how much #A1c lowering can be expected from this #SGLT2i therapy in patients with #T2D?
22) It's B: In general, these agents show modest improvements in A1c, approximately 0.6-1.0%, and are overshadowed in potency of glycemic control by #GLP-1 receptor agonists (such as #semaglutide and #dulaglutide).
doi.org/10.7326/0003-4…
doi.org/10.7326/0003-4…
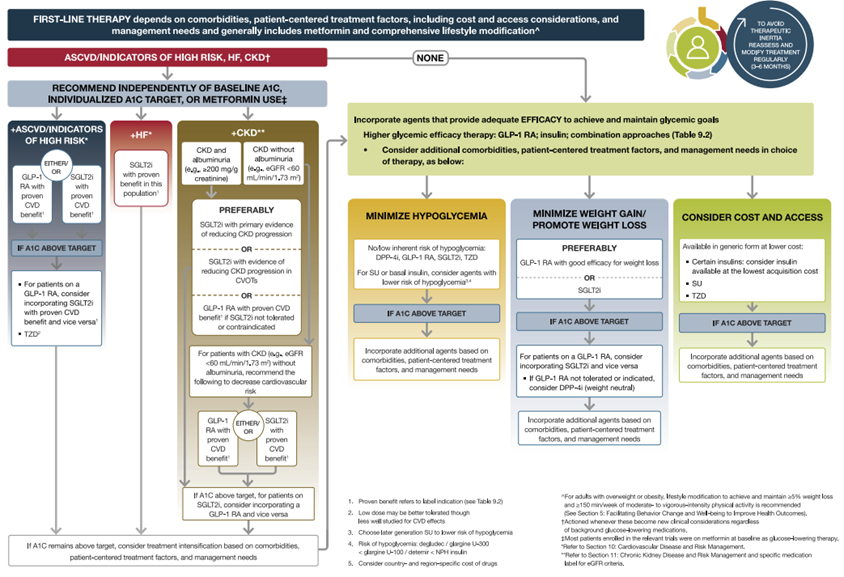
23) Over the years, however, we have seen a prioritization of this class due to pluripotent benefits outside of glycemic control. Compare the 2015 and 2022 @AmDiabetesAssn pharmacologic approach charts below.
See doi.org/10.2337/dc22-S…

See doi.org/10.2337/dc22-S…
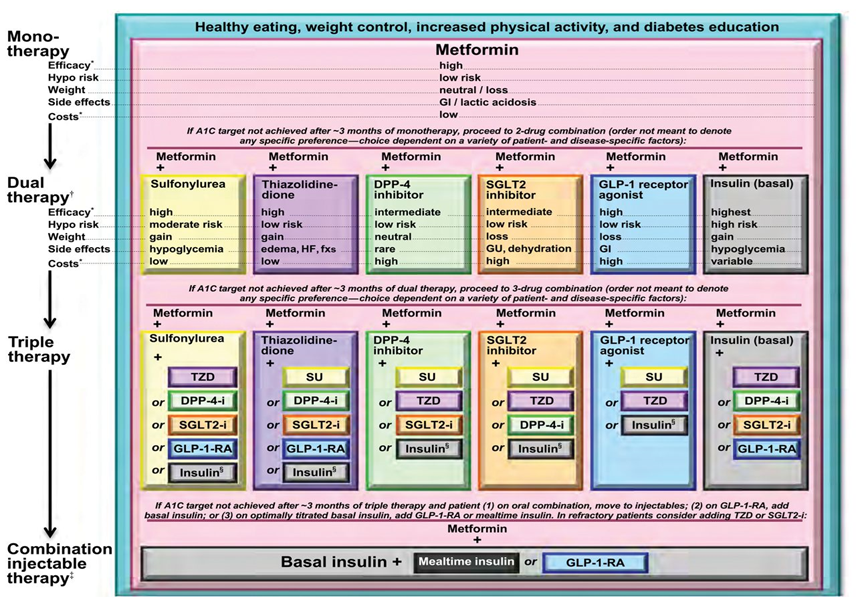
24) Several large studies have cast doubt on the effectiveness of preventing #macrovascular risk by forcing #A1c lower and lower. Our newer approaches and standards have a heavy focus on *how* we lower sugars rather than just to what level we lower to.
25) #SGLT2i have 2 critical benefits over some older med classes: they do not cause hypoglycemia & they do not cause weight gain (they typically promote mild weight loss, which helps w/the adiposity-driven pathophysiology of many patients with T2D).
See 🔓doi.org/10.2337/dc22-S…
See 🔓doi.org/10.2337/dc22-S…

26) A critical statement has been added to @AmDiabetesAssn guidelines in recent years, highlighted below, as studies have shown various #cardiometabolic benefits of #SGLT2 receptor inhibition regardless of baseline glycemic control. 

27a) Some guidelines such as those of @TheAACE (🔓doi.org/10.4158/CS-201…, left below) and joint @escardio/@EASDnews ( 🔓doi.org/10.1093/eurhea…, right below) even directly suggest #SGLT2i use . . . 

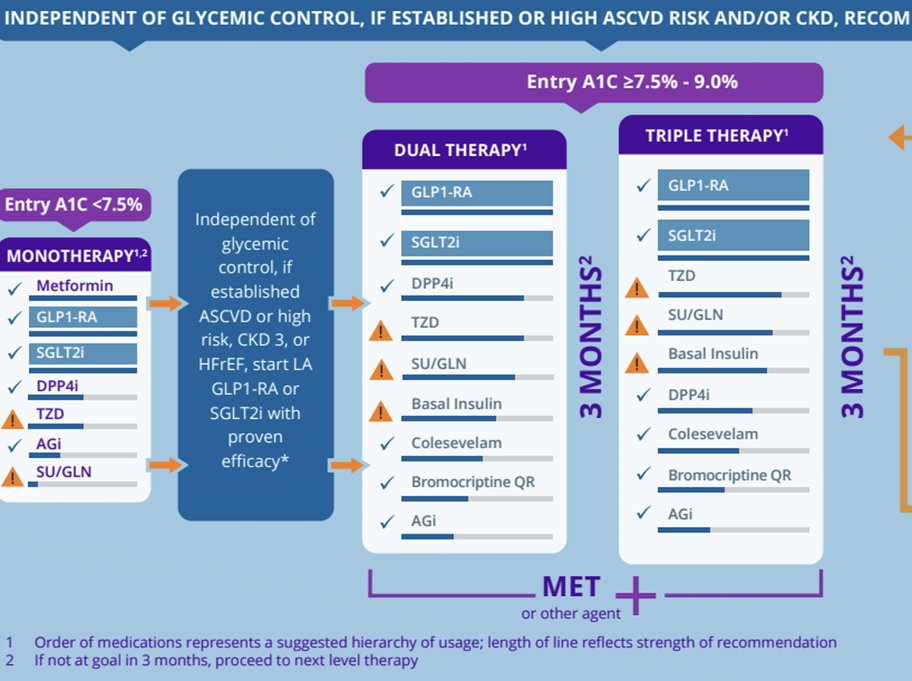

27b) . . . as first-line monotherapy in appropriate patients (although in the US many insurers will require metformin use or a documented reason why metformin cannot be used in order to approve).
28) The recently published AHA/ACC/HFSA heart failure guidelines also highlight this class with strong recommendations, as below (from 🔓doi.org/10.1016/j.jacc…): 
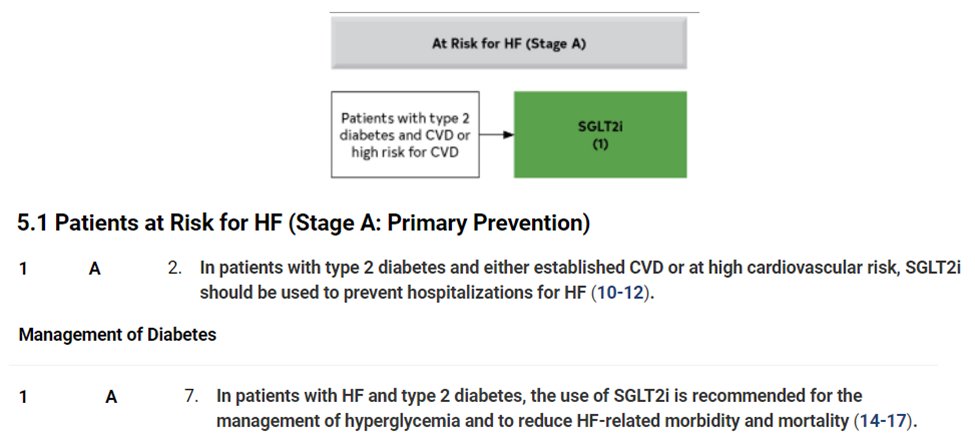
29) As we see in these practice guidelines, the use of #SGLT2i should be particularly prioritized in patients with or at high risk for #heartfailure, #CKD, or #atherosclerotic #cardiovascular disease.
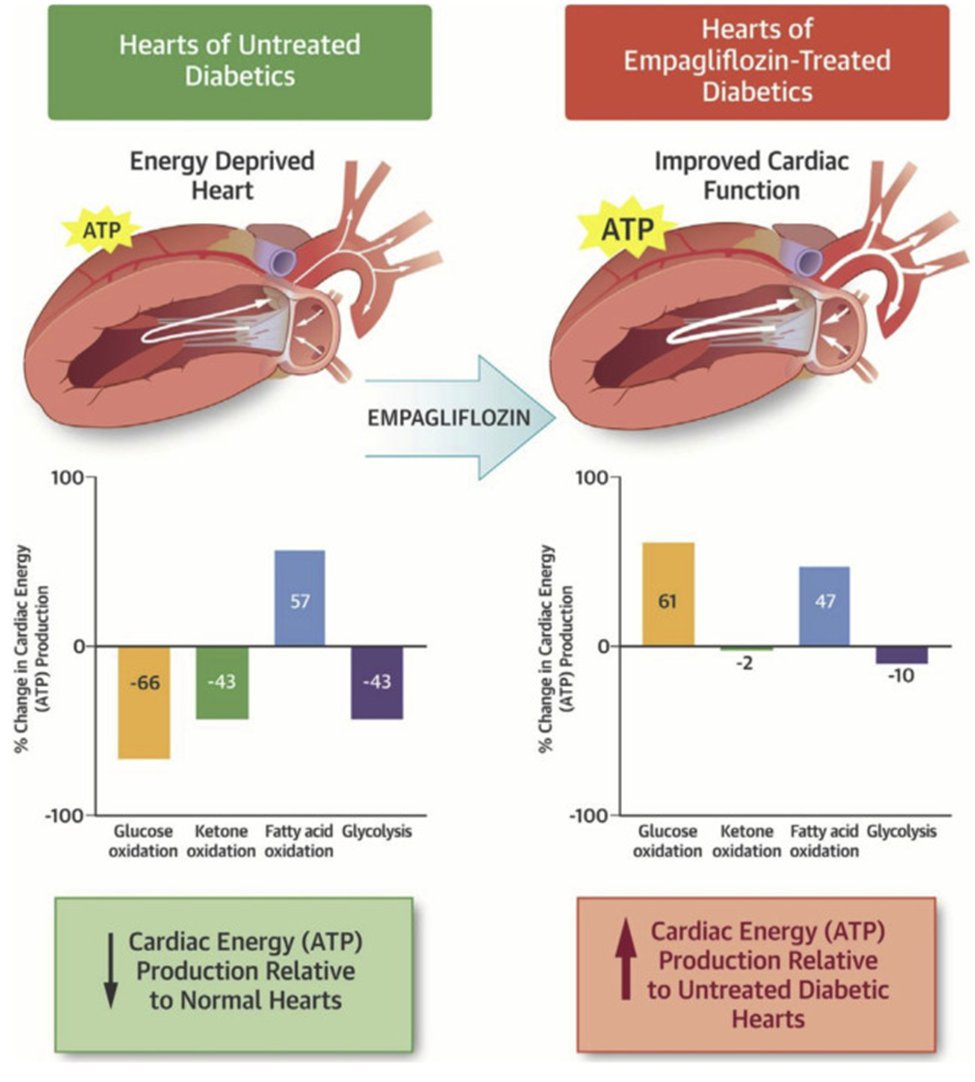
30) The impact of SGLT2i on each of these disease states has been discussed in other tweetorials (see tweet 4), and is summarized nicely in a recent NEJM article by cardiology legend Eugene Braunwald (tweet 3).
31) Again, the effects on these comorbidities are potent and largely *independent* of their effects on glycemic control. This is a critical point.
See 🔓 doi.org/10.1001/jama.2… (left) and 🔓doi.org/10.2337%2Fdc21… (right)

See 🔓 doi.org/10.1001/jama.2… (left) and 🔓doi.org/10.2337%2Fdc21… (right)


32) A poll to drive home the point: a patient with T2D, heart failure and CKD presents to you. A1c is 6.5%. Should you consider SGLT2i therapy?
33) How they work to reduce these risks is beyond the scope of this tweetorial, but here are some references to dive deeper below:
🔓doi.org/10.1016/j.jacb…
🔓doi.org/10.1007/s00125…
🔓doi.org/10.1161/HYPERT…



🔓doi.org/10.1016/j.jacb…
🔓doi.org/10.1007/s00125…
🔓doi.org/10.1161/HYPERT…



34) Full warnings are included in package inserts, but a few practical considerations in the next tweets:
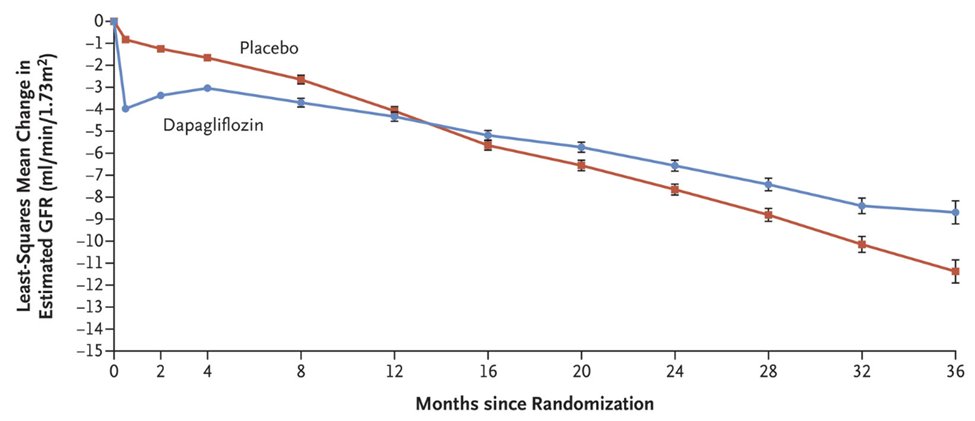
35a) 1. Soon after #SGLT2i initiation, there will be a dip in eGFR ⬅️mechanism of renoprotection of this class (similar to changes seen with #ACEi/ARB initiation). The magnitude of the dip varies, but has not been shown to be associated with safety concerns.
36) I @tmodarressi tend to follow the strategies outlined below by Drs. Hiddo Heerspink and David Cherney, two very well-known researchers in the SGLT2i world.
See 🔓doi.org/10.2215/CJN.02…
See 🔓doi.org/10.2215/CJN.02…

37) 2. There is generally no risk of hypoglycemia unless pt is on insulin, sulfonylurea or meglitinide. Hypoglycemia is NOT from SGLT2i but from the other agent. Consider downtitration of those agents, particularly if pt has reasonable glycemic control before SGLT2i initiation.
38) 3. Euglycemic #DKA is rare, but when it happens it is typically during extended fasts. Therefore, many clinicians will advise discontinuation a few days before surgery and skipping if experiencing upper GI illness or poor PO intake for other reasons.
🔓doi.org/10.2337/dc15-1…
🔓doi.org/10.2337/dc15-1…
39) 4. By promoting glycosuria, SGLT2i can potentiate genitourinary infections, particularly genital yeast infections. Patients should be counseled regarding signs and symptoms. Reconsider therapy in patients experiencing recurrent episodes.
doi.org/10.1177/106002…
doi.org/10.1177/106002…
40) So what may be next for the SGLT2i class strictly in the glycemia world? Intriguing data from the DAPA-HF trial (which enrolled patients both with and without T2D) showed a 32% reduction in the incidence of new T2D.
See 🔓doi.org/10.2337/dc20-1…
See 🔓doi.org/10.2337/dc20-1…

41) 🤔Could SGLT2i move even earlier in the #cardiometabolic health journey and be used in #prediabetes or insulin-resistant non-diabetes to start impacting health earlier?
42) Further, we know that many pts w T2D develop CV diseases at much younger ages (see the curves shifted left below). Can pushing tx into earlier phases of the pathophysiological life cycle preserve health and prevent these burdensome diseases?
(from 🔓doi.org/10.1016/S2213-…)
(from 🔓doi.org/10.1016/S2213-…)

43) Lastly, a plea: SGLT2i do not “belong” to anyone. Whether in endocrinology, primary care, cardiology, nephrology, etc, we are all responsible to our pts for using this class appropriately. SGLT2is may be the single most important and pluripotent medications of a generation.
44) And that's it! You just earned 0.5hr CE/#CME! Go to cardiometabolic-ce.com/cardiorenal21/ and claim your certificate! And follow @cardiomet_ce and @ckd_ce for the BEST continuing education on Twitter from expert authors! I am @tmodarressi. Thanks for joining!
• • •
Missing some Tweet in this thread? You can try to
force a refresh