
1/ During July 2020 many worked quickly to scramble #COVID19 prep before the Fall classes. I helped model estimated COVID #aerosol risk as @UofDenver made plans. Not allowed then, but shared now in case it can prompt discussion for Winter prep.
Doc + 🧵:
bit.ly/3gVfMcu
Doc + 🧵:
bit.ly/3gVfMcu
2/ A key concern at the time (& still) was #music ensemble classroom activities, b/c it was obvious early on that #COVIDisAirborne and that #choir & wind instruments were likely to present high COVID #aerosol risk.
nfhs.org/articles/unpre…
nfhs.org/articles/unpre…
3/ Using my version of an aerosol #boxmodel, I calculated probability that #SARSCoV2 could infect after breathed out by someone in specific classrooms. With this I could easily investigate best prevention bang for buck. I.e. Rehearsal duration? Wait time b/n classes? Etc.
4/ For each of several classrooms & activities, I investigated #aerosol risk w/ a range of values for:
1. Number of students
2. Wait time after class
3. Duration of class
4. Air exchange rate
5. Added filtration units
6. Community prob. of infection
7. Relative infectivity rate



1. Number of students
2. Wait time after class
3. Duration of class
4. Air exchange rate
5. Added filtration units
6. Community prob. of infection
7. Relative infectivity rate




5/ In all cases, the COVID risk model was operated with the assumption that all individuals in choir or wind ensemble rehearsal would be distanced by 12 ft and be wearing masks at all times.
6/ DURATION: One important result came by estimating quantitative risk reduction by reducing rehearsal time. E.g. by reducing from 45 ⮕ 30 min, #aerosol risk went down 50-60%, depending on room specifics. 

7/ WAIT TIME: Second result was that waiting longer after class could reduce risk, but with diminishing returns w/ more time. If higher ventilation rate, the faster risk was flat w/ extra wait (b/c all aerosol from prev class already removed & only risk left from those present). 


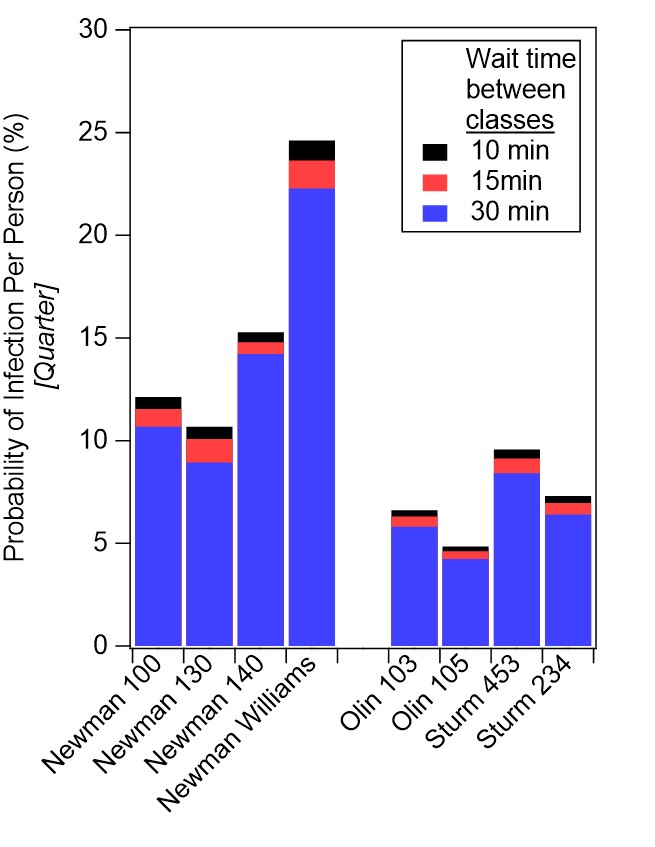


8/ FILTRATION: Third result was to show that adding portable HEPA filtration could reduce risk, but not significantly in large or already well-ventilated rooms. 

9/ FILTRATION IN PRACTICE ROOMS: An important exception to the previous statement about HEPA filtration was ⮕ using a DIY #boxfanfilter after a small practice room was occupied could reduce risk dramatically (to ~zero) after 15 min of wait.
texairfilters.com/how-a-merv-13-…
texairfilters.com/how-a-merv-13-…

10/ #CO2 MONITORING (using a few ~$150 sensors) was helpful to verify air exchange sufficient in these rooms. In one case, was clear #ventilation schedule was not well-matched with student rehearsal timing. Discussed w/ Facilities to change schedule, fixed issue & lowered risk! 

11/ Although we did our own COVID #aerosol modeling and monitoring specific to music & lecture classrooms at @UofDenver, the observations & recommendations made were also informed significantly by work led by @ShellyMBoulder and summarized here:
nfhs.org/articles/third…
nfhs.org/articles/third…
12/ See these links related to research by @ShellyMBoulder & @SmogDr groups related to #music & fine arts related #aerosol emissions:
nfhs.org/media/4119362/…
nfhs.org/articles/unpre…
smtd.colostate.edu/reducing-bioae…
nfhs.org/media/4119362/…
nfhs.org/articles/unpre…
smtd.colostate.edu/reducing-bioae…

13/ The model I used for calculations was based on the #WellsRiley box model, assuming quick mixing of #SARSCoV2 aerosols into the room. @jljcolorado released a public calculator months ago that is still extremely useful:
tinyurl.com/covid-estimator
tinyurl.com/covid-estimator
14/ I took that model and re-wrote into @WaveMetrics #IgorPro to optimize calculations for my purpose, and to add features like the ability to analyze the effect of aerosol build-up before a class period & risk reduction based on wait time. 

15/ There are now many really useful, interactive #COVID #risk calculation tools available on the internet for various purposes.
Examples:
safeairspaces.com
…re-modeler-data-devils.cloud.duke.edu
zeit.de/wissen/gesundh…
For more search “model” on tab 1 here: bit.ly/3fzmB16
Examples:
safeairspaces.com
…re-modeler-data-devils.cloud.duke.edu
zeit.de/wissen/gesundh…
For more search “model” on tab 1 here: bit.ly/3fzmB16
16/ To estimate the amount and type of portable air cleaner that could be best for your use, see this great interactive calculator put together by @j_g_allen @cedenolaurent @ShellyMBoulder. #HEPA #filtration
docs.google.com/spreadsheets/d…
docs.google.com/spreadsheets/d…
17/ I previously put together related COVID aerosol modeling observations about holiday meal risk into a recent thread & document (Hint: don't share indoor meals w/ mixed households right now!:
https://twitter.com/HuffmanLabDU/status/1328732644629049345
18/ And also shared a variety of other #CO2 measurements from my life activities & some tips on measuring the #ventilation rate in your home or school as a #DIY project:
https://twitter.com/HuffmanLabDU/status/1335999080938364932
19/ Remember that #layered COVID prevention efforts are still key, because we are not out of the woods on this pandemic. Details above discuss observations from #aerosol modeling in university classrooms, but the general principles apply everywhere.


20/ The #vaccine is now being distributed, but still months before we are all safe. #BeAirAware & follow guidelines (#masks, #ventilation, social distance, reduce shared indoor time), use risk tools if helpful, be wise, and encourage safe #COVID practices!
bit.ly/3gVfMcu
bit.ly/3gVfMcu
• • •
Missing some Tweet in this thread? You can try to
force a refresh



