Recall that, in general:
BP = CO x SVR
BP = [HR x SV] x SVR
BP = [HR x [ESV-EDV]] x SVR
Imagine someone has been on a thiazide for 12 months. Which of these factors is affected, leading to lower BP?
Initially, thiazides induce a diuresis (via the block of the Na/Cl cotransporter in the kidney). Result:
⬇️ venous return
⬇️ end-diastolic volume
⬇️ stroke volume
⬇️ cardiac output
⬇️ BP!
Note that this causes an INCREASE in SVR (via RAAS activation)
ncbi.nlm.nih.gov/pubmed/13811661
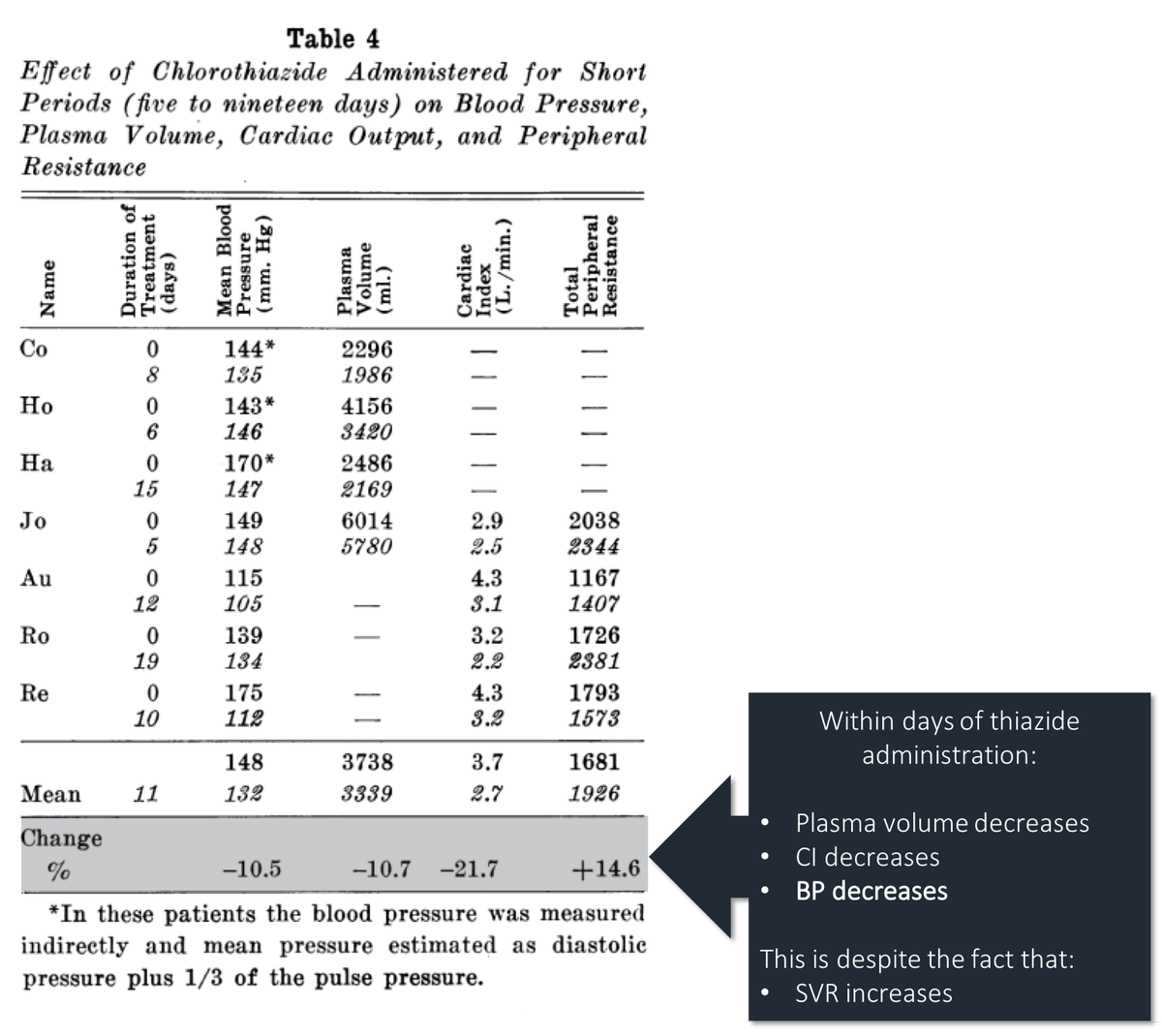
More proof that the initial drop in BP is related to a decrease in plasma volume and resulting drop in stroke volume and cardiac output:
If you co-administered IVF with thiazides, you blunt BP-lowering effect.
ncbi.nlm.nih.gov/pubmed/13666018
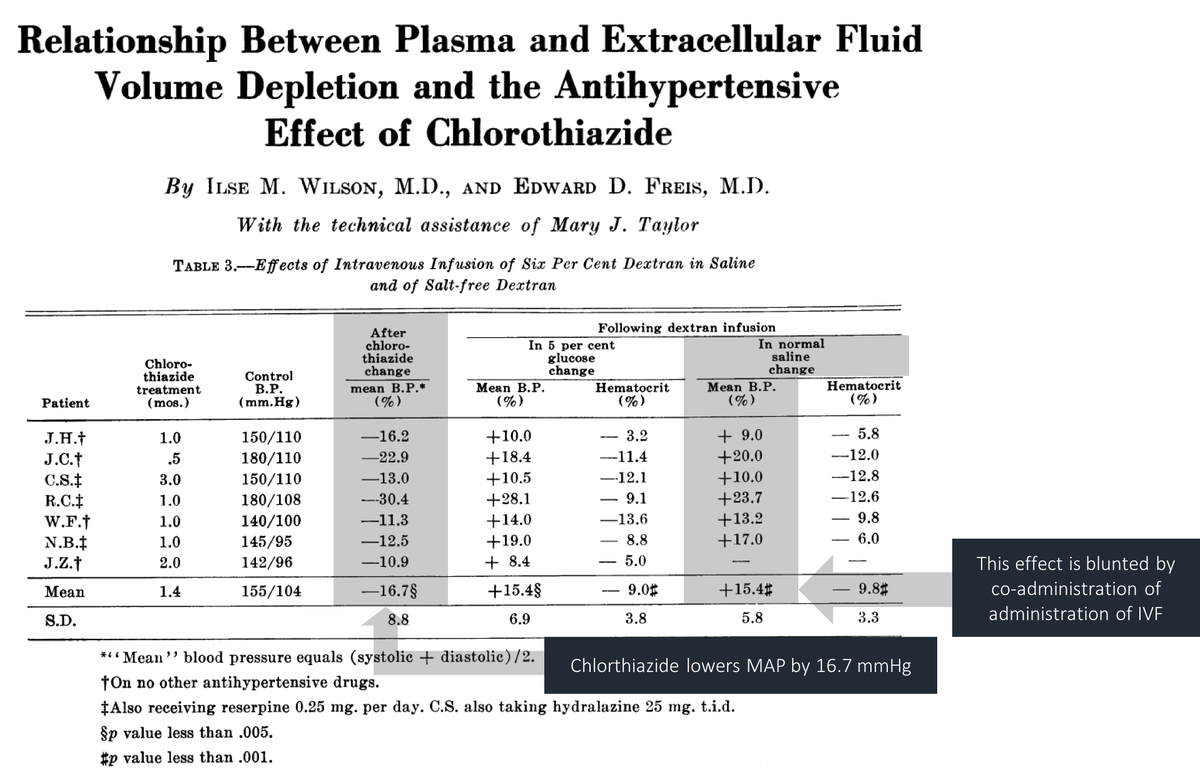
So, in the short-term, it appears that a decrease in CO (via decreased EDV) is the main mechanism by which blood pressure decreases. The BP falls, even though SVR increases.
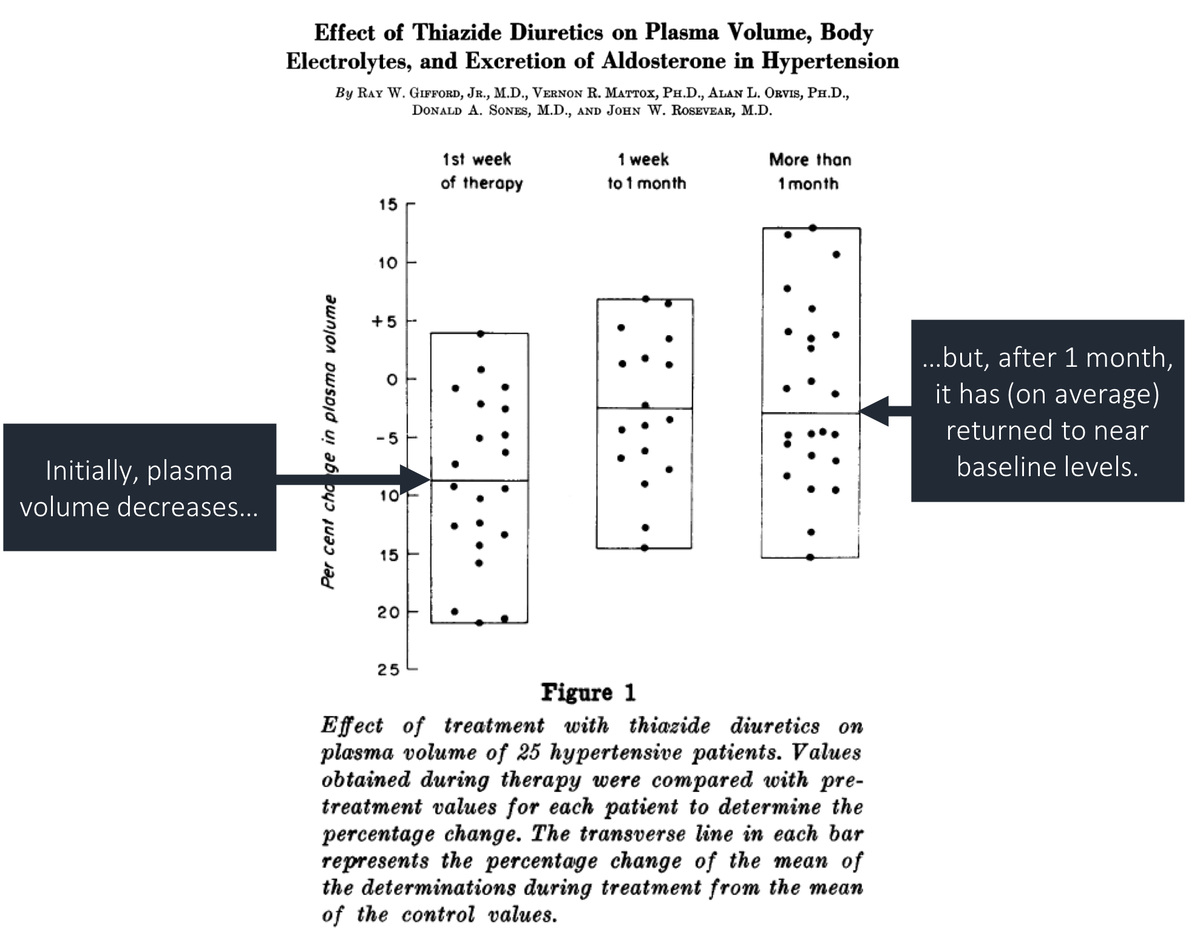
But, what if we look at patients chronically taking thiazides? Is their CO still below baseline?
Although plasma volume initially falls, after remaining on a thiazide for weeks to months, it returns to near baseline levels.
What would this do to EDV and CO?
ncbi.nlm.nih.gov/pubmed/13898487
Interestingly, there appear to be different CO and SVR changes in those who respond to chronic thiazide use versus those who don't respond.
Responders show a:
⬆️ CO
⬇️ SVR
This suggests that chronic BP control is due to lower SVR (and not lower CO)!
ncbi.nlm.nih.gov/pubmed/6987024
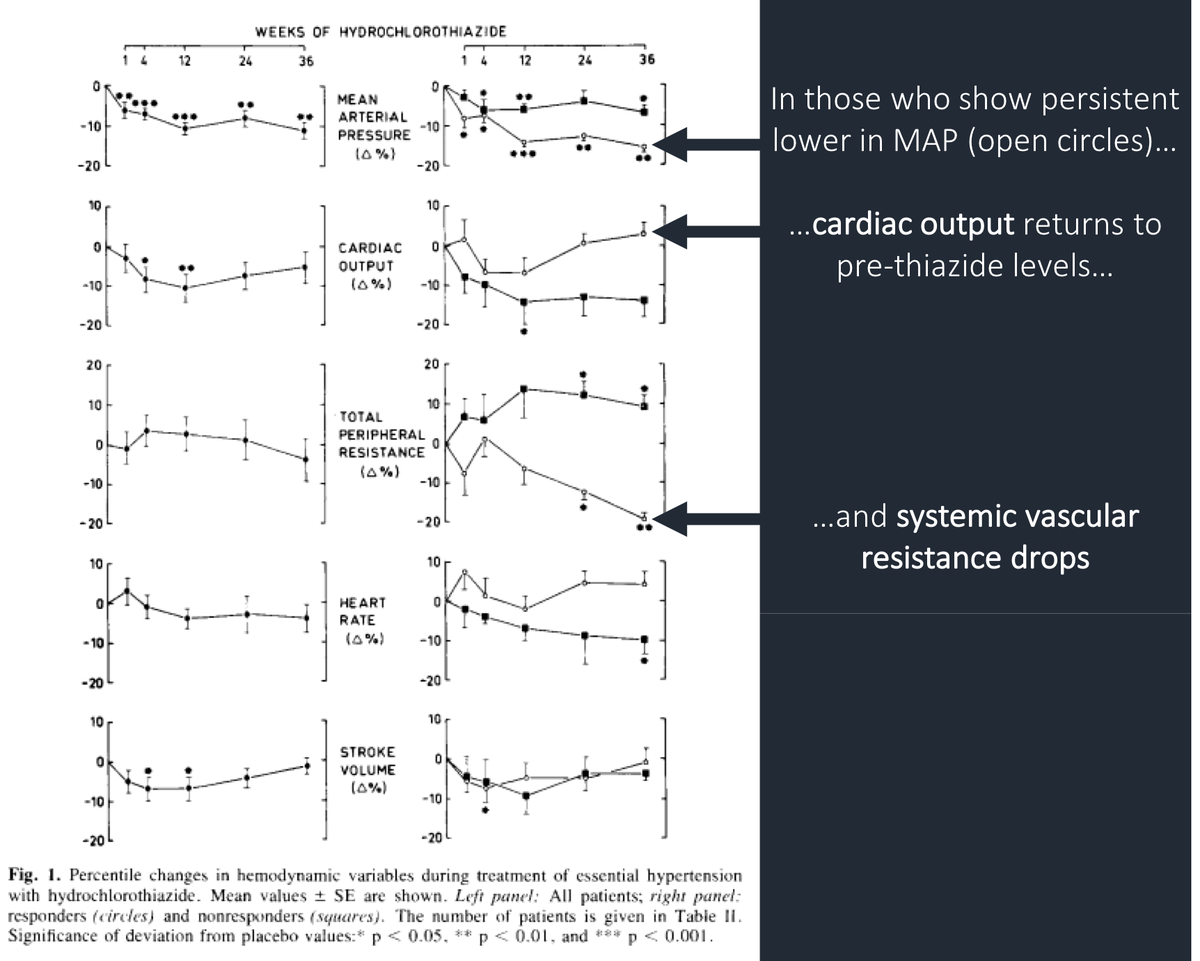
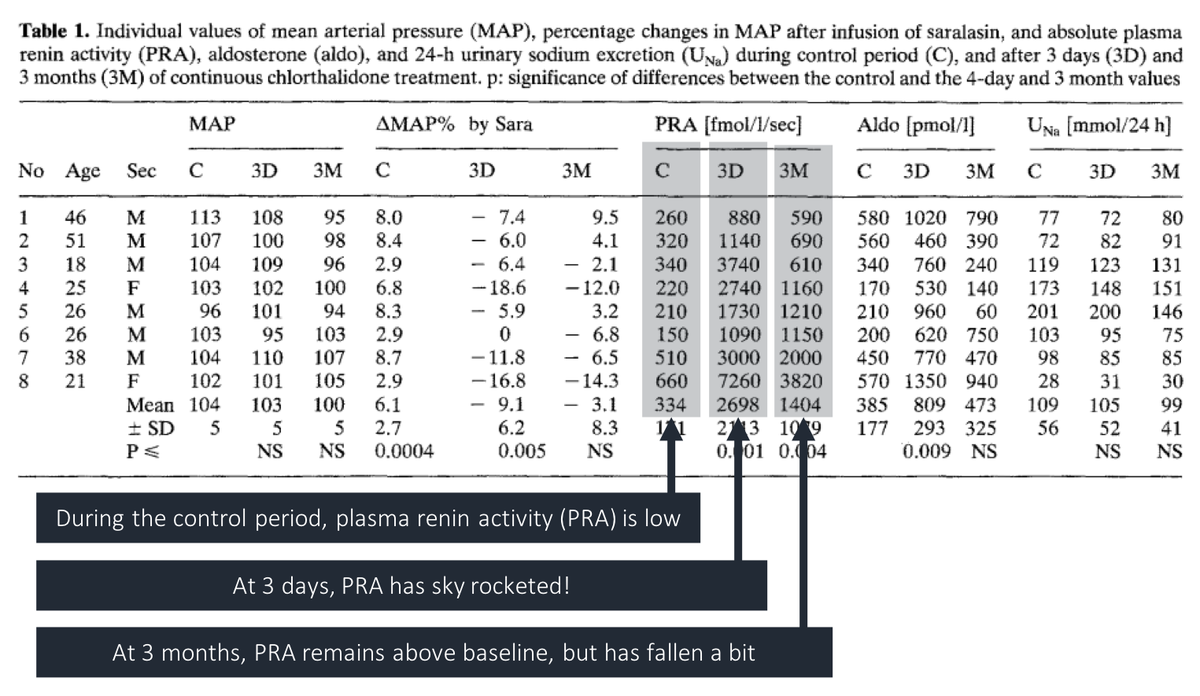
What's also interesting is that the SVR decreases despite persistently elevated renin levels.
So, if a decrease in SVR is what leads to long-term BP control, it doesn't seem that "de-activation" of RAAS is the only factor.
ncbi.nlm.nih.gov/pubmed/7202469
Interim Summary:
In the short-term, thiazides lower BP via diuresis and resulting:
⬇️ PV
⬇️ CO
But, eventually, patients see:
⬆️ PV and CO to near-normal
⬇️ SVR
Our next step: explain the decrease in SVR...
Many hypotheses have been offered to explain the decrease in SVR in chronic thiazide use:
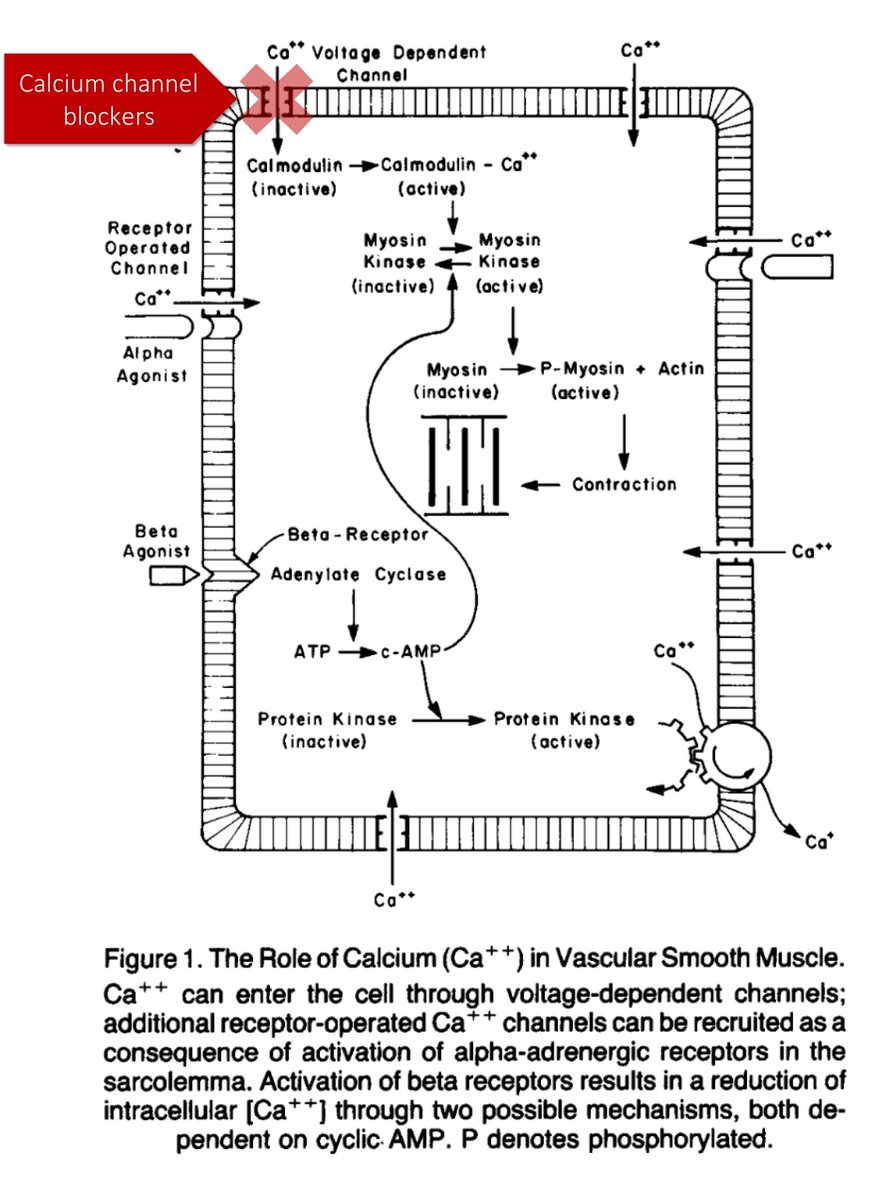
*opening of Ca-activated potassium channels
*decreased release of endogenous digitalis-like factor
*reverse autoregulation
I'll discuss the first two.
In one study, HCTZ was injected directly into the brachial artery. Investigators saw a decrease in blood pressure.
But, this decrease was blunted by tetraethylammonium, a known blocker of large-conductance calcium-activated potassium channels (KCa).
ncbi.nlm.nih.gov/pubmed/9856976
These results suggest that thiazides open KCa channels causing:
*membrane hyperpolarization
*reduction in intracellular calcium
*vasodilation (i.e., decreased SVR)
ncbi.nlm.nih.gov/pubmed/1373909
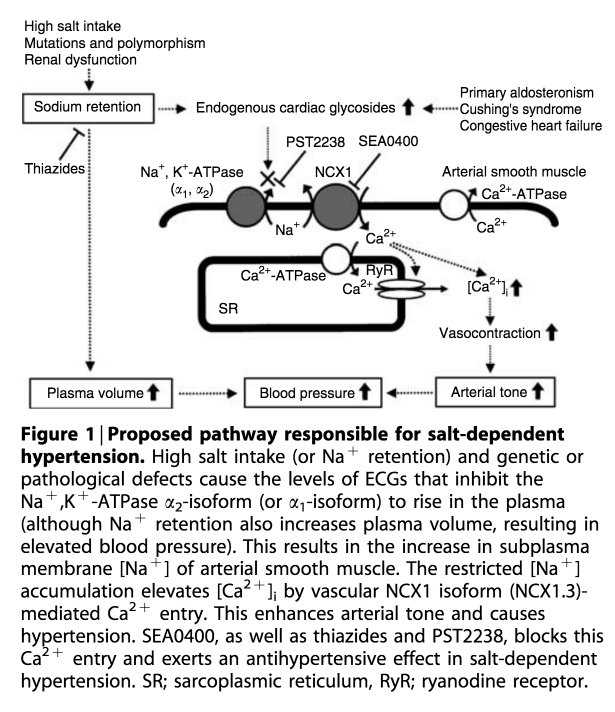
An alternate theory suggests that thiazides decreased the release of endogenous digitalis-like factor. This would lead to:
⬆️ Na-K-ATPase activity
⬇️ intracellular [Na]
⬇️ intracellular [Ca]
⬆️ vasodilation
⬇️ decreased SVR
⬇️ decreased BP!
ncbi.nlm.nih.gov/pubmed/16641927
Before closing, let's ask our original question.
Imagine someone has been on a thiazide for 6 months. Which of these factors is affected, leading to lower BP?
Amazingly, even though thiazides have been around since the 1950s, we still don't know how exactly they lower blood pressure. Our best theories:
Short-term: ⬇️ CO (via decreased PV/EVD)
Long-term: ⬇️ SVR
How exactly SVR is decreased remains a mystery. At least to me.
The blood pressure equation should read:
BP = [HR x [EDV-ESV]] x SVR
Thanks to @saul03 and @strauss_matt for pointing out that I had swapped EDV and ESV.