Multisystem inflammatory syndrome in children is driven by zonulin-dependent loss of gut mucosal barrier.. @vipintukur @ProfSomashekhar @naveenthacker @iapindia @INDIANJOURNALO4 @VirusesImmunity @EditorIndPed @ICMRDELHI @MoHFW_INDIA @iiscbangalore 

Weeks after #SARS-CoV-2 inf or exposure, some children develop a severe, life-threatening illness called Multisystem Inflammatory Syndrome in Children (#MIS-C). GI symptoms are common in MIS-C pts & severe hyperinflammatory response ensues with potential for ❤️ complications.
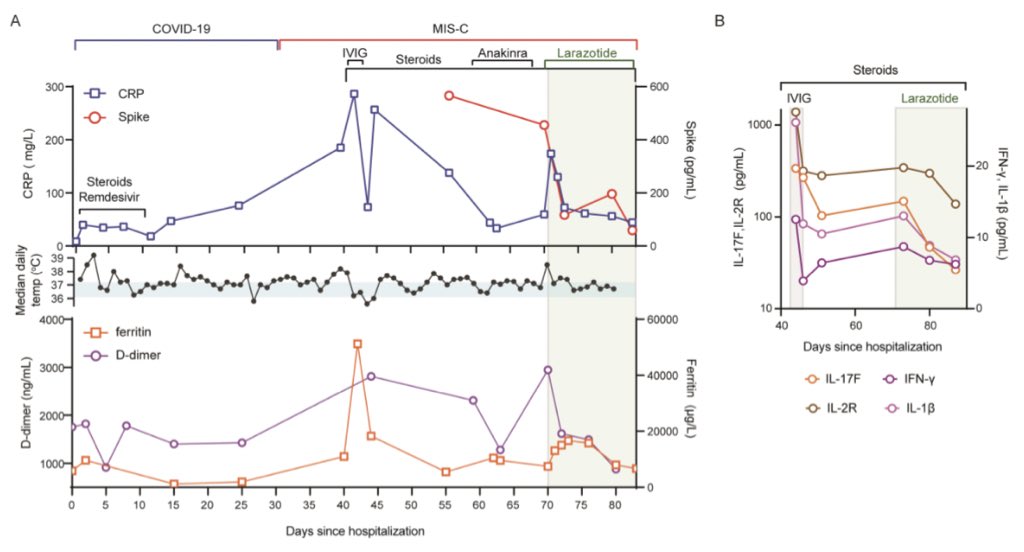
👉🏽As proof of concept, they treated a #MIS-C patient with #larazotide, a #zonulin antagonist, & monitored impact on antigenemia and clinical response.
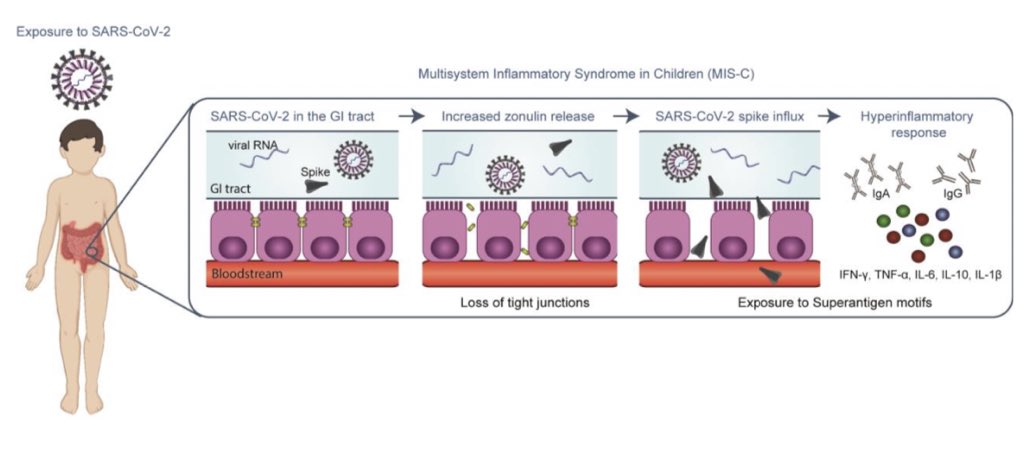
👉🏽in MIS-C, prolonged + of SARS-CoV-2 in t GI tract ➡️ to release of zonulin, a biomarker of intestinal permeability,
👉🏽in MIS-C, prolonged + of SARS-CoV-2 in t GI tract ➡️ to release of zonulin, a biomarker of intestinal permeability,
wth subsq trafficking of SARS-CoV-2 antigens into t 🩸 , ➡️to hyperinfl. T MIS-C pt treated wth larazotide displayed a coinciding ⬇️ in plasma SARS-CoV-2 Spike Ag levels, inflammatory markers, & a resultant clinical improvement above tht achieved wt currently avail treatments.
These mechanistic data of MIS-C pathogenesis provide insight into targets for diagnosing, treating, and preventing MIS-C, which are urgently needed for this increasingly common severe COVID-19-related disease in children. @EricTopol #tweetorial #MedTwitter #COVID19Pandemic
T source of t antigenemia in MIS-C is likely t gut. MIS-C develops days to weeks after resolution of t initial infection, often when SARS-CoV-2 viral levels are low/undetectable in respiratory secretions, making t MIS-C trigger less likely 2 be frm upper respiratory tract source
⬆️zonulin indicate breakdown of intestinal epithelial tight junctions,➡️ may let t leak of 🦠 Ag into t 🩸 stream. In Kawasaki disease, pts presenting wth prominent GI symptoms at t onset of illness R less likely to respond to IVIG therapy alone & thus ➡️ to develop ❤️ aneurysm
As zonulin-dependent loss of gut integrity develops in MIS-C but not COVID-19-infected children, this suggests that a chronicity of SARS-CoV-2 dysbiosis in the gut results in a cumulative increase in breakdown of mucosal barrier integrity. #ACADEMIA #scicomm
Age and sex were described for all pediatric patients and controls, in addition to clinical features of illness for acute #COVID-19 and #MIS-C. 

Timing of sample collection and sample analysis are defined for children with MIS-C or acute COVID-19. @PedCritCareMed #Pediatrics #rheumatology 

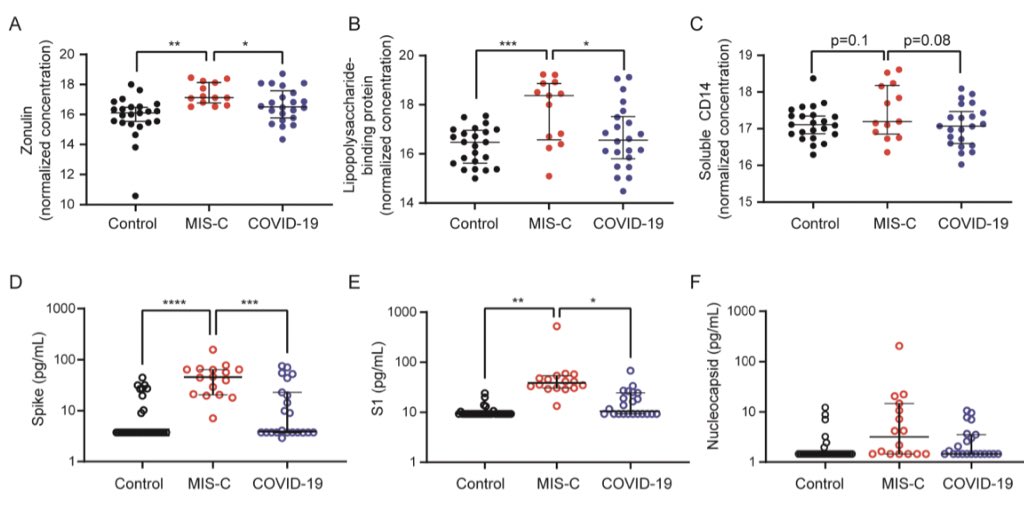
A)Plasma zonulin,B) LPS-binding proteinC) soluble CD14 ,in children with MIS-C (n=13),COVID19 (n=21),& non-COVID19 controls (n=23).D)SARS Spike,E)S1 & F) Nucleocapsid were quantified from t plasma of 👶 with MIS-C (n=16),👶 with acute COVID-19 (n=22),& pre-pandemic contr (n=32) 
proposed hypo ➡️ MIS-C. 🦠 enters t GI tract. Dysbiosis leads to ⬆️ zonulin release & resultant loss of tight junctions. 🦠Ag, especially t Spike protein, breaches t mucosal barrier, entering t 🩸 stream. T superAg motif of t Spike protein +s a pathogenic hyperinflam response. 
jci.org/articles/view/… .... to summarise 



• • •
Missing some Tweet in this thread? You can try to
force a refresh