Quick someone tweet a concerning angiogram cine and ask if anyone else would refer a specific stable CAD patient to OMT!!

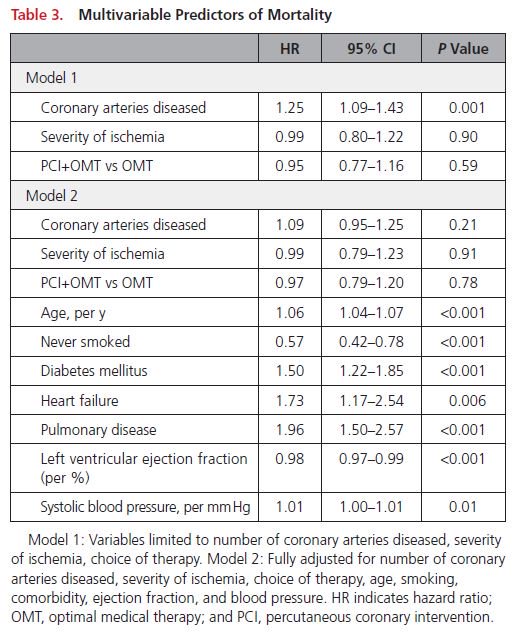
observed that the severity of CAD as assessed by QCA predicted long-term mortality whereas the extent and severity of ischemia as assessed by SPECT MPI did not."