A standard refrain for subspecialists, but one that often generates significant stress on both ends of the call.
Why?
Q: If you have ever felt anxiety about calling a consult, what was the cause of most of your stress?
Thus, collegial and effective consultation is essential.
pubmed.ncbi.nlm.nih.gov/6615097/
This is the HOW of consultation.
In this context, past efforts to help learners prepare for consults fell into 2 categories:
1-Strategies to systematize REQUESTING of consults (5Cs, CONSULT, PAGE)
2-Strategies to systematize RESPONSE to consults (see last Tweet)
Frameworks for ‘types’ of consultation do exist:
Kessler et al. 2013 – pubmed.ncbi.nlm.nih.gov/23017469/
Hale et al. 2019 – pubmed.ncbi.nlm.nih.gov/30768469/
As an educator interested in #TeachDx, I’ve been reflecting on how subspecialists contribute to a case from a reasoning perspective.
The goal? A universal conceptual framework for ‘subspecialty reasoning’.
For instance, it could help us better define:
a) the way consults are requested and performed
b) how to assess and coach subspecialty trainees
c) metrics of high-quality subspecialty care
pubmed.ncbi.nlm.nih.gov/31577583/
It would be a natural next step to extend this focus to subspecialty training.
@MikeMeliaMD @EmilyBlumbergMD
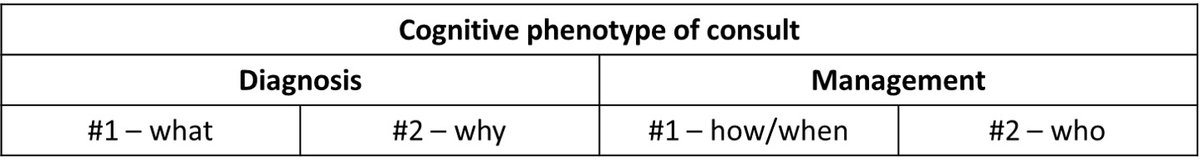
Let’s start with what we do – consults – & generate a paradigm for the 'phenotypes' of cognitive ‘asks’ we get.
This effectively transfers the burden of generating a ‘consult question’ from the consulting team *to the consultant.*
These are cases without an established dx whose ultimate dx may/may not be within the consultant’s domain – i.e. non-specific abnormalities. The consultant must answer: WHAT is the dx?
In ID: Fever + ____. Unexplained eosinophilia. Leukocytosis.
These are cases w/ an established dx in the consultant’s specialty – syndrome + confirmatory test – whose pathogenesis hasn't been fully defined. The consultant must answer: WHY this dx (or is there another dx)?
In ID: Bloodstream infxns. OIs.
Cases w/ established dx & pathogenesis but uncertain Rx plan. The consultant must consider 3Ts – time/test/treat – thresholds to guide best next step.
In ID: BSI in pt w/ ICD. Immunosuppression in pts w/ OIs. Infxn in tough to sample site.
The issue is ownership. The consultant must ‘own’ short-term care of the pt b/c of unique access to an intervention (procedure, restricted drug, etc.) OR must 'own' the long-term care of the pt.
In ID: new dx of HIV, OPAT, undifferentiated FUO.
So what’s the point?
Being meta about consults in this way can help us:
1-be explicit about a subspecialist’s cognitive input
2-assess/coach subspecialty trainees
3-reimagine how to request consults
Dx Probs #1 – domain-specific schemas/illness scripts
Dx Probs #2 – metacognition (what else is going on?)
Mgmt Probs #1 – navigating test/treat thresholds
Mgmt Probs #2 – metacognition (communicating uncertainty/commitment to f/u)
Dx Probs #1 – refining problem representation & DDx
Dx Probs #2 – avoiding bias (anchoring, premature closure, etc.)
Mgmt Probs #1 – developing test/treatment thresholds
Mgmt Probs #2 – communication skills
Dx Probs #1 – I’ve got sick pt & need help making a dx
Dx Probs #2 – I’ve got dx but want to ensure I'm not missing something
Mgmt Probs #1 – I’ve got dx & need help w/ best next step
Mgmt Probs #2 – I’ve got dx & need you to own the case
@ImproveDx @IMreasoning @rabihmgeha @DxRxEdu @tony_breu @sargsyanz @andrewolsonmd @thecurbsiders @JenniferSpicer4 @Amstrw @CarlosdelRio7 @gradydoctor @EmilyAbdoler @MDdreamchaser