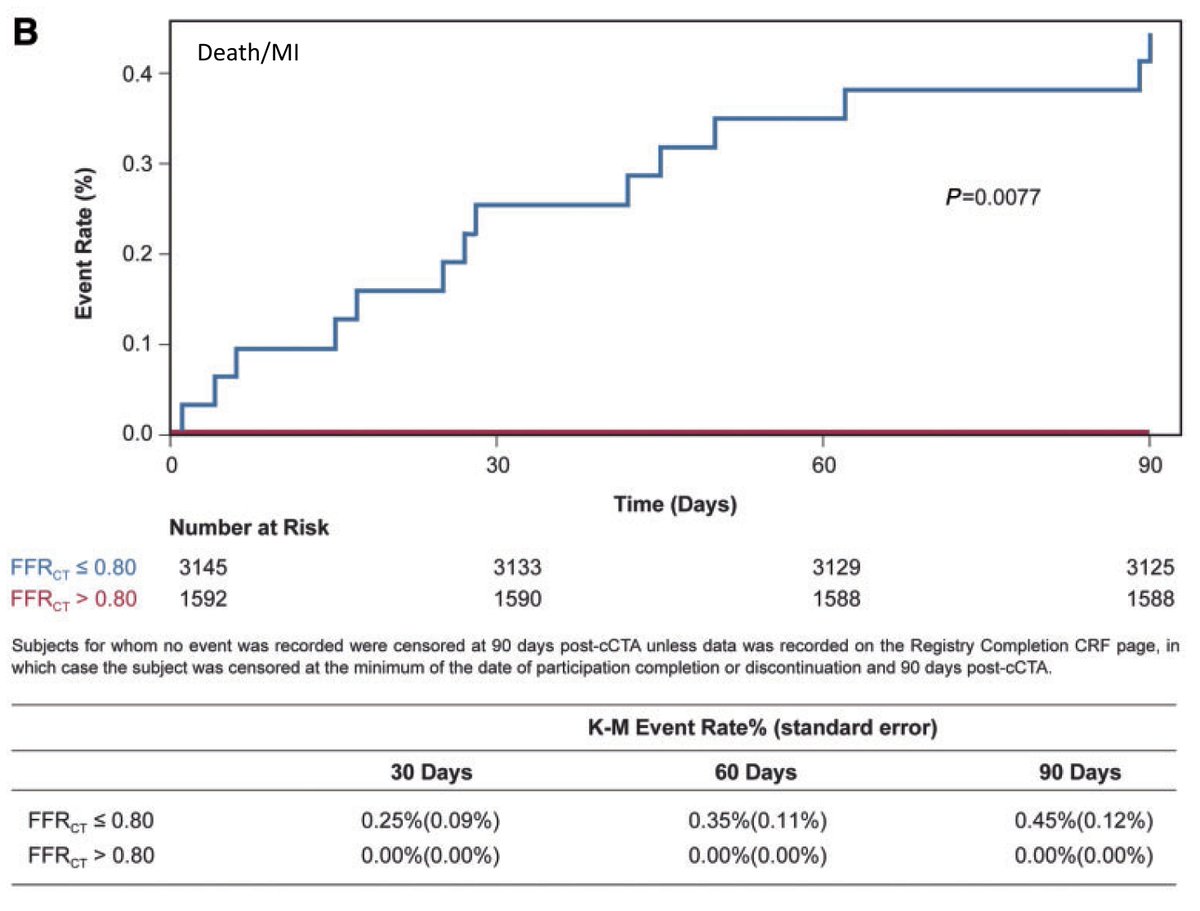
But who is right?
(A little better for LCx and RCA but only a bit.)
But even worse, I’m pretty sure they are analyzed and/or reported incorrectly.
This is surely much more revolutionary! VCs, load up the truck for @HeartFlow stock!
@DShaywitz
This has to be play of chance.
(A) Yes! CT-FFR Rulez, Venk droolz
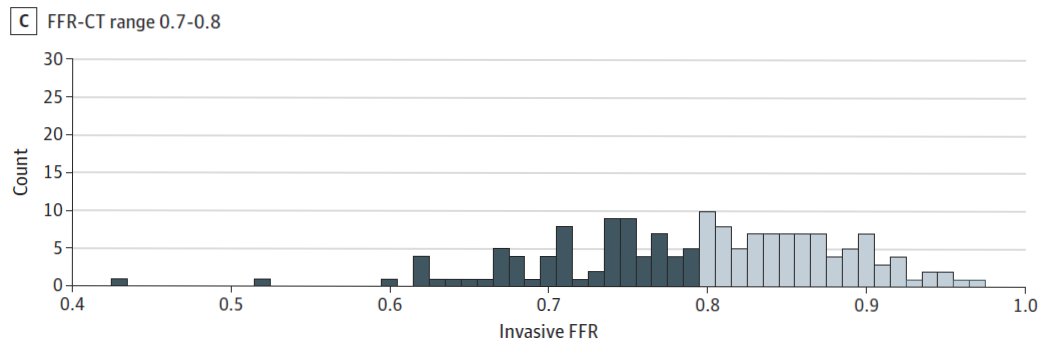
(B) Not so sure
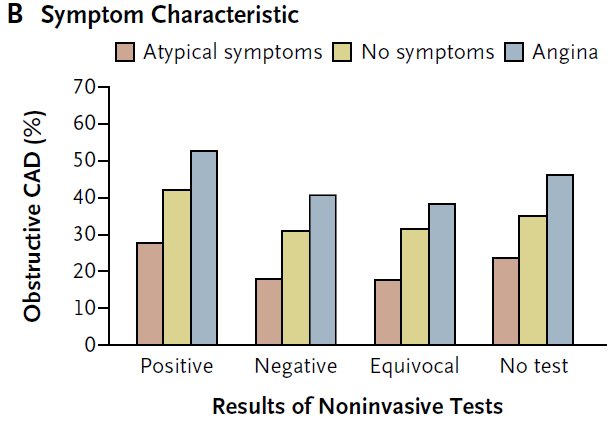
(C) Probably rushed
(D) Never
This really should be evaluated in a trial.
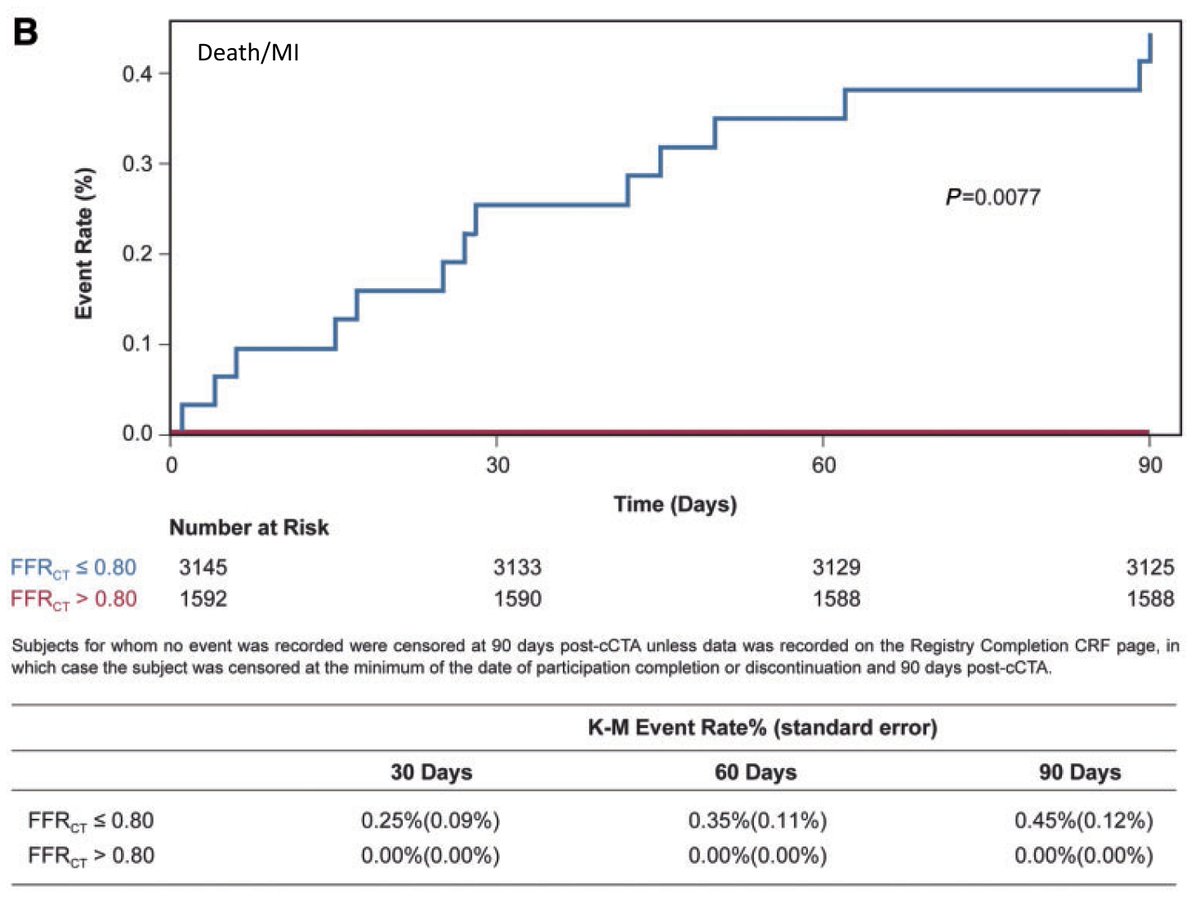
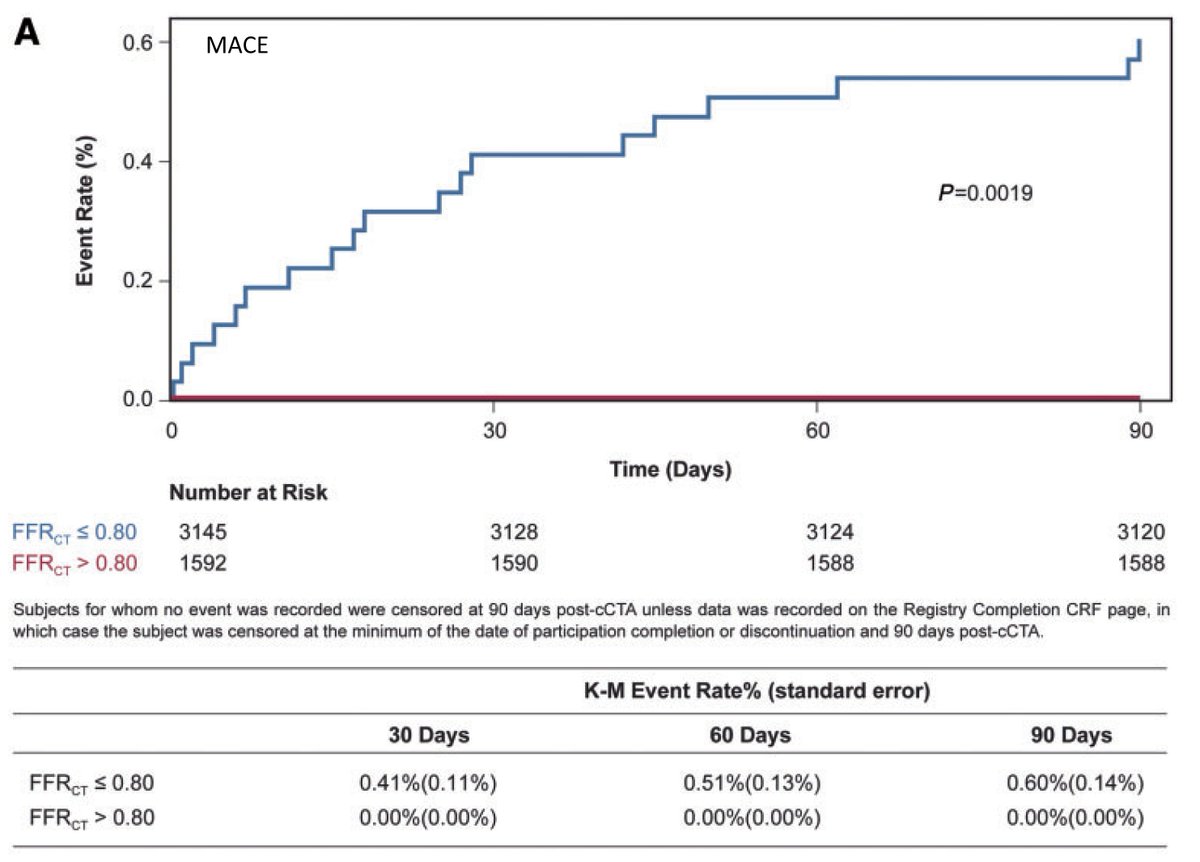
But all the other points about driving treatment decision making remain and become even more funny when the event rate in the supposedly sick group is extraordinarily low.