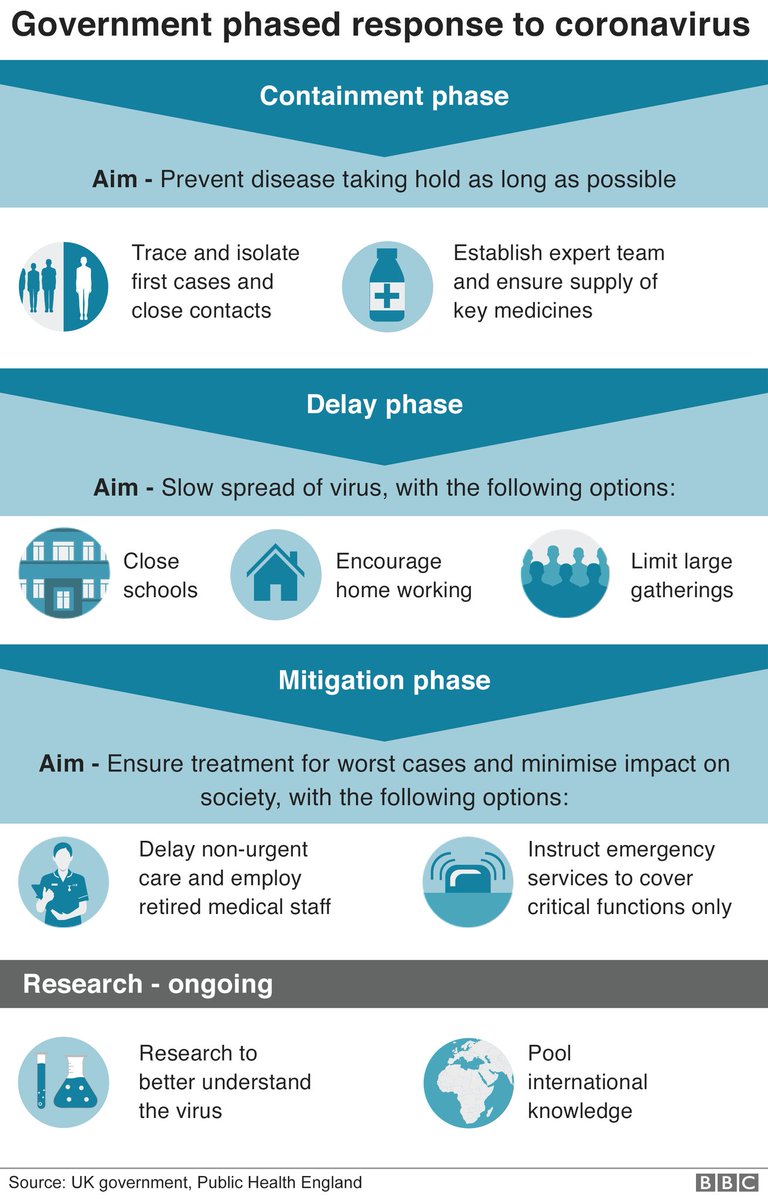
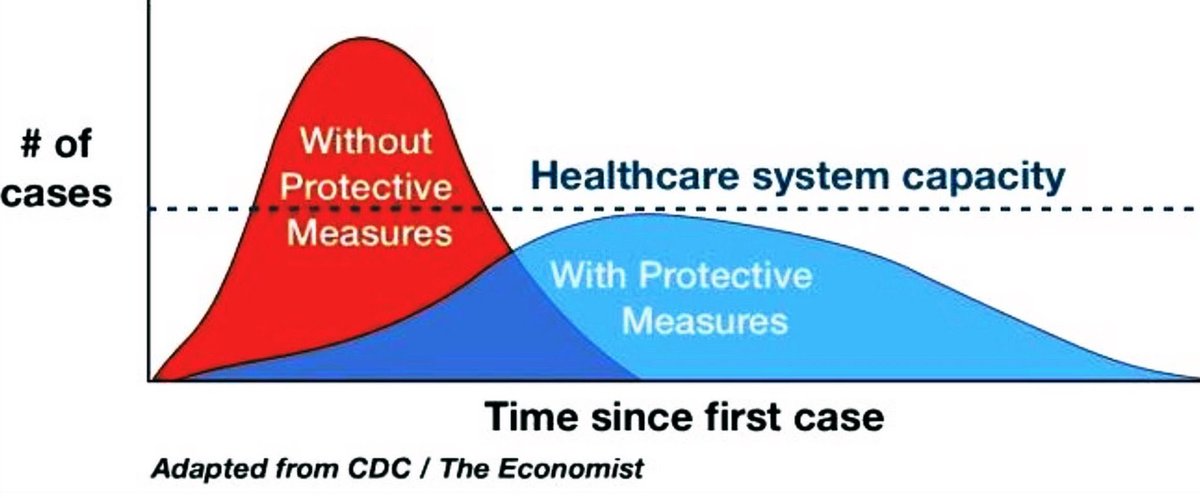
We need to clearly define when the public health goal is containment-trying to keep the virus from circulating- and when the goal shifts to mitigation-working to reduce the peak impact of the outbreak
I'm proud to have worked as a CDC Epidemic Intelligence Service Officer, and I never had smarter, harder working colleagues than during my 12 yrs at @nycHealthy
What I'm going to describe is informed by my past experience and conversations w experts, but I am not an expert in #COVID19
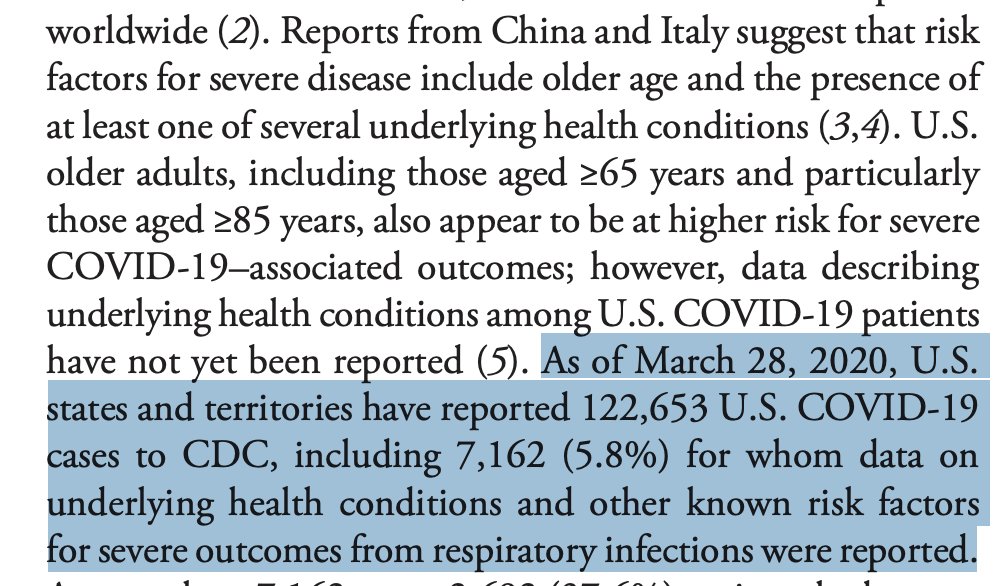
We are treating the outbreak in the US as if we are in containment mode- case identification, contact tracing, quarantine and active monitoring of exposed individuals
But I fear that in many locales there is already sustained community spread
*and we know that these are just the tip of the iceberg* because of the delays in testing
That means that in the next two weeks the number of diagnosed cases will explode
Closing schools
Cancelling events.
Telling people to stay home.
I see no guidance as to which localities are at this stage, and what they should do.
@CDCgov must do better
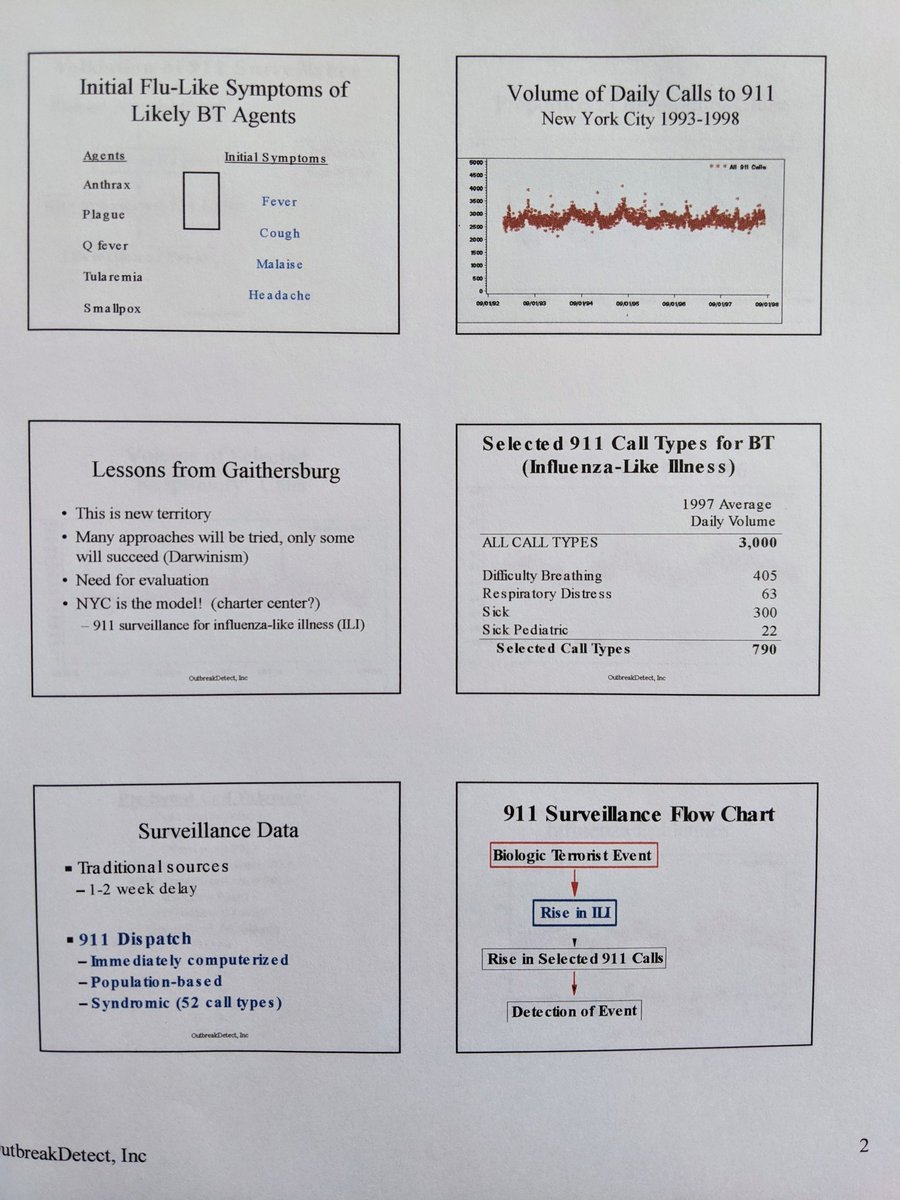
And here's the thing-we invested hundreds of millions of dollars to develop exactly this capability
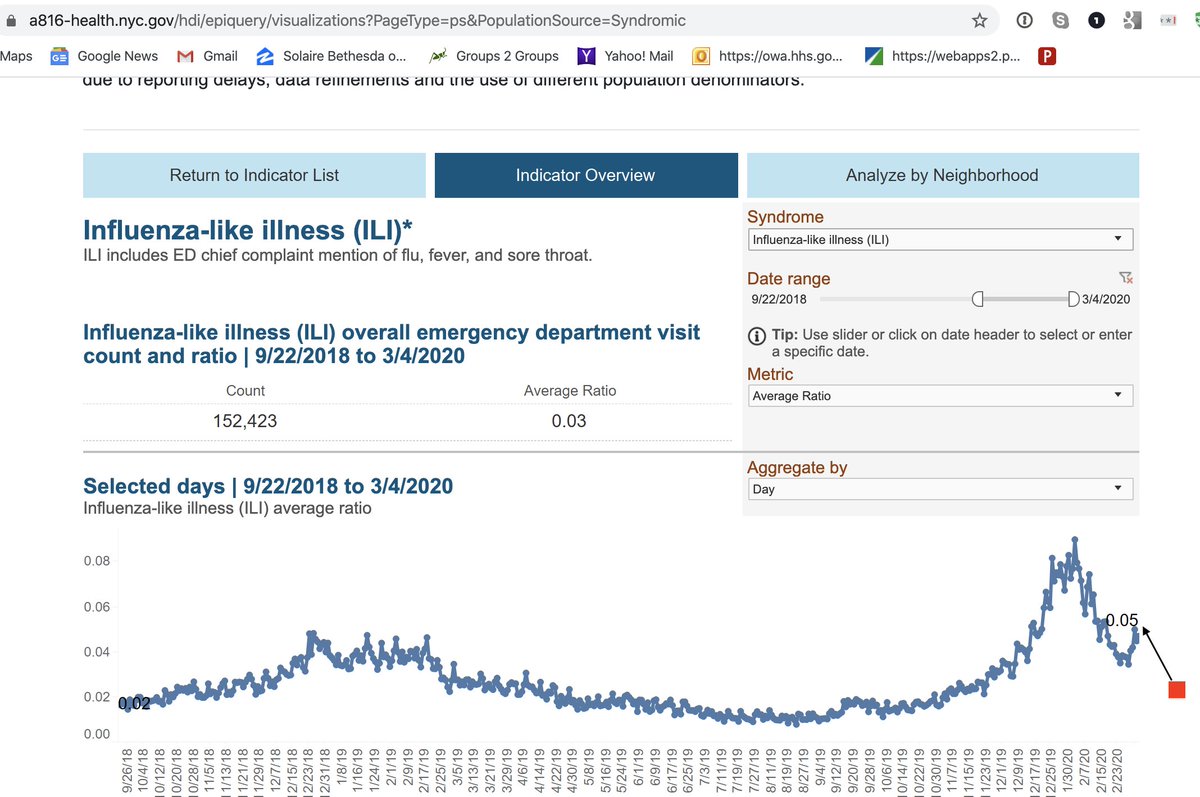
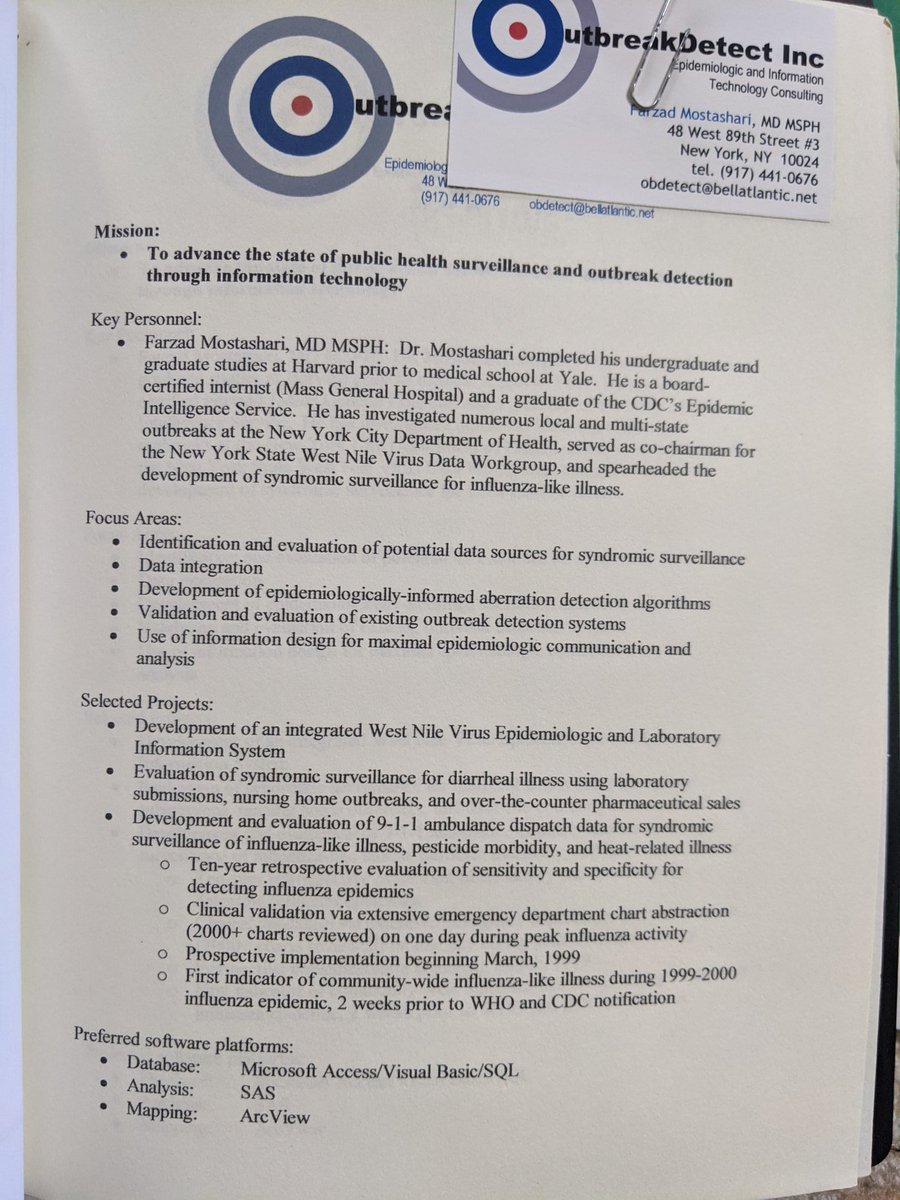
After 9/11, I was part of a group of what would now be called Data Scientists who pioneered "syndromic surveillance"- monitoring things like emergency department registration data for real-time public health surveillance
academic.oup.com/jamia/article/…
I was in one of the leading centers, NYC
wwwnc.cdc.gov/eid/article/10…
Over 70% of hospitals in the US are sending realtime data to public health now
cdc.gov/nssp/index.html
reassuringly, you can see the peak of influenza activity rising each year, and subsiding.
I don't know if federal authorities are tightly monitoring fever/cough ER visit trends across the country and investigating if #COVID19 I hope so
We need to be working URGENTLY on expanding/protecting healthcare capacity
An "abundance of caution" in CDC guidance to impose airborne precautions/N95 masks (as for TB) vs droplet precautions (as in flu)
we don't have enough N95 masks.
cdc.gov/infectioncontr…
What does that do to healthcare capacity?
Pushing testing of asymptomatic contacts or mild cases (no-copay, "if you want a test you can get it") after you already have widespread community transmission
That further exposes other patients and healthcare workers, and saps resources
like this:
1) Severe Acute Respiratory Illness (SARI) surveillance, Active case finding, contact tracing, quarantine.... UNTIL we have evidence of sustained community transmission (multiple community-acquired cases, validated non-flu ED ILI signal)
THEN
Stop routine testing in mild/asymptomatic
Stop contact tracing
Cancel mass gatherings
we urgently need to find out if children are infectious, not just infected, and whether school closures work
not shaking hands
washing hands, using hand sanitizer
practicing not touching your face (good luck)
working from home
We can't do what they did.
Not just in terms of open society, but in sheer resources.
In Wuhan >1,800 TEAMS of epidemiologists, min 5 people/team, were tracing tens thousands of contacts a day
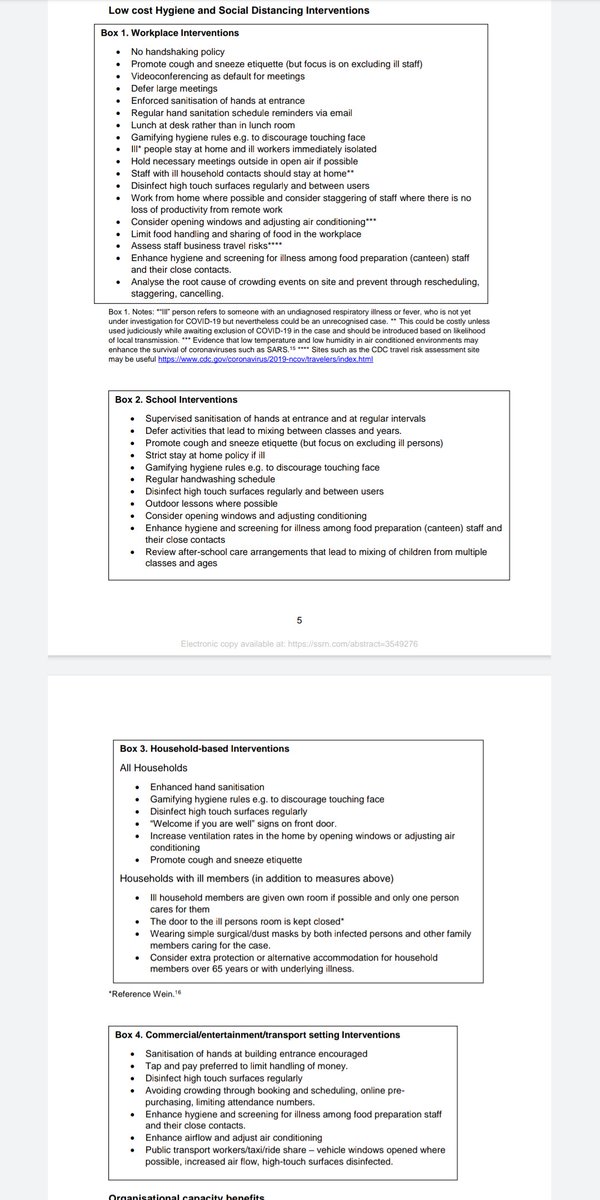
Also, excellent clear writing from @CraigBDalton
papers.ssrn.com/sol3/papers.cf…
Of course with a country as large/heterogenous as US, different locales will step through at own pace, not nationwide.
Here's the UK's
bbc.co.uk/news/amp/uk-51…