ACUTE SKIN GRAFT-VERSUS-HOST DISEASE:
A #tweetorial/#medthread on this complication of stem cell transplantation!
#MedEd #FOAMEd #dermtwitter #onctwitter #medtwitter #dermatology #dermatologia pc:@dermnetnz
1st, a poll:
How do you differentiate acute & chronic skin #GVHD?
Acute vs. chronic GVHD is usually differentiated by when it occurs: before or after 100 days since allogeneic stem cell transplant. BUT in the skin, MORPHOLOGY is key!
As with almost everything else in derm, start with the exam. That will tell you what you're dealing with!
Figuring out which one of the ddx is most likely is critical. If you think it's morbilliform drug, check out my old #tweetorial on the topic!
Viral exanthems are less likely (but don't forget to check the donor's status)
But what might tip you off that it's GVHD?
If you picked 1 OR 3, you're right! Acute GVHD, as opposed to drug eruptions & viral exanthems, are usually follicular & acral, & then spreads toward the center.
Check out my acral rash #tweetorial for more details on this!
But if it's severe and stage IV, acute skin GVHD can mimic SJS/TEN. These patients need aggressive wound care, and we often treat for both since they're hard to differentiate!
My first ever #tweetorial on SJS/TEN here:

So should we biopsy? While it's often done, my own practice is not to as the #dermpath findings aren't a slam dunk (and it doesn't change mgmt!). Because acute GVHD involves the follicles, the #pathology correspondingly involves the acrosyringium in GVHD, but it's not perfect.
What are other unique eruptions in the SCT population to think about?
Remember that you could also consider:
- Engraftment syndrome (usually btw day +9 to +16, & with fever & pulm edema etc).
- Eruption of lymphocyte recovery (corresponds with re-expansion of lymphocyte pop).
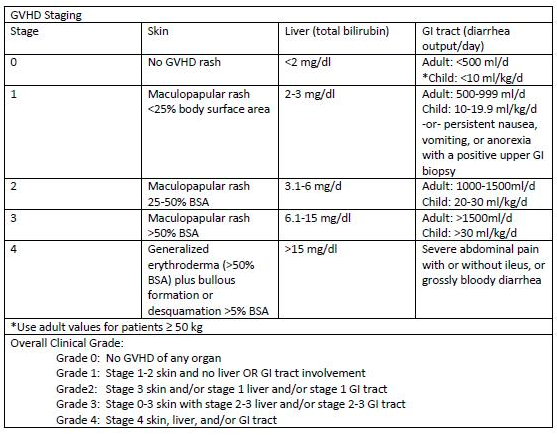
A reminder that acute skin GHVD doesn't always happen alone! These are the patients that require a check of liver enzymes and diarrhea frequency, to see if liver or gut GVHD is also playing a role!
Notice how stage IV skin = grade IV GVHD?
Table from: cancertherapyadvisor.com/home/decision-…
But how do you treat these patients? Depends on the stage.
If it's stage IV, we're reaching for immunosuppressants and IVIG, in hopes that we can treat the GVHD or SJS/TEN, whichever one it may be. These patients are so sick, we're throwing the kitchen sink at them.
If stage I-III, I'll reach for topical steroids. I'm reticent to recommend systemic steroids, since I also don't want to blunt any possible graft-versus-leukemia/lymphoma (GVL) effect!
My #tweetorial on topical steroids for reference:
Of course, systemic immunosuppression may be required if the skin is progressing, is severe, or if other organs are involved. Collaborating with #oncology is key since the details of the patient's transplant history are critical in weighing the risks/benefits!
Let's recap:
👉Acute vs. chronic skin GVHD is based on morphology, not timing.
👉 Acute GVHD starts acrally, moves in, & is follicular.
👉Acute skin GVHD usually morbilliform, or TEN-like when stage IV.
👉 Biopsy not usually helpful.
👉 If not stage IV, treatment is topicals.
Thus concludes our #tweetorial/#medthread on Acute cutaneous GVHD! Feel free to comment/add more below Hope this helps some of you out there who might care for these patients in the future!