#crazy Useless #patient
1/n
Middle-aged man, loves his #family, #farming, drives a cab, #happy. Son & wife at #home. Father-son relationship strong as rock. One #morning, son finds father mumbling to self. Mother says he hardly slept
Mumbling becomes angry ramblings. #Clinical
1/n
Middle-aged man, loves his #family, #farming, drives a cab, #happy. Son & wife at #home. Father-son relationship strong as rock. One #morning, son finds father mumbling to self. Mother says he hardly slept
Mumbling becomes angry ramblings. #Clinical

2/n
Has very little #breakfast. Walks excessively. Goes and lies down, only to get up and walk again. Family interactions little. Sleeps well for 2 hours from 12 to 2PM. Lunchtime. Groggy #father gets on the lunch table and defecates near plates and food. Son and mother aghast.
Has very little #breakfast. Walks excessively. Goes and lies down, only to get up and walk again. Family interactions little. Sleeps well for 2 hours from 12 to 2PM. Lunchtime. Groggy #father gets on the lunch table and defecates near plates and food. Son and mother aghast.
3/n
Father has gone mad. Calls the friendly neighbor, brings his car, rushes to #Medical specialty #clinic nearby. Father disoriented. Son gets the Fword from his own father multiple times, he is shocked! Then comes hurling of abuses after which they restrain him in the car.
Father has gone mad. Calls the friendly neighbor, brings his car, rushes to #Medical specialty #clinic nearby. Father disoriented. Son gets the Fword from his own father multiple times, he is shocked! Then comes hurling of abuses after which they restrain him in the car.
4/n
In the clinic, #young duty-doc LOOKS at the patient, diagnoses #psychosis, advises observation and sedatives. After 2mg lorazepam, patient knocked out, later wakes up confused. Starts gibberish talk again. In between he identifies the wife, not son. This is devastating.
In the clinic, #young duty-doc LOOKS at the patient, diagnoses #psychosis, advises observation and sedatives. After 2mg lorazepam, patient knocked out, later wakes up confused. Starts gibberish talk again. In between he identifies the wife, not son. This is devastating.
5/n
The young #Doctor is called again. He says this needs advanced #treatment. Psychosis is ‘refractory’ - he tells the #nurse – like a bloody crazy useless mad person (son overhears). Saddened by the fact that his father is driven to crazy for what reason?
The young #Doctor is called again. He says this needs advanced #treatment. Psychosis is ‘refractory’ - he tells the #nurse – like a bloody crazy useless mad person (son overhears). Saddened by the fact that his father is driven to crazy for what reason?
6/n
So, they rush him in an ambulance to a bigger General #hospital nearby where an elderly #emergencymedicine doc sees the confused, groggy, occasionally abusive patient in restraints. He LOOKS attentively, but also #touch and #EXAMINE the patient.
So, they rush him in an ambulance to a bigger General #hospital nearby where an elderly #emergencymedicine doc sees the confused, groggy, occasionally abusive patient in restraints. He LOOKS attentively, but also #touch and #EXAMINE the patient.
7/n
Lesson 1: don’t #practice visual medicine. CLINICALLY EXAMINE the patient. The patient and family are gladdened by this. They get a sense that there is #care and #comfort is on the way if a doctor places her/his hands on the patient. Don’t be shy. #MedicalStudents
Lesson 1: don’t #practice visual medicine. CLINICALLY EXAMINE the patient. The patient and family are gladdened by this. They get a sense that there is #care and #comfort is on the way if a doctor places her/his hands on the patient. Don’t be shy. #MedicalStudents

8/n
He finds a firm liver, enlarged spleen and spider angioma signs of cirrhosis. Son says father used alcohol heavily, stopped a year ago after #Blood vomiting after binge&retching. Doc says looks like he has cirrhosis and issues – needs gastro/liver doc. #Medical #examination
He finds a firm liver, enlarged spleen and spider angioma signs of cirrhosis. Son says father used alcohol heavily, stopped a year ago after #Blood vomiting after binge&retching. Doc says looks like he has cirrhosis and issues – needs gastro/liver doc. #Medical #examination
9/n
Our evaluation confirms #cirrhosis and portal hypertension (PHT; increase in liver pressure when liver shrinks). PHT is like a block in the highway. Cars get to take service roads and bypasses. These service roads/bypasses for #Portal venous blood are called #collaterals
Our evaluation confirms #cirrhosis and portal hypertension (PHT; increase in liver pressure when liver shrinks). PHT is like a block in the highway. Cars get to take service roads and bypasses. These service roads/bypasses for #Portal venous blood are called #collaterals
10/n
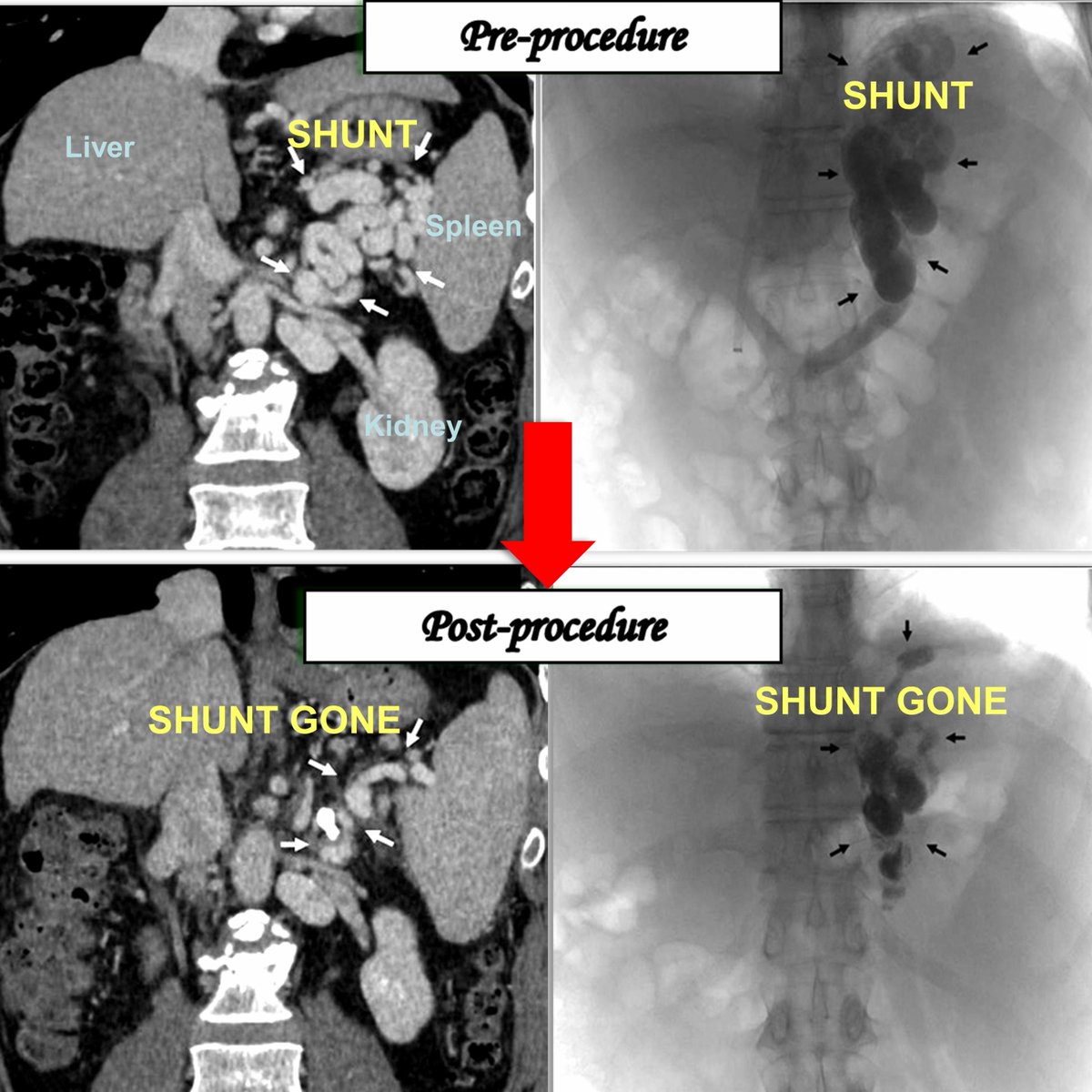
Some collaterals are huge – called shunts, drawing blood away from liver, increasing #ammonia waste, resulting in brain failure – hepatic encephalopathy. In patient, blood ammonia levels were >300 and patient diagnosed with hepatic encephalopathy. #CT #Scans show large shunt
Some collaterals are huge – called shunts, drawing blood away from liver, increasing #ammonia waste, resulting in brain failure – hepatic encephalopathy. In patient, blood ammonia levels were >300 and patient diagnosed with hepatic encephalopathy. #CT #Scans show large shunt
11/n
What was done? Lower ammonia. Look if patient candidate for liver #Transplant (using #MELD score and if not a transplant candidate, then block the shunts. How? Simple non-surgical #interventional #radiology procedure – shunt embolization by @SRajesh_IR
#irad #GITwitter
What was done? Lower ammonia. Look if patient candidate for liver #Transplant (using #MELD score and if not a transplant candidate, then block the shunts. How? Simple non-surgical #interventional #radiology procedure – shunt embolization by @SRajesh_IR
#irad #GITwitter
12/n
See what happens in the image below. Large shunts are taken care of. Ammonia reduction brings patient back to senses. Discharged a week later; CT scan done 3 months later showed shunts are gone. #Sedatives and #hypnotics worsen #encephalopathy in cirrhosis.
See what happens in the image below. Large shunts are taken care of. Ammonia reduction brings patient back to senses. Discharged a week later; CT scan done 3 months later showed shunts are gone. #Sedatives and #hypnotics worsen #encephalopathy in cirrhosis.
13/End
Do not forget to examine. Examine. Examine.
‘A good physician treats the disease but a great physician treats the patient who has the disease’
Not every cirrhosis patient is a goner at diagnosis.
“Diagnosis is not the end, but the beginning of practice”
Do not forget to examine. Examine. Examine.
‘A good physician treats the disease but a great physician treats the patient who has the disease’
Not every cirrhosis patient is a goner at diagnosis.
“Diagnosis is not the end, but the beginning of practice”
• • •
Missing some Tweet in this thread? You can try to
force a refresh