This nationwide complete analysis of all adult deaths in #England & #Wales has found that the #COVID pandemic has resulted in an abrupt inflation in acute #cardiovascular deaths above that expected for the time of year. heart.bmj.com/content/early/…
That is, about 2000 additional deaths over a 4 month period.
Nearly half of the deaths occurred outside of the #hospital setting, either at #home or in #carehomes.
The greatest proportional increase in excess acute #cardiovascular deaths occurred in people’s homes.
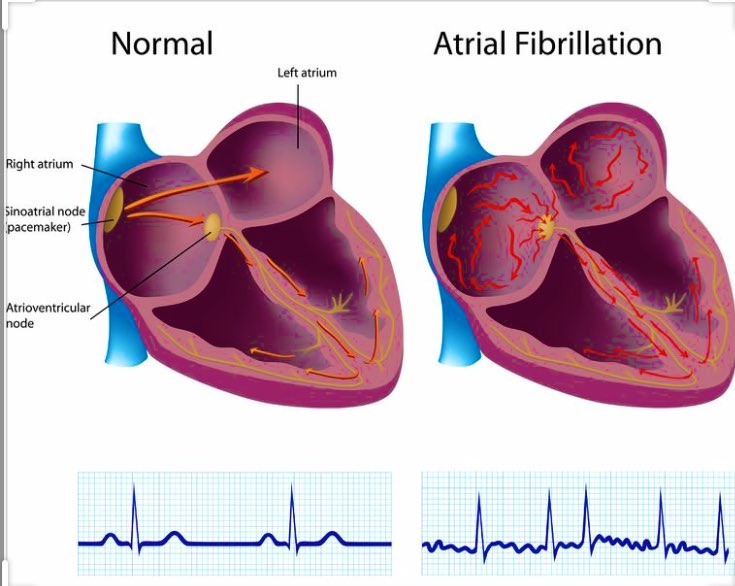
The most frequent cause of acute #cardiovascular death during the #COVID19 pandemic in #England & #Wales was #stroke followed by #heartattack & #heartfailure.
We studied all adult acute #cardiovascular deaths (n=587,225) in England & Wales, between 1st January 2014 & 30th June 2020.
After 2nd March 2020, there were 28,969 acute #cardiovascular deaths of which 5.1% related to #COVID19, & an excess acute cardiovascular mortality of 2085 (+8%).
The greatest cause of excess cardiovascular death in care homes & hospices was #stroke (715, +39%), compared with ACS (#heartattack) (768, +41%) at home & cardiogenic shock (55, +15%) in #hospital.
This ‘displacement of death’, most likely, signifies that the public either did not seek help or were not referred to #hospital during the pandemic – a finding supported by the fact that the majority of acute #cardiovascular deaths were not recorded as due to #COVIDー19.
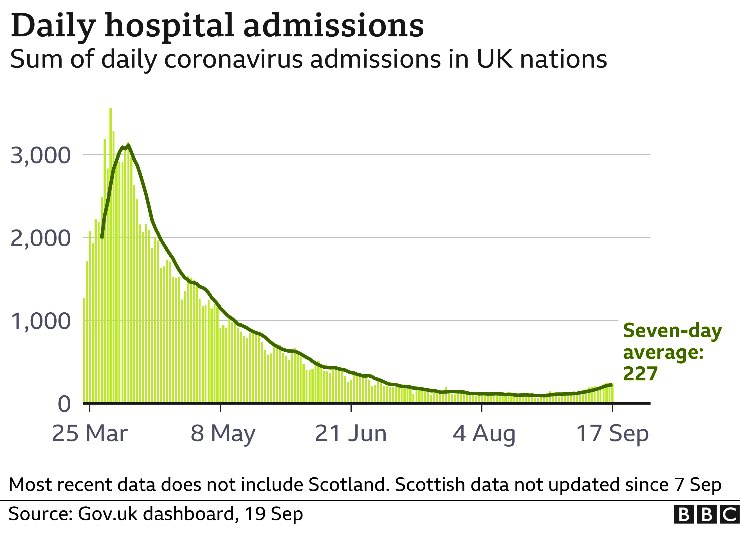
Given the above times series plots show that the excess in acute #cardiovascular mortality began in late March 2020 & peaked in early April 2020, @GOVUK directives at the time including the onset of UK #lockdown on 23/3/20 could have accentuated a maladaptive public response.
That is, the excess #cardiovascular deaths began to emerge at the time the Government was promoting its ‘Stay at home, Protect the #NHS, Save lives’ messages.
Care homes & hospices witnessed a substantial increase in excess acute #cardiovascular deaths. This finding highlights the susceptibility of the elderly and co-morbid to the wider implications of COVID-19 crisis.
That is, not only were #carehome residents prone to the respiratory effects of #COVIDー19 infection, but they will also have been exposed to the acute #cardiovascular complications of COVID-19 & decisions not to go to #hospital for fear of becoming infected.
This situation will have been exacerbated by the discharge of unknowingly infected patients from #hospitals to #carehomes, a lack of systematic testing, the efficient person-to-person transmission of the virus, & its propensity to death in the vulnerable.
Through the systematic classification of all adult deaths in England & Wales, it is possible to show there has been an excess in acute #cardiovascular mortality during #CovidUK , seen greatest in the community & corresponds to public messaging & decline in admissions to hospital.
... & some people may have taken the messaging to mean that the #NHS was not able to cope if they had a medical emergency, or that #hospitals were a place where they would catch the contagion
“It is entirely plausible that a number of deaths could have been prevented if people had attended #hospital quickly when they began to experience their #heartattack or #stroke.”
“... people who died at home were most likely to have had a #heartattack. This is further support for the speculation that many people were staying away from #hospital even though they were very ill with an acute #cardiovascular illness.”
“The sad irony is that previous research we have undertaken showed that nationwide #heartattack services remained fully operational & continued to deliver high quality care during the peak of the [#COVID19] pandemic.”
As the #NHS prepares for another wave of #COVID19, we need to ensure people understand that #hospitals are open & have processes in place to minimise the risks of patients becoming infected.” @NHSEngland @BritishCardioSo @BSHeartFailure @BCIS_uk @BcsPresident @TheBHF @PHE_uk
The investigation was carried out by a team of #data scientists & clinicians, led by academics @UniversityLeeds @LeedsHospitals @LeedsMedHealth @UoL_LICAMM @LIDA_UK . The other collaborators were from @mmamas1973 @DrShingKwok @tomdenwood @NHSDigital @ONS @CardiacAudit
The article is freely available here @Heart_BMJ: Place and causes of acute cardiovascular mortality during the COVID-19 pandemic heart.bmj.com/content/early/…
• • •
Missing some Tweet in this thread? You can try to
force a refresh