1/
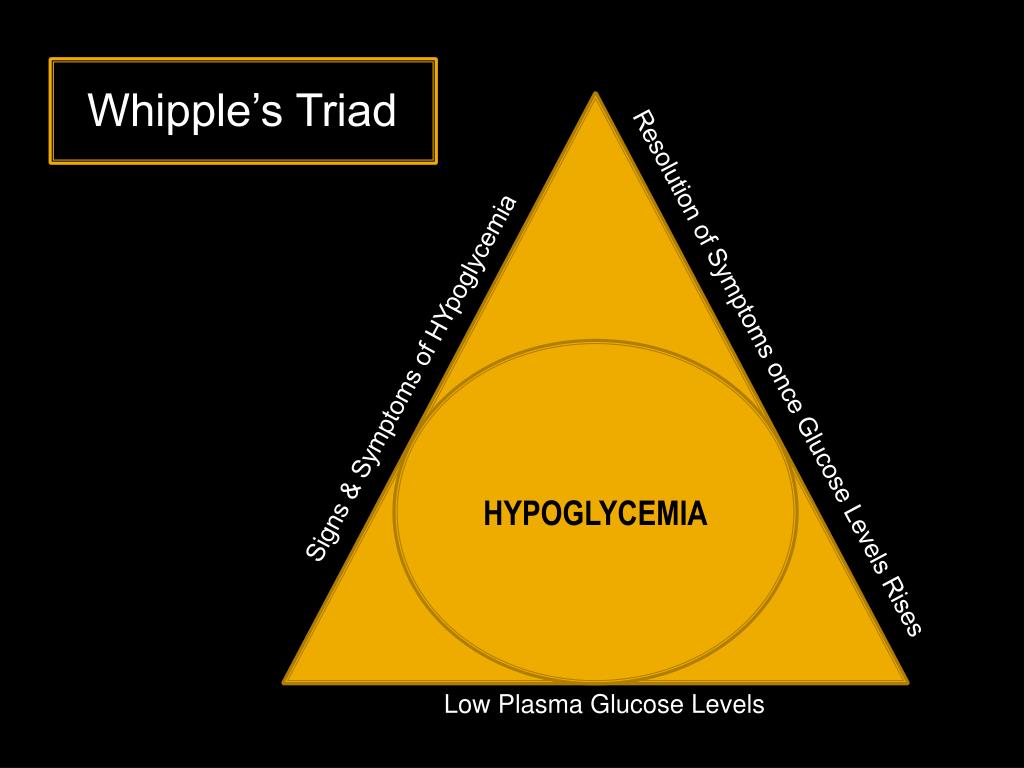
Eponyms are falling out of favor in medicine. They aren't descriptive and essentially require twice the memory space to recall both the name & the associated term.
But pancreaticoduodenectomy doesn't exactly roll off the tongue so I suspect the Whipple is here to stay.
When I had to undergo the surgery myself two years ago @IntermtnMedCtr, I made the somewhat bizarre, deliberately exhibitionist request that the procedure be live-Tweeted so that the step-by-step process could be visualized for other patients contemplating the operation.
My surgeons graciously agreed to have the wonderful @intermountain social media team in the OR and they documented the events of the day sequentially, which you can revisit here: wakelet.com/wake/e82752c4-…
I am so grateful to have this documentation, both for my own surreal out-of-body experience but much more so for the demystification of a much-feared procedure.
I firmly believe that knowledge empowers patients and can dispel at least some of oncology's anxious uncertainty.
To be clear, this surgery is not to be taken lightly.
Dr. Whipple died in 1963; over a half-century later, his namesake intervention still carries significant morbidity & mortality (I was cited a 3% risk of death, a number that loomed large the sleepless night before the op)
This @nejm study validates that the procedure is least risky when performed in a high-volume center, so it is entirely appropriate for patients to ask their operative team about caseload and outcomes:
nejm.org/doi/full/10.10…
And so, I do recognize the profound privilege I received on August 7th, 2017: a new lease on life and a forever-altered perspective on what it means to be a patient.
I send all those in the oncology community my sincere gratitude and solidarity.
oftumorsandmen.com/whipple-blog/2…