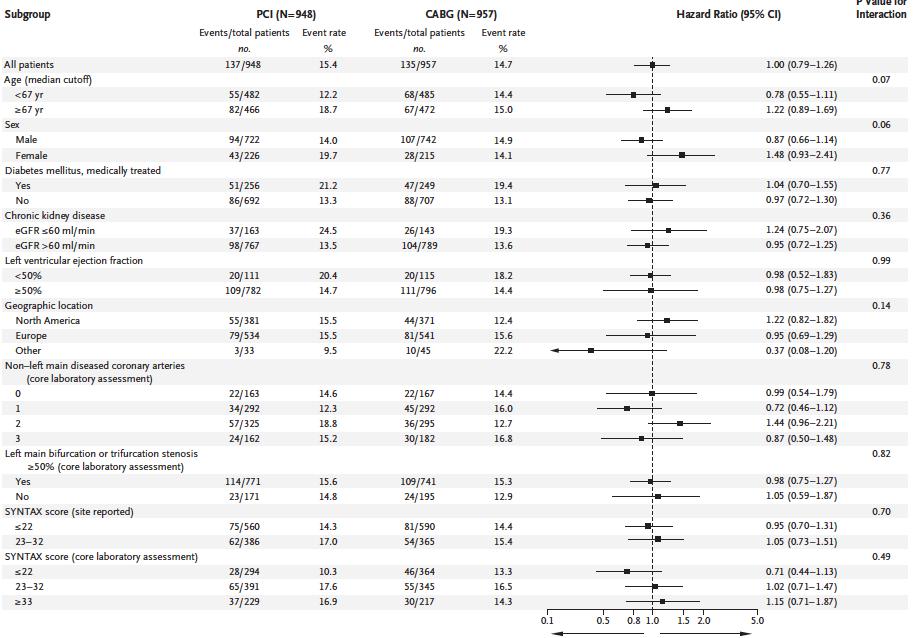
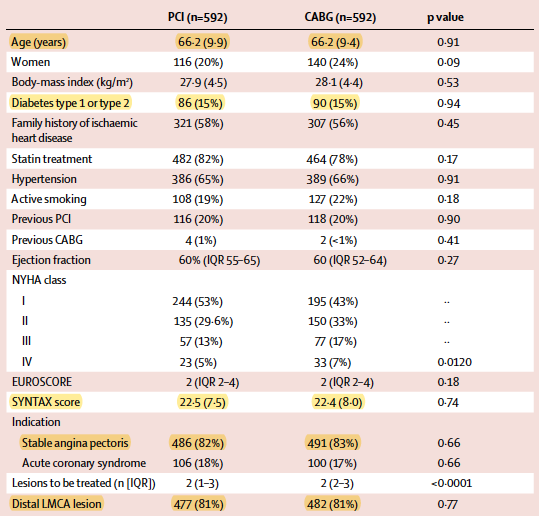
1. LM >70% visually, or >50% hemodynamically significant
2. Heart team suitable for both Tx
3. SYNTAX score <32
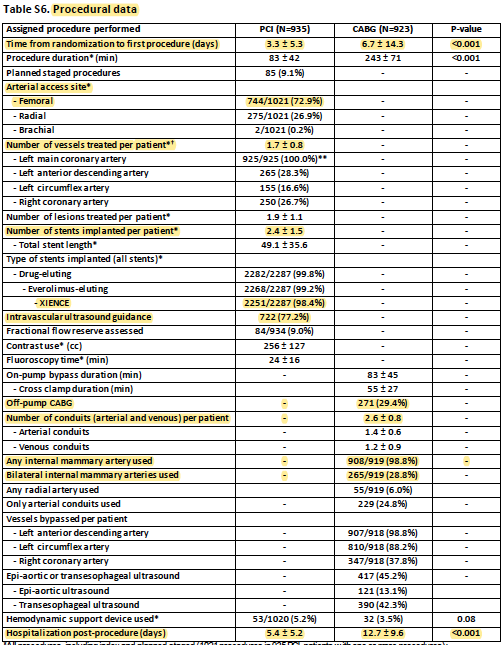
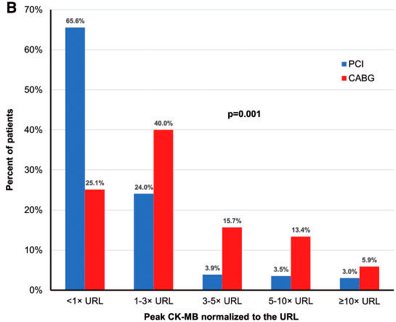
#PCI: #RadialFirst only 26.9%, 1.7 vessesls Tx, 2.4 stents, DES 99.8%, IVUS 77.2%. hospital stay 5.4 d
#CABG: off-pump 29.4%, 2.6 grafts, IMA 98.8%, BIMA 28.8%, 24.8 arterial only. hospital stay 12.7
1. 1/4 actually had high SYNTAX score with core lab
2. 3-year, although not short, longer is preferred for more definitive conclusions
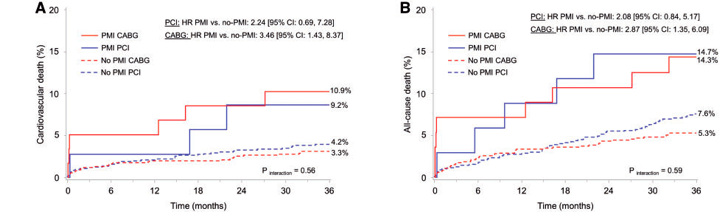
3. Definite non-CV death higher in PCI group, while CV death similar, bad luck?
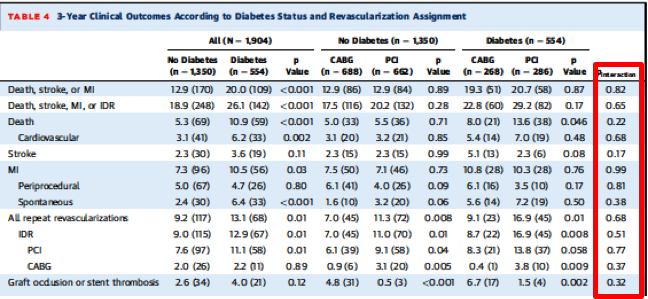
1.Repeat revasc in primary outcome: revasc far way less patient-important than death-stroke-mi, and many other methodological aspects favoring CABG
2.Periproedural MI (even large) likely missed (not systematically measured)
3.Frist gen DES used in some patients
Now on, a few key articles...
1. Heart team (minimum: clinical card, surgeon, and IC)
2. Shared decision making: involve the patient in the discussion and incorporate values and preferences
3. Be aware of ur center results (CABG and PCI) for RCT external validity