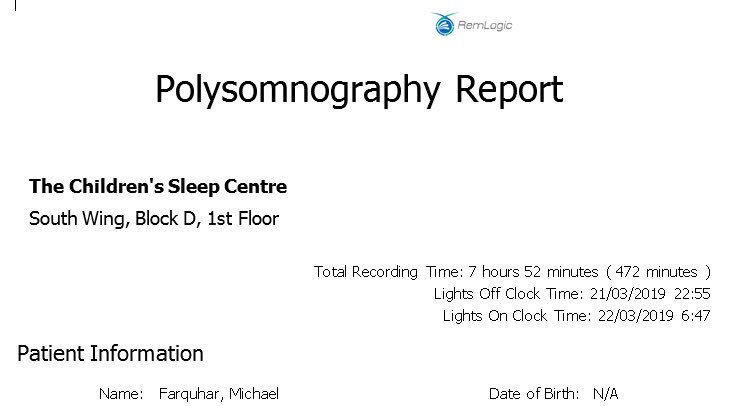
Phase 1 of Snow Leopard, opened in 2016, is our Transitional Care Unit, supporting patients who need Long Term Ventilation as they head from our acute wards to home

We’ve also got increased soundproofing (Big Ben *will* bong again soon...)

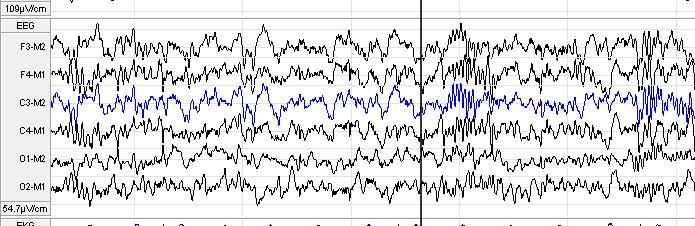
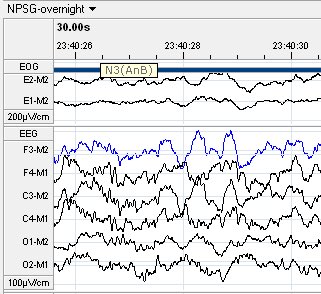
And while many of our patients don’t sleep exactly as they would at home, we almost always get enough sleep to get the good quality data we need a
(I’m still picking it out of my hair 3 hours after my study stopped!)

Although I woke several times overnight, they were generally brief - I only remember 2 of them!
We all wake and settle back as we sleep
33 minutes of “wake after sleep onset” sounds a lot but is fairly normal.
Anything above 85% is fine, and my sleep efficiency of 91% is perfectly respectable.
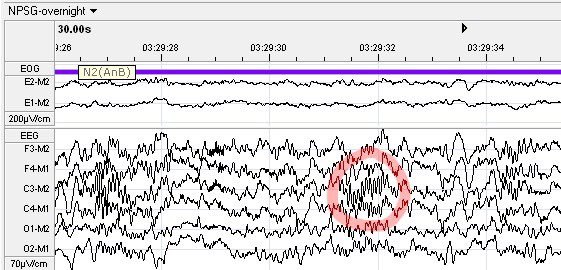
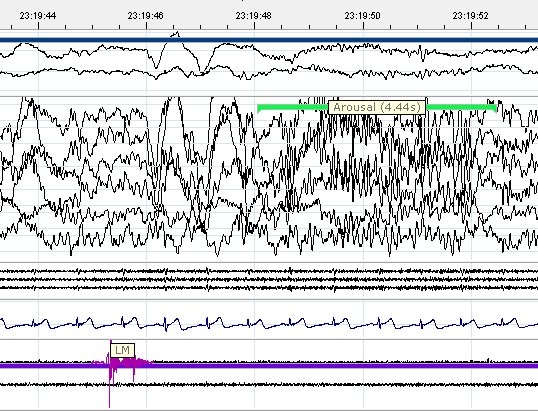
Occasionally we have normal pauses in our breathing, and these *don’t* affect sleep quality usually ... but ...
That muscle paralysis also makes our breathing more vulnerable. Most apnoeas happen during REM, and our brain responds by jumping us out of REM to switch off the paralysis. Clever!
We often don’t *need* that level of sensitivity, but it can be helpful in some situations where we are assessing breathing in sleep
For other reasons, they are MUCH safer sleeping on their backs; the “Back To Sleep” campaign significantly cut the number of Sudden Infant Death Syndrome deaths
Before Big Ben went silent for a few years, we could regularly see impact of his chimes and *BONG!*s on the quality of sleep of children being studied in our lab
(You can read about it @bmj_latest here)

These can be normal (I had a few) but if they affect sleep quality they cause Periodic Limb Movement Disorder
Can be difficult to realise you’ve got it; usually needs bed partner to complain!
The foundation of treating any sleep problem though is good attention to core sleep routine and habits