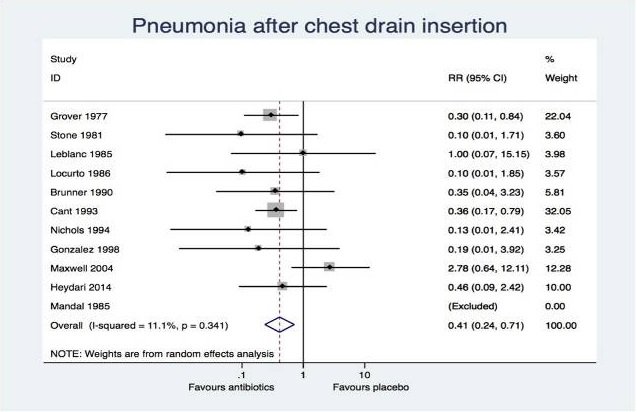
You assess a patient with a stab wound to the left chest in respiratory distress. Chest XR shows a large hemopneumothorax, and you insert a large-bore chest tube. Do you give antibiotics?
ctsnet.org/article/histor…
If antibiotics reduced infection by 75%, and infection incidence is 2.5%, what sample size do we need at a=0.05 b=0.2?
We'd need 1372 patients in our sample. So n=224 ain't cutting it.
You assess a patient with a stab wound to the left chest in respiratory distress. Chest XR shows a large hemopneumothorax, and you insert a large-bore chest tube. Do you give antibiotics?