(A #MedTwitter and #Tweetorials contribution). Appreciate edits by @ebtapper.
Looking again at our para studies (WBC 2480, PMN 74%, total protein 4.3, SAAG >1.1), what is the diagnosis?
Culture-Negative Neutrocytic Ascites = CNNA
By the way, which of the following systems fail in cirrhosis, increasing susceptibility to SBP?
Macrophage = MØ
gastrojournal.org/article/S0016-…
- Serum complement levels become deficient
- Ascites is 5 to 10-fold more dilute than serum = reduced complement/opsonization
- PMN/Kupffer cell functional impairment
gastrojournal.org/article/0016-5…
- Cirrhosis with GI bleeding
- Recurrent SBP
Standard abx for ppx include the following:
- ciprofloxacin 500mg qdaily
- norfloxacin 400mg qdaily
- Bactrim DS qdaily
Note ➡️ important to consider tendon rupture risk w/ FQ's in this young adult.
HRS = hepatorenal syndrome
nejm.org/doi/pdf/10.105…
- Cr>1.0, BUN>30, or T bili>4.0
- Recurrent SBP given increased risk for renal failure
The short answer is culture positivity varies widely, but yield increases when immediate bedside inoculation occurs.
ncbi.nlm.nih.gov/pmc/articles/P…
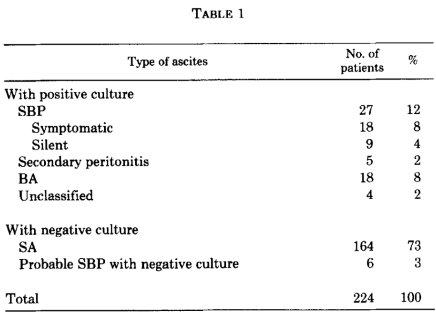
1/ SBP diagnosis: ascitic WBC >500, PMN >250
2/ Consider repeat dx para on day 3 if sx’s persist (fever, abd pain)
3/ Rule out secondary BP w/ Protein >1, Glucose <50, LDH > serum LDH ULN
4/ Ascitic fluid cx yield improves w/ bedside inoculation
clinicalproblemsolving.com/wp-content/upl…
clinicalproblemsolving.com/wp-content/upl…
Thanks for reading! #FOAMed #MedEd