Biggest paper yet from the lab now a #preprint on @biorxivpreprint. A massive #openscience resource on #tissueTregs, and what makes #Tregs tick in the #tissues.
Spoiler-alert: Tissue Tregs are really different from what we all thought. 🧵 1/21
biorxiv.org/content/10.110…
Spoiler-alert: Tissue Tregs are really different from what we all thought. 🧵 1/21
biorxiv.org/content/10.110…
Go back to that sweet innocent time in the spring of 2016. #Brexit was an unlikely joke, @HillaryClinton was cruising to a landslide against some reality TV starlet, and we thought that #TissueTregs formed by seeding tissues and differentiating into unique terminal cells. 2/21 

We had examples of #fatTregs and #muscleTregs becoming unique permanent residents, and the @ERC_Research funded us to undertake an overly ambitious project to look at everything, everywhere, all at once.
Only possible because of the #dreamteam of @jldvib and @olivertburton. 3/21


Only possible because of the #dreamteam of @jldvib and @olivertburton. 3/21


A lot of expertise goes into extracting #Tregs from #tissues, and comparing 48 different tissues from the same mice turns every experiment into a monster task. Many of the improvements we made to our flow cytometry pipeline were made for this paper. 4/21
…rentprotocols.onlinelibrary.wiley.com/doi/10.1002/cp…
…rentprotocols.onlinelibrary.wiley.com/doi/10.1002/cp…
We characterised the #TissueTreg everywhere, *everywhere*, across the mouse. They are a pretty consistent component of the resident T cells in most non-lymphoid tissues, only unusually high in #skin and #tongue. Still, put together #TissueTregs are only 0.3% of Tregs. 5/21 

At first glance, #tissueTregs looked special. Take a tissue and compare it against lymphoid/blood #Tregs and the differences are huge. But the more tissues you add, the more they look the same. The only three distinct phenotypes were gut, lymphoid and bulk non-lymphoid. 6/21 

(as an aside, you know that old trick of adding intravenous anti-CD45 to exclude vascular contamination? Well, if you do that and perfuse, the vascular "contaminants" actually look quite different from blood, and look closer to the #TissueTreg inside. 7/21) 

"That's just because of the 45+ markers you selected for flow!", you cry. Fair, fair, but the same is true for RNAseq. Take different #TissueTreg populations, say #KidneyTregs and #PancreasTregs and they are 97% identical at the transcriptional level. 8/21 

If you are interested in looking for your favourite gene in #TissueTregs, you can use our handy interactive online expression viewer, made by @SamarTareen. Just pick #Treg or #Tconv and your choice of organs, and out comes nice statistical analysis. 9/21
bioinformatics.babraham.ac.uk/shiny/expressi…
bioinformatics.babraham.ac.uk/shiny/expressi…
You are probably not asking "what about if you #age the mice, or change their #microbiome?", but if you were the answer is... meh? Numbers increase and the phenotype intensifies somewhat, but still, #TissueTregs look generic once you broaden your view. 10/21 

"Ahah!", you cry, "What about the #genetics? Gene X uniquely controls #Tregs from my favourite #tissue!".
Would that it were so, but take ten signature #TissueTreg #genes, knock them out and look across 14 organs, and they either effect all non-lymphoid tissues or none. 11/21
Would that it were so, but take ten signature #TissueTreg #genes, knock them out and look across 14 organs, and they either effect all non-lymphoid tissues or none. 11/21

"Surely, at least, you can confirm they are permanent residents", I can feel you start to worry. "After all, parabiosis experiments proved that".
Did they, though? Most experiments were done at 2 weeks. What happens when you look a little longer? 12/21
Did they, though? Most experiments were done at 2 weeks. What happens when you look a little longer? 12/21

We had @Vaclav_G run #Markovchain modelling on a massive parabiosis time-course, and #TissueTregs only had a half-life of ~3 weeks, edging up towards 10 weeks in the fat and gut. Not permanent residents. 13/21 

At this point we had to drop the "seed & specialise" model. It just no longer fit the data.
"#TissueTregs are pan-tissue in nature", came the Siren's call.
They look the same, use the same genes, only drop-in to visit an organ - perhaps they recirculate across tissues? 14/21
"#TissueTregs are pan-tissue in nature", came the Siren's call.
They look the same, use the same genes, only drop-in to visit an organ - perhaps they recirculate across tissues? 14/21

"We can test that", I confidently asserted. 4 years ago.
Fortunately, wunderkind @OrianBricard joined and thought of #TCR sequences as #genomic barcodes. Straight off the bat, we knew we were on to something. Liver, kidney, pancreas Tregs all shared the same TCRs. 15/21
Fortunately, wunderkind @OrianBricard joined and thought of #TCR sequences as #genomic barcodes. Straight off the bat, we knew we were on to something. Liver, kidney, pancreas Tregs all shared the same TCRs. 15/21

Strap yourselves in, here it starts to get funky. We took Brian Brown's Pro-Codes and used them to simultaneously track 20+ retrogenic #TissueTreg TCRs. They all drove #Treg fate, and almost all become multi-tissue homing. 16/21 

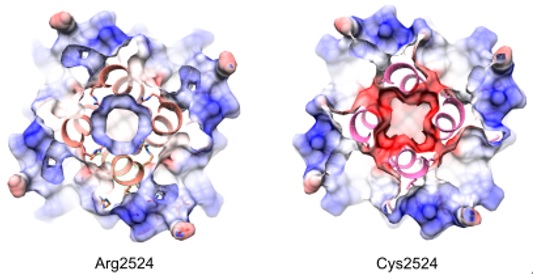
(another aside, if you think that self-reactive #TissueTregs would see different antigens in different tissues... not really. 98% of MHC-presented antigens in each tissue are also presented in other tissues. #Tregs don't know to focus on the tissue-restricted antigens. 17/21) 

For the sake of brevity (yes! I am skipping a lot of data), let's just go to the final proof. Extract #Tregs from the #tissues, reinfuse them, and where do they go? *Shrug*. They don't care. Any tissue will do. Apart from gut Tregs they are tissue-agnostic. 18/21 

Pretty conclusive then. A common pool of #TissueTregs can percolate between multiple non-lymphoid non-gut organs, dipping in for ~3 weeks, turning on a common tissue program, then moving on. Global homeostatic police. Regulatory cells with a pan-tissue beat. 19/21 

Does this mean everyone was wrong about #TissueTregs? Hell no. The field was created by pioneers, with rock-solid data. You just reach different conclusions when you look broader and longer. Makes it even cooler that the same visiting cells rewire each tissue differently. 20/21
Interested? Read the pre-print now, or the expanded version ETA 2025 ;)
Thanks to the team in @VIBLifeSciences, @KU_Leuven, @BabrahamInst and now @CamPathology @Cambridge_Uni. And to @ERC_Research and then @wellcometrust for supporting big visions. 21/21
biorxiv.org/content/10.110…
Thanks to the team in @VIBLifeSciences, @KU_Leuven, @BabrahamInst and now @CamPathology @Cambridge_Uni. And to @ERC_Research and then @wellcometrust for supporting big visions. 21/21
biorxiv.org/content/10.110…
• • •
Missing some Tweet in this thread? You can try to
force a refresh