drive.google.com/file/d/0Byheg1…
First, how will I know when I am at a therapeutic dose? You answer that an optimal methadone dose will not over-sedate you, and will achieve the following goals:
6/
For our patient, the 30 mg dose treated their acute w/d symptoms. Are they at an optimal dose? 7/
/12
Generally, these fall into two categories.
1️⃣ Sedation
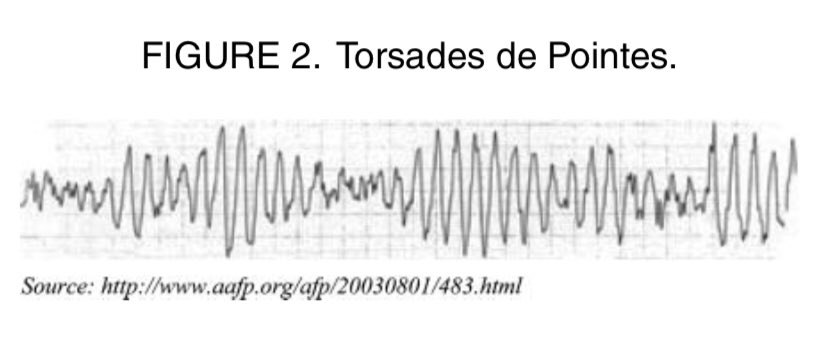
2️⃣ Cardiac risk
A big component of both is potential drug-drug interactions. /14
drive.google.com/file/d/1gP9tb1…