How can we make use of the MCH and MCHC provided with most complete blood counts?
In my 13 years as a doctor, I can’t recall having ever utilized an MCH or MCHC. After reviewing some literature, that might change for me.
Maybe this thread might change your approach too...
Let’s get a baseline. Do you typically look at and utilize the mean corpuscular hemoglobin (MCH) and/or mean corpuscular hemoglobin concentration (MCHC)?
Let's start with the MCH. As the name suggests, this is the average amount of hemoglobin in a red blood cell (RBC). It does not take into account RBC size.
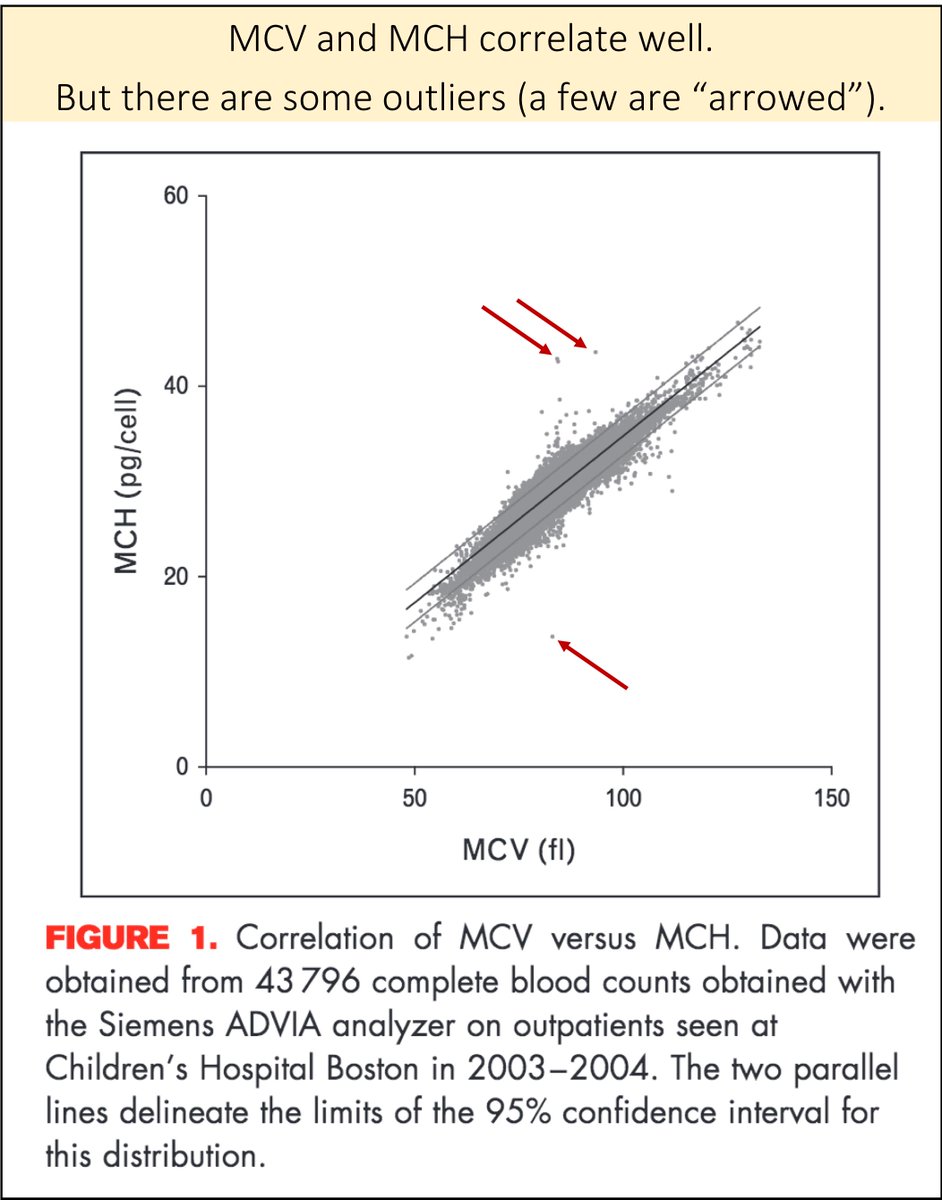
MCH correlates well with mean corpuscular volume (MCV) so many simply use the latter.
ncbi.nlm.nih.gov/pubmed/23449069
If you didn't otherwise know, what would you predict is a more accurate sign of iron deficiency: size of RBC (low MCV) or how much hemoglobin (Hgb) is in the RBC (low MCH)?
[I would have predicted that the amount of Hgb is superior.]
Turns out that a low MCH is the more sensitive value. Multiple studies have shown this.
One example: a 1990 study found the following sensitivities for ferritin <20 ng/mL:
MCV <77 fL = 61%
MCH <27 pg = 74%
ncbi.nlm.nih.gov/pubmed/2272155
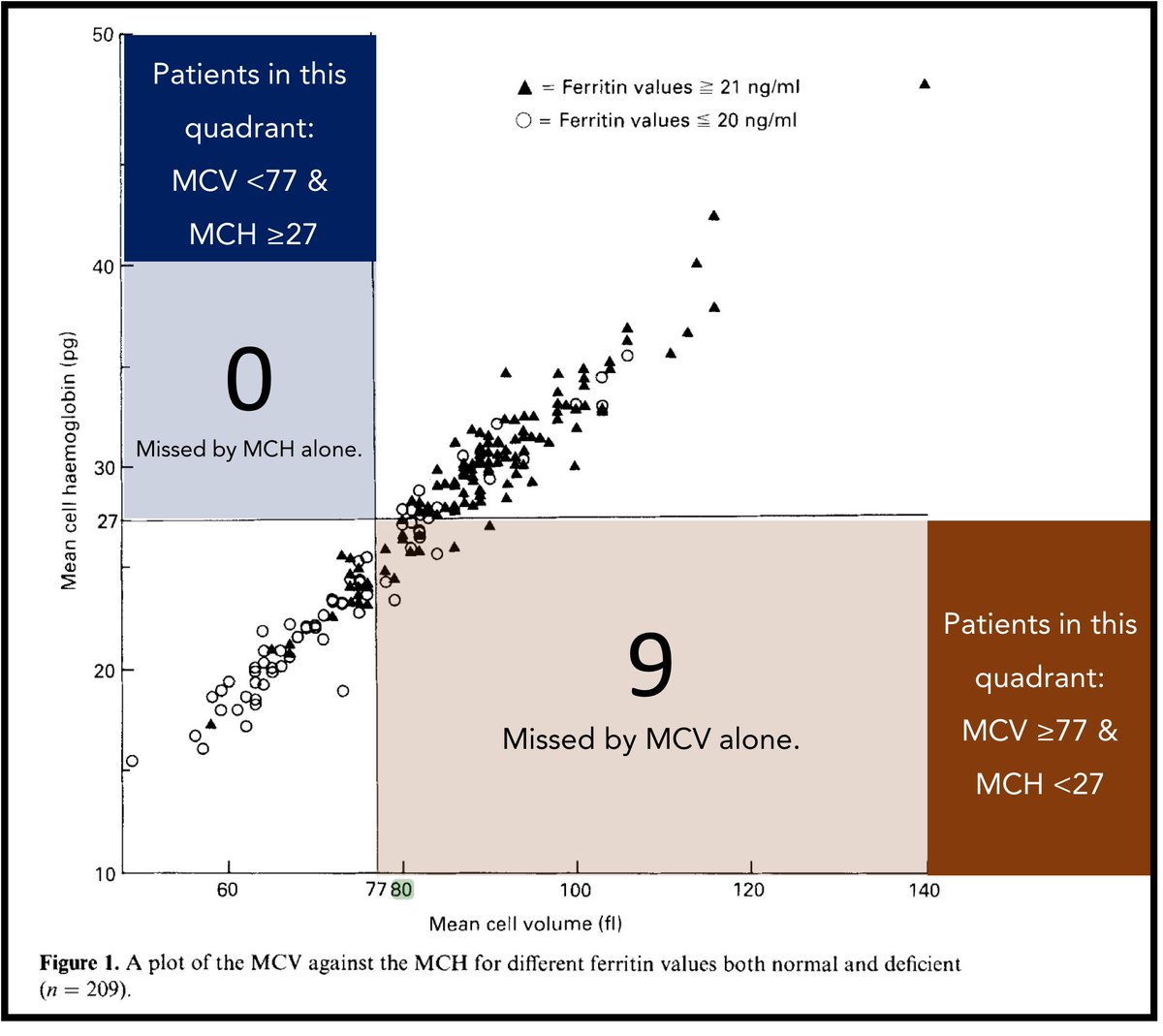
When I look at these sensitivities (which are consistent with other studies), I realize I should not apply an MCV-based schema rigidly.
My take-away: neither MCV nor MCH is sensitive, but if I had to choose one value as a "clue" suggesting iron deficiency, it would be MCH.
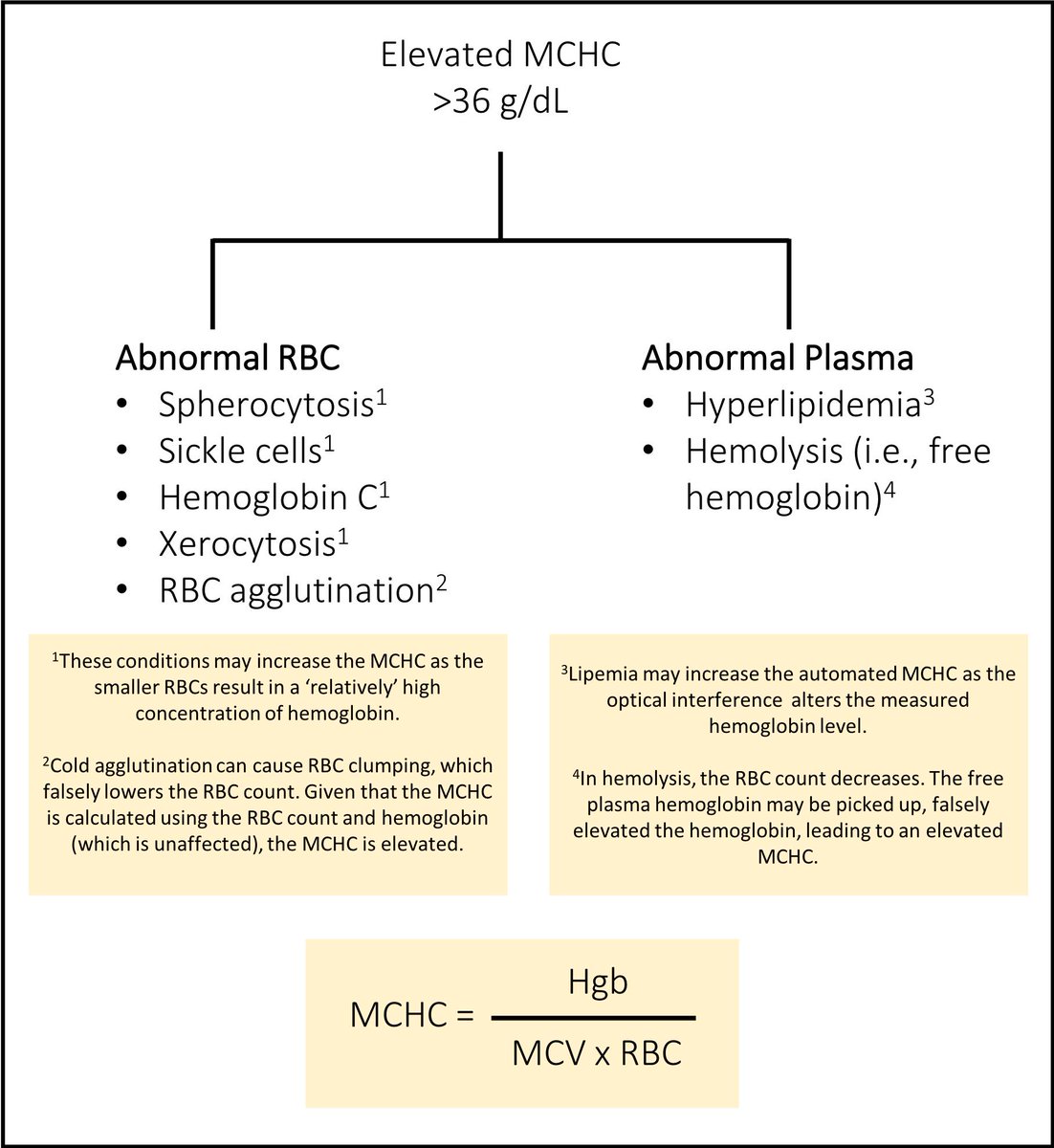
MCHC is fascinating. It indicates the relative amount of Hgb in an RBC.
So, two differently sized RBCs (i.e., MCV is different) with the same amount of hemoglobin in them (i.e., MCH is the same), will also have different MCHC values.
MCHC has value when forming a differential diagnosis and may even provide prognostic value.
Which of the following can be associated with an elevated MCHC?
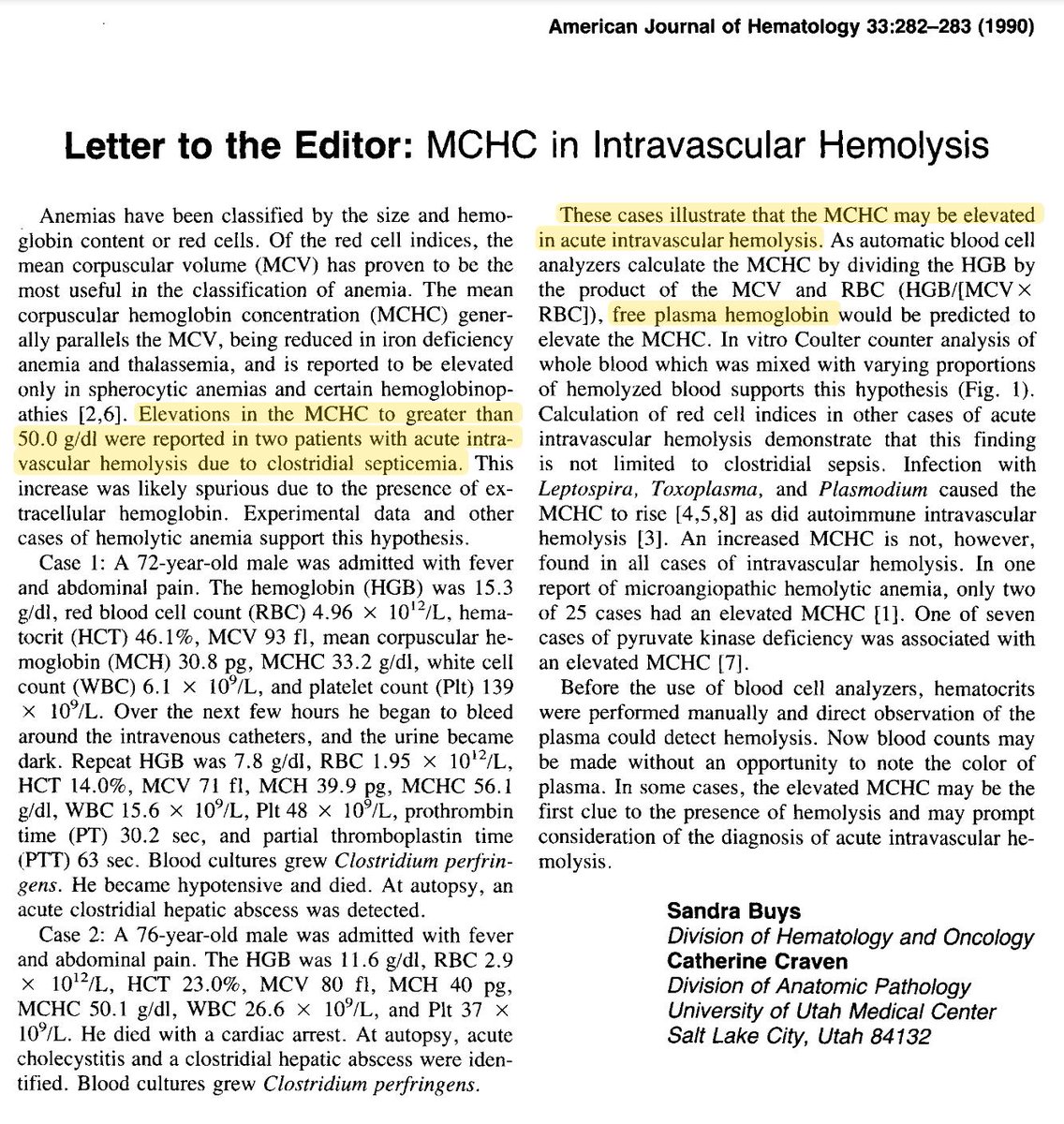
Intravascular hemolysis is an interesting example.
If enough Hbg is in the plasma after the RBC hemolyzes, it can be picked up when the Hgb is measured by the machine.
This letter provides a few case examples.
ncbi.nlm.nih.gov/pubmed/2316515
There are many studies demonstrating that "relative hypochromia" (i.e., a low MCHC) is correlated with poorer outcomes.
One study noted that even in nonanemic patients with heart failure, a low MCHC was associated with lower survival.
ncbi.nlm.nih.gov/pubmed/26897638
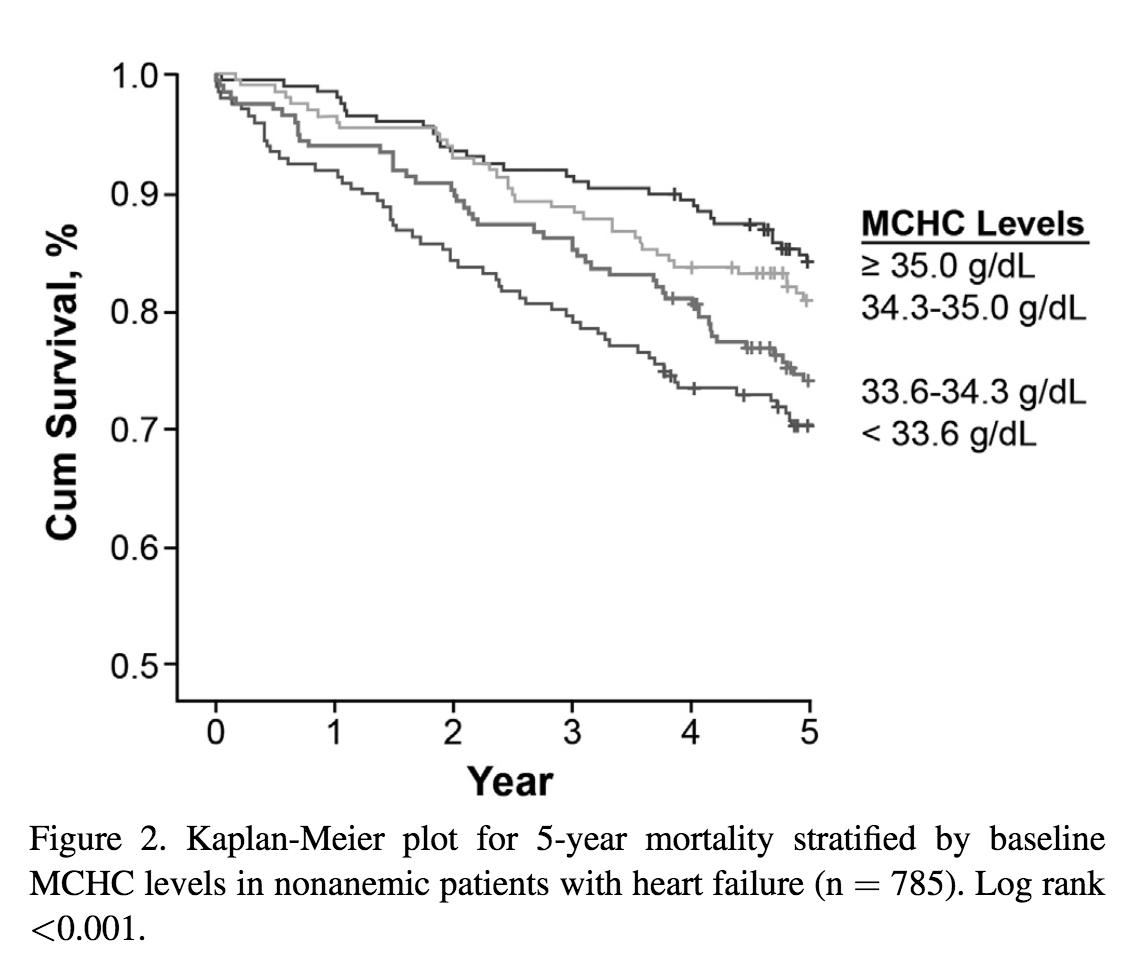
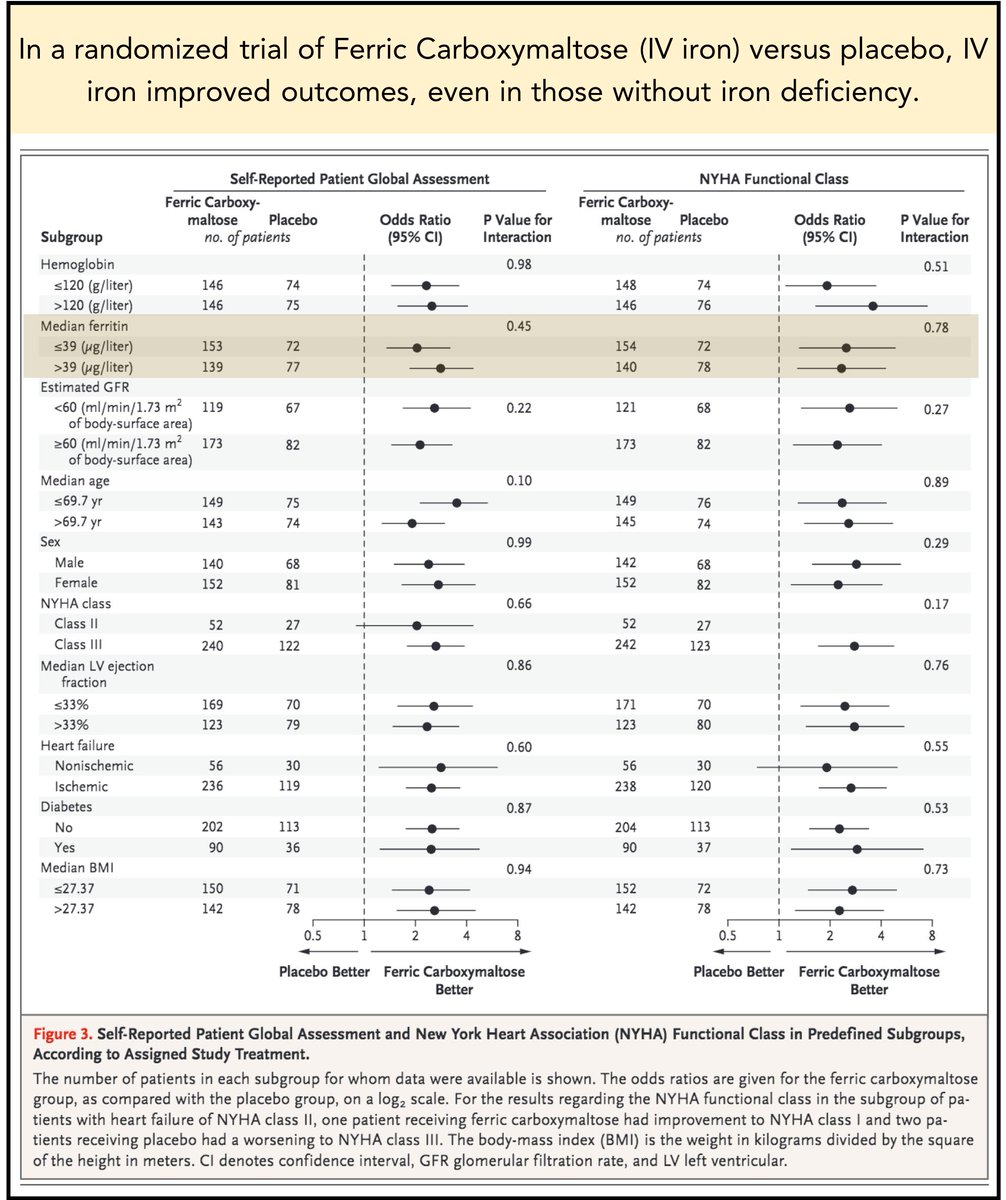
The correlation between low MCHC and poorer outcomes in heart failure patients may be related to iron deficiency.
And, as the FAIR-HF trial suggested, IV iron benefit patients with heart failure, even when anemia is absent.
ncbi.nlm.nih.gov/pubmed/19920054
Before summarizing, I'm curious whether this thread will change anyone's practice.
So, what do you think about MCH and MCHC now?
If you found any of this interesting, you can read more about the other glossed-over component of the CBC, the mean platelet volume (MPV) in this thread.
Since reading about MPV, I look at them far more frequently.
➢ MCH is more sensitive than MCV for iron deficiency, but neither is particularly good
➢ A high MCHC can be a clue to spherocytosis, intravascular hemolysis, and other diagnoses
➢ A low MCHC is associated with worse outcomes in heart failure