My previous understanding of this diagnostic test was recently challenged and lends credence to the fascinating diversity of pleural effusions/dz.
(A #MedTwitter and #Tweetorials contribution).
Initial pleural fluid studies:
protein <0.8 LDH 2300 glucose 278 RBC 400 WBC 17.5k trigs 204 cholesterol 225 chylomicrons (-)
What type of effusion is this?
1.Pleural fluid hematocrit (hct) >50% peripheral hematocrit
2.RBC/100,000 (estimate for pleural fluid hct if not obtained) >50% peripheral hct
TF = tube feeds
Review of chylothorax management:
academic.oup.com/ejcts/article/…
Circ = circulation
Absorb = absorption (from enterocytes)
Triglycerides >100 AND ⬆ chylomicrons (gold standard).
- ⬆ amylase
- ⬇ pH
- multiple pathogens on pleural fluid culture
- Triglycerides can be elevated in setting of esophageal perforation depending on PO intake
Let’s go over a few learning points:
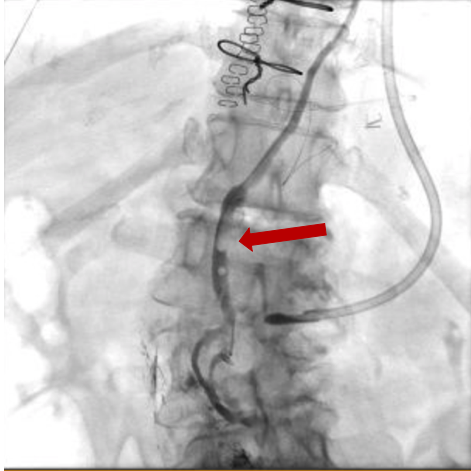
3/ Low-fat TF’s + octreotide are often successful conservative management, but if chylous output >500cc daily, may require TD embolization/ligation
4/ Chylothoraces are RARELY infected and if multiple pathogens on pleural fluid culture -> suspect esophageal perforation
Thanks for reading! #FOAMed #MedEd
@thecurbsiders, @DoctorWatto: new episode idea -> pleural disease diagnosis/simple mgmt. Malignancy vs infection vs alternative. Fascinating diagnostics and management!