Why does cirrhosis predispose to "bacterial translocation"?
I have long heard that this is the mechanism of spontaneous bacterial peritonitis (SBP), but I hadn't understood why cirrhosis leads to more of it.
[Or where the bacteria translocate to...]
Let's have a look.
A question: which of the following contribute to the pathogenesis of SBP in patients with cirrhosis?
[TNF = tumor necrosis factor]
SBP is complex, with multiple factors contributing to its occurrence in those with cirrhosis.
At least three things are relevant:
➢ Bacterial overgrowth
➢ Increased intestinal permeability
➢ Altered immunity
Let's examine the first two.
ncbi.nlm.nih.gov/pubmed/15123075
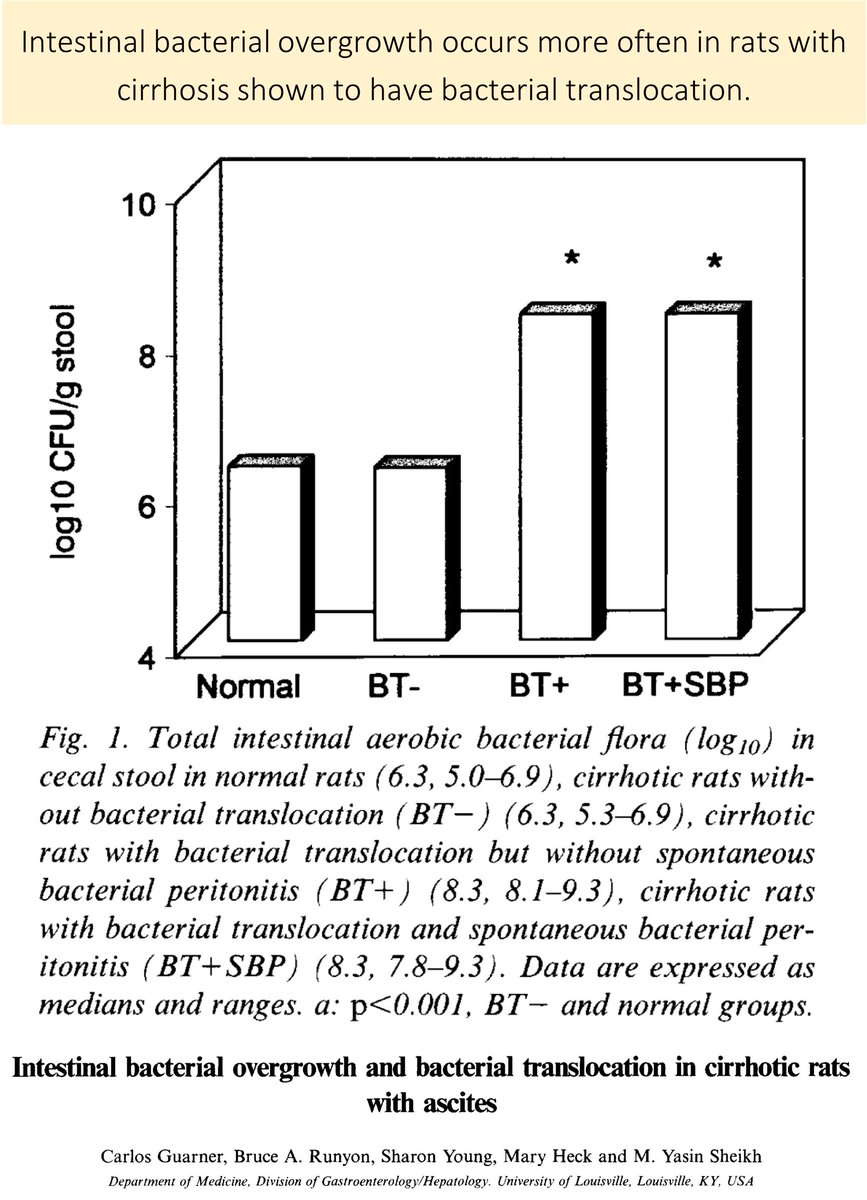
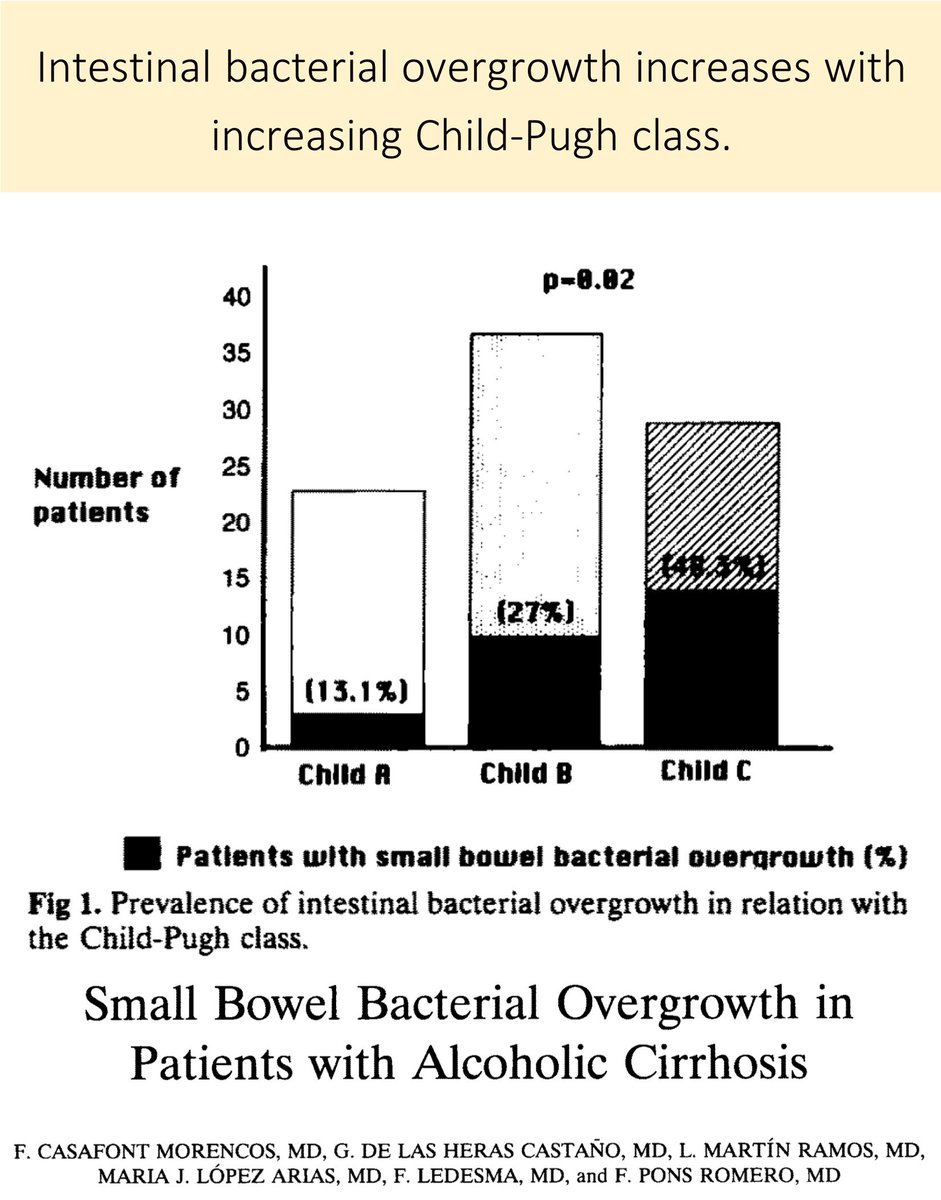
Bacterial overgrowth (BO) has been observed in rat models of cirrhosis and increases in frequency with worsening severity of cirrhosis.
As we'll see later, the bacteria that "overgrow" are those eventually cultured in SBP.
ncbi.nlm.nih.gov/pubmed/9210626
ncbi.nlm.nih.gov/pubmed/7781442
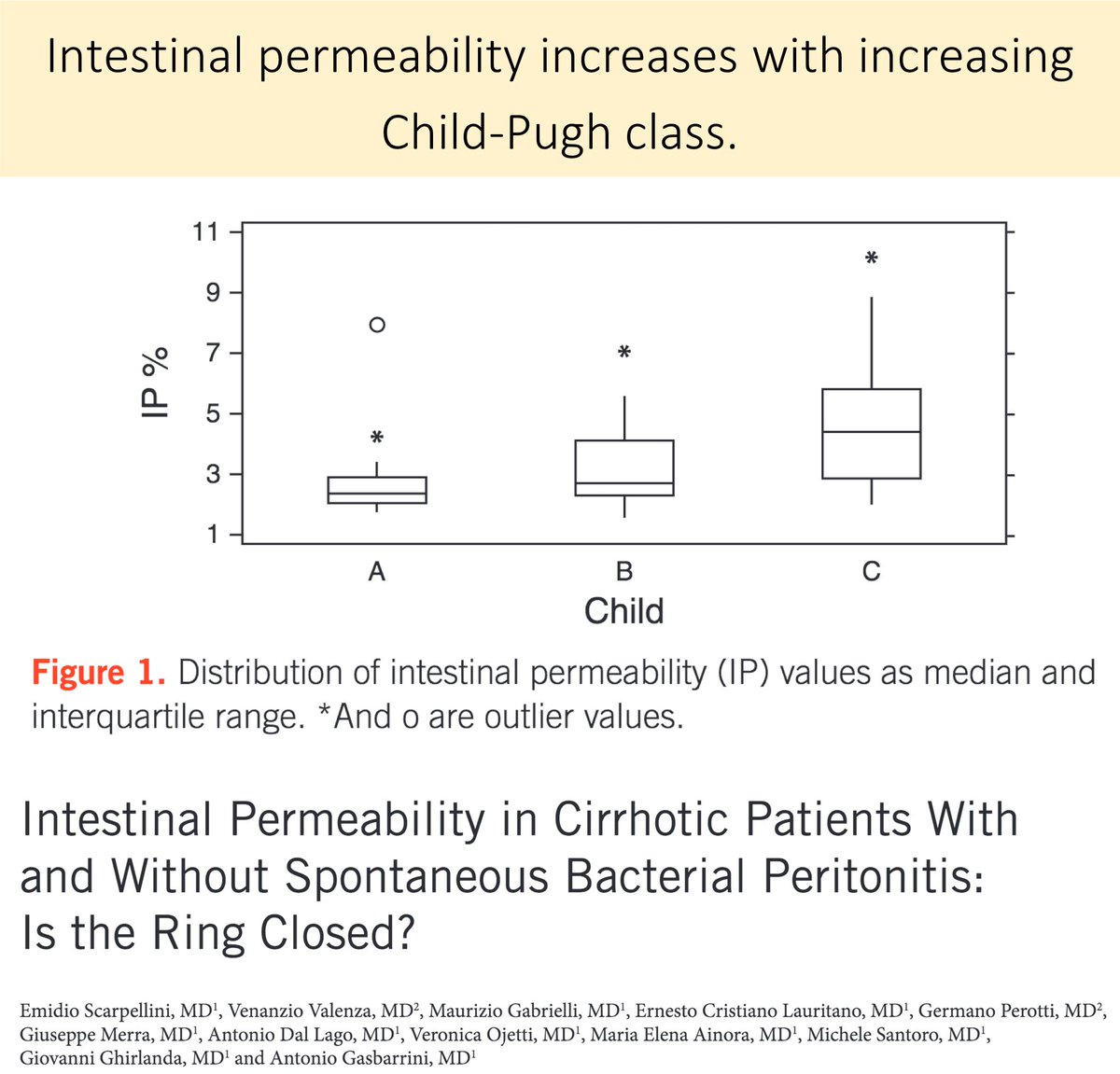
In addition to bacterial overgrowth, increased intestinal permeability increases the risk of SBP.
One study identified increased intestinal permeability in:
• 42% of those with cirrhosis (worse as Child-Pugh increases)
• 4% of controls
ncbi.nlm.nih.gov/pubmed/19844200
To recap thus far, cirrhosis is associated with:
➢ Bacterial overgrowth
➢ Increased intestinal permeability
But, where do the bacteria go next? Where do they "translocate" to?
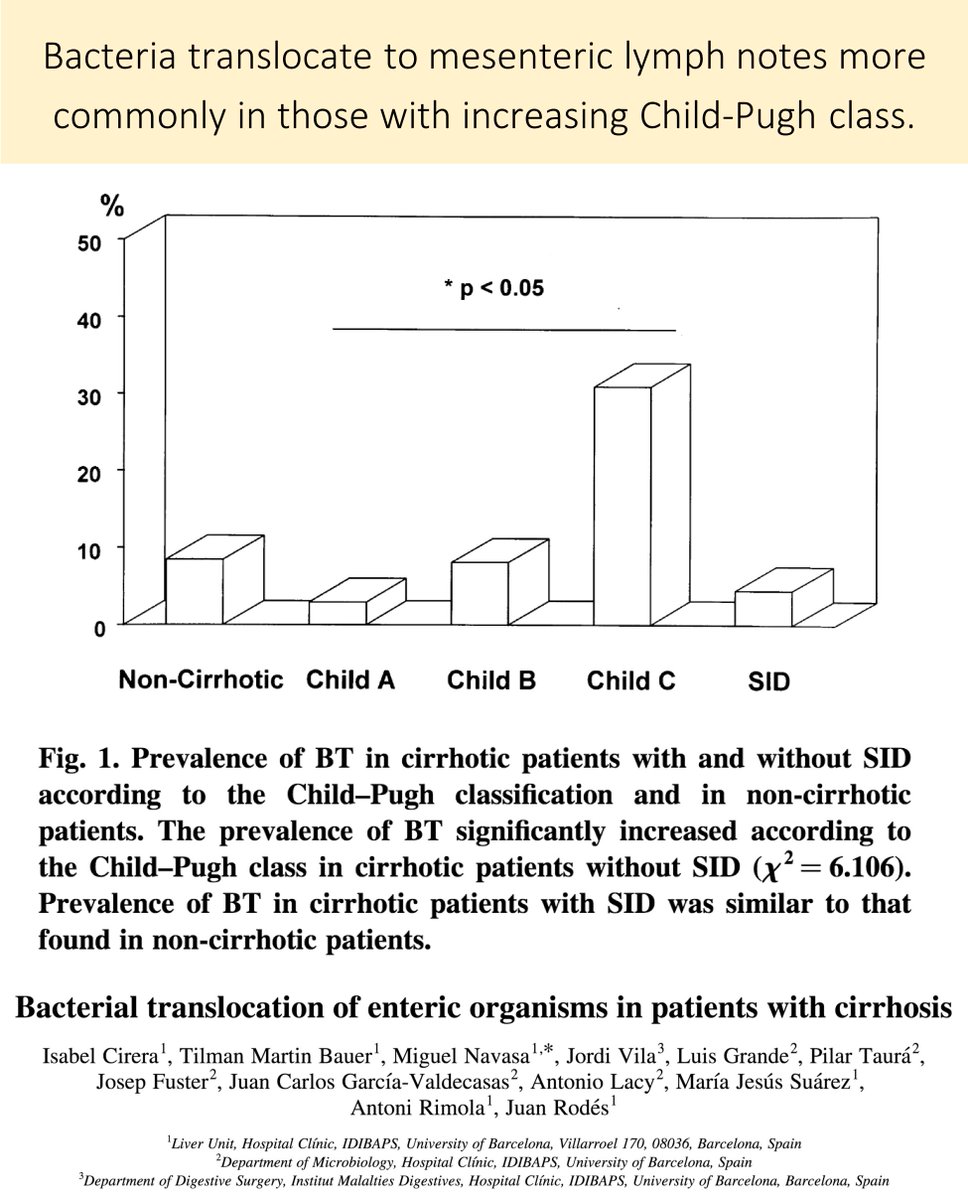
In the setting of BO and increased permeability, bacterial likely translocate to mesenteric lymph nodes first (MLN).
Unsurprisingly, translocation to the MLN is more common as the severity of cirrhosis worsens.
ncbi.nlm.nih.gov/pubmed/11211904
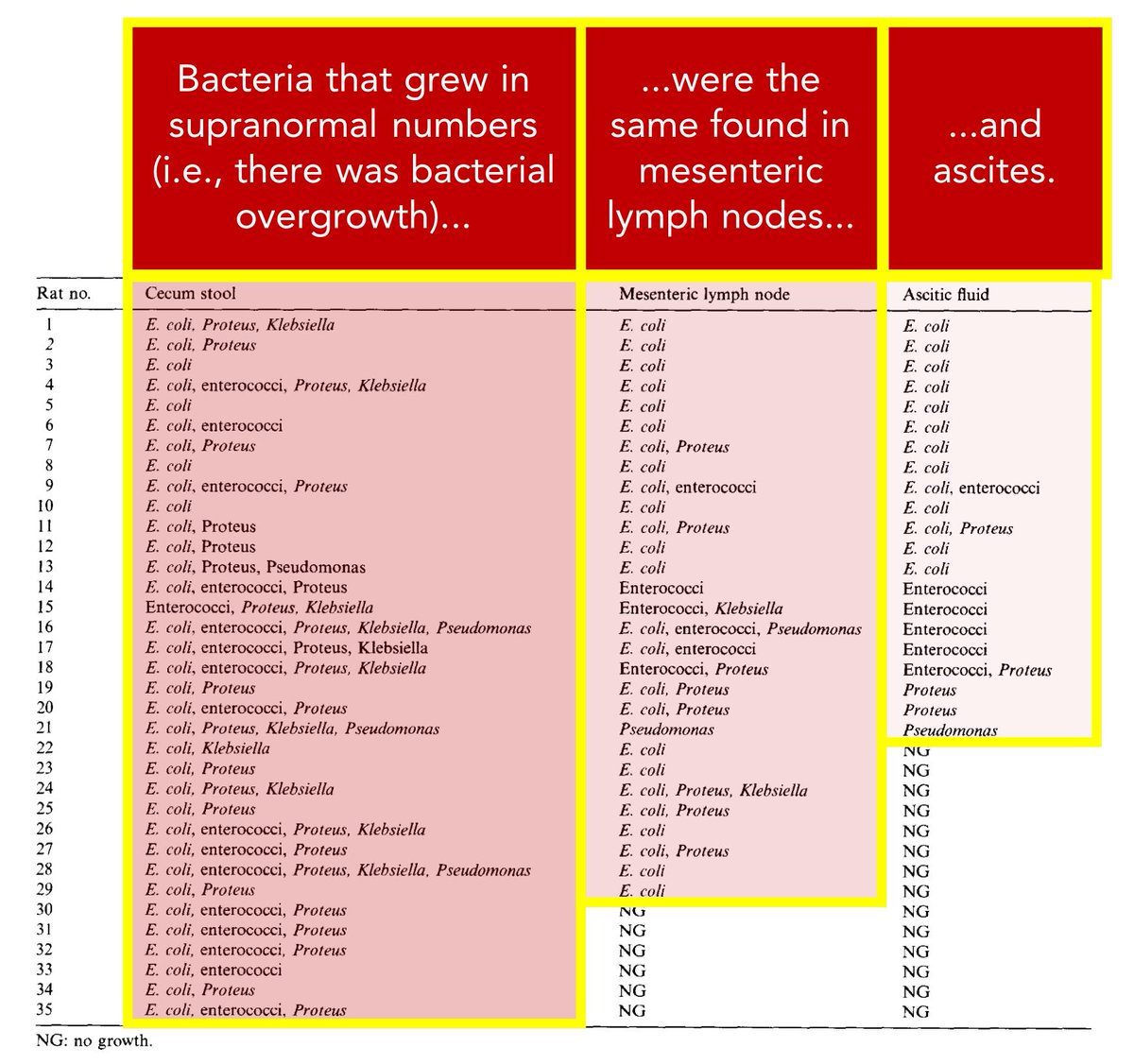
Returning to one of the studies in tweet 4, the bacteria that grew in ascites were the same found in MNL and the cecum.
And, the frequency of isolation was: cecum > MLN > ascites...
...suggesting that the MLN are intermediaries.
ncbi.nlm.nih.gov/pubmed/9210626
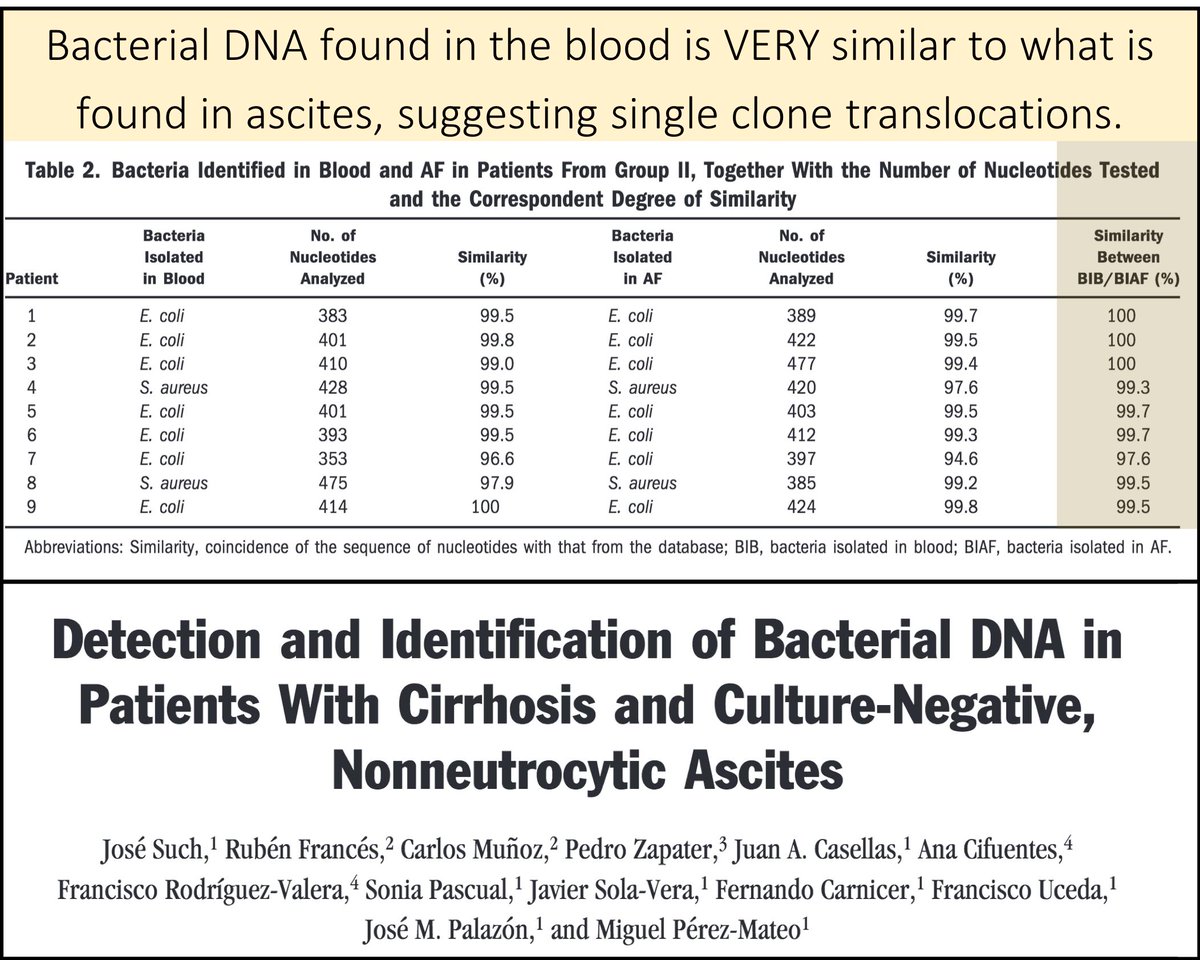
Another intermediary: the blood.
Though most patients with SBP don't have positive blood cultures, studies demonstrate genetically similar bacterial DNA in the blood and ascites of patients with cirrhosis.
ncbi.nlm.nih.gov/pubmed/12085357
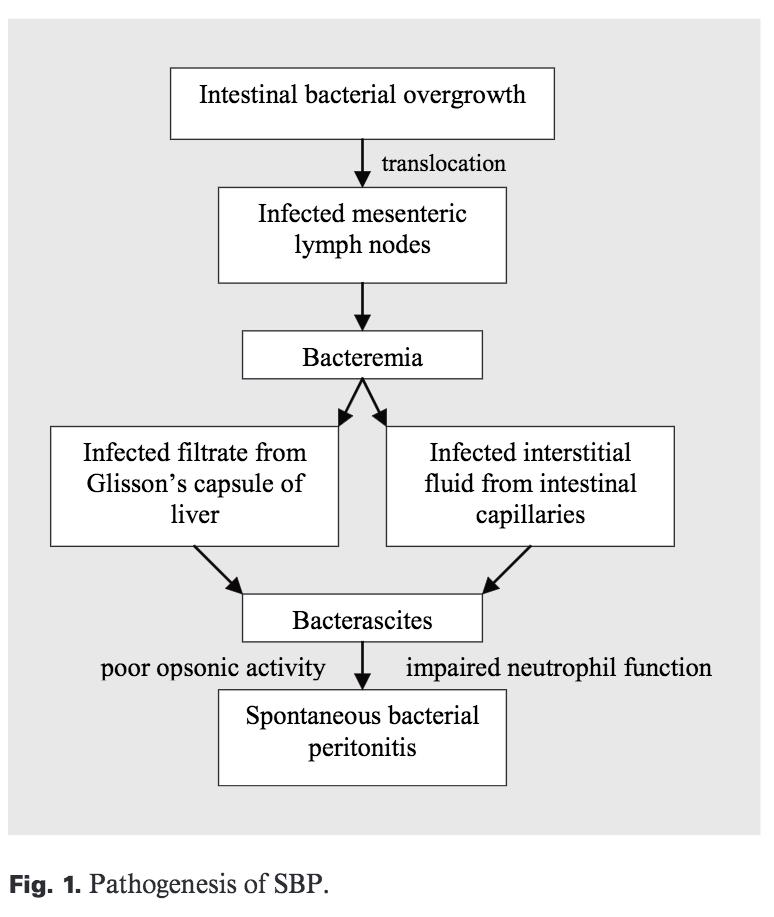
Putting it together, the sequence of events leading to SBP may be:
Bacterial overgrowth ➔ Translocation to mesenteric lymph nodes ➔ Bacteremia ➔ Ascites
Altered immunity likely contributes across many of these events.
ncbi.nlm.nih.gov/pubmed/15920324
Let's put some of this knowledge together.
First, which of the following might INCREASE the risk of SBP?
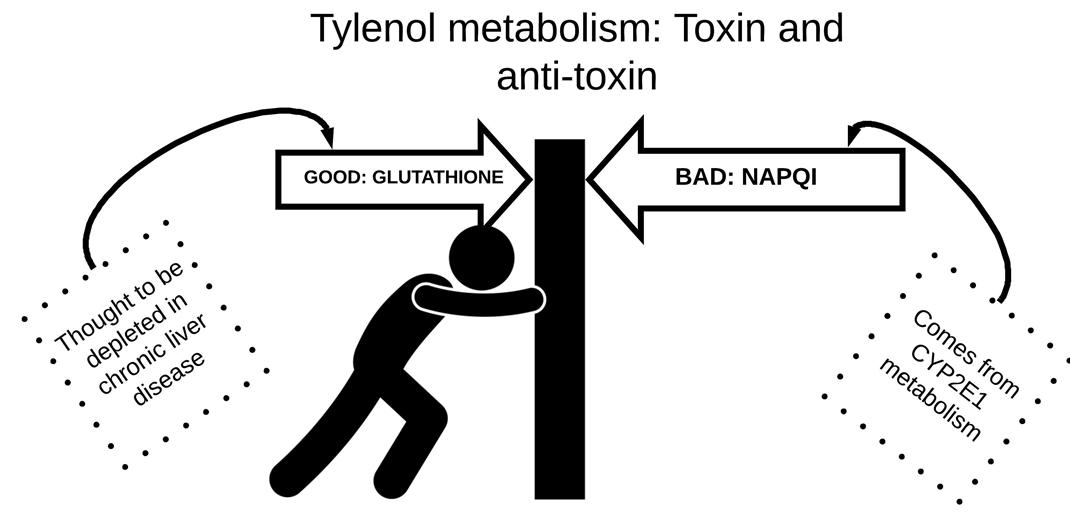
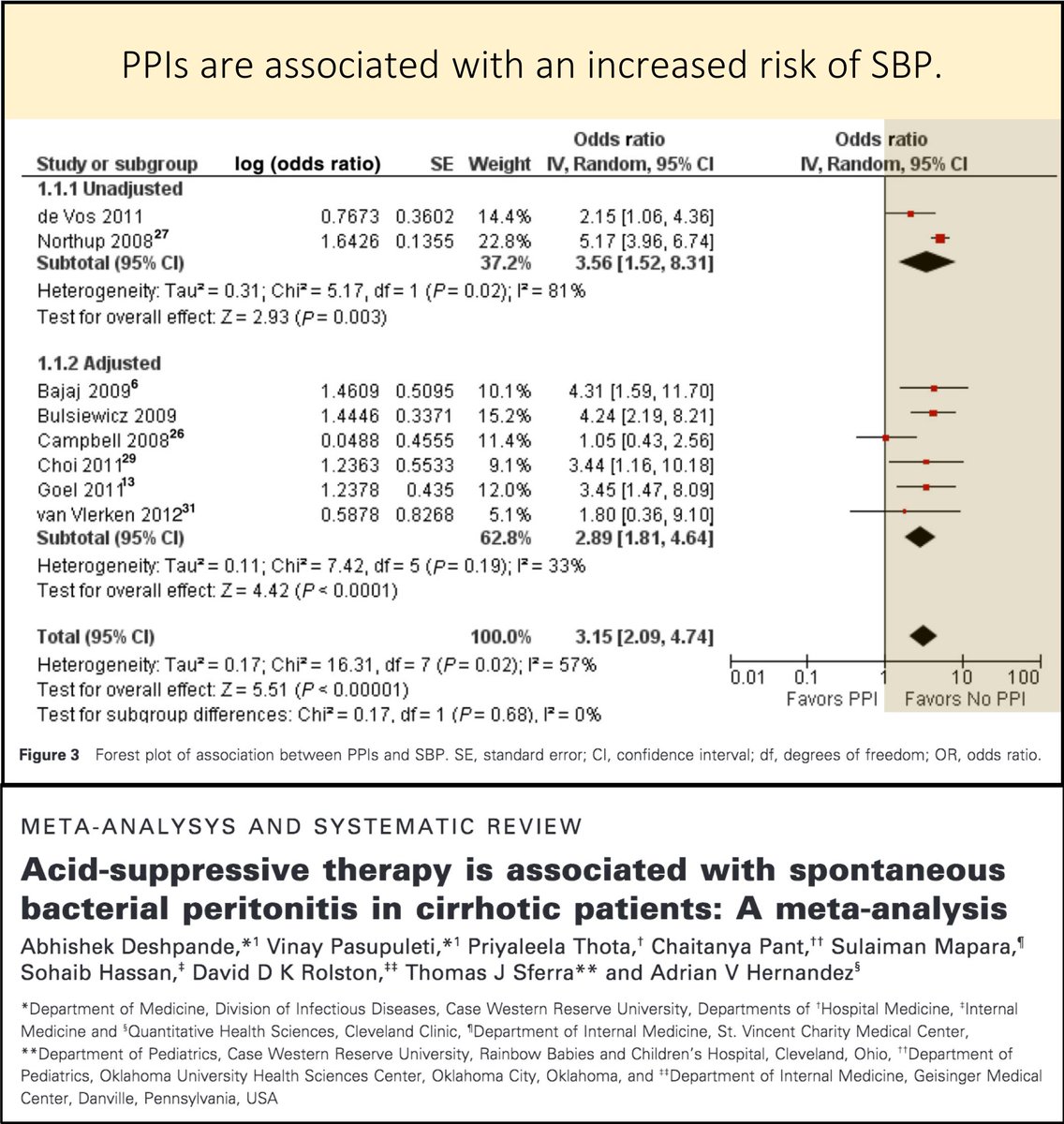
Given that proton-pump inhibitors (e.g., pantoprazole) likely increase bacterial overgrowth, they may predispose to SBP.
The data do not consistently show this association, but one meta-analysis supports the link.
ncbi.nlm.nih.gov/pubmed/23190338
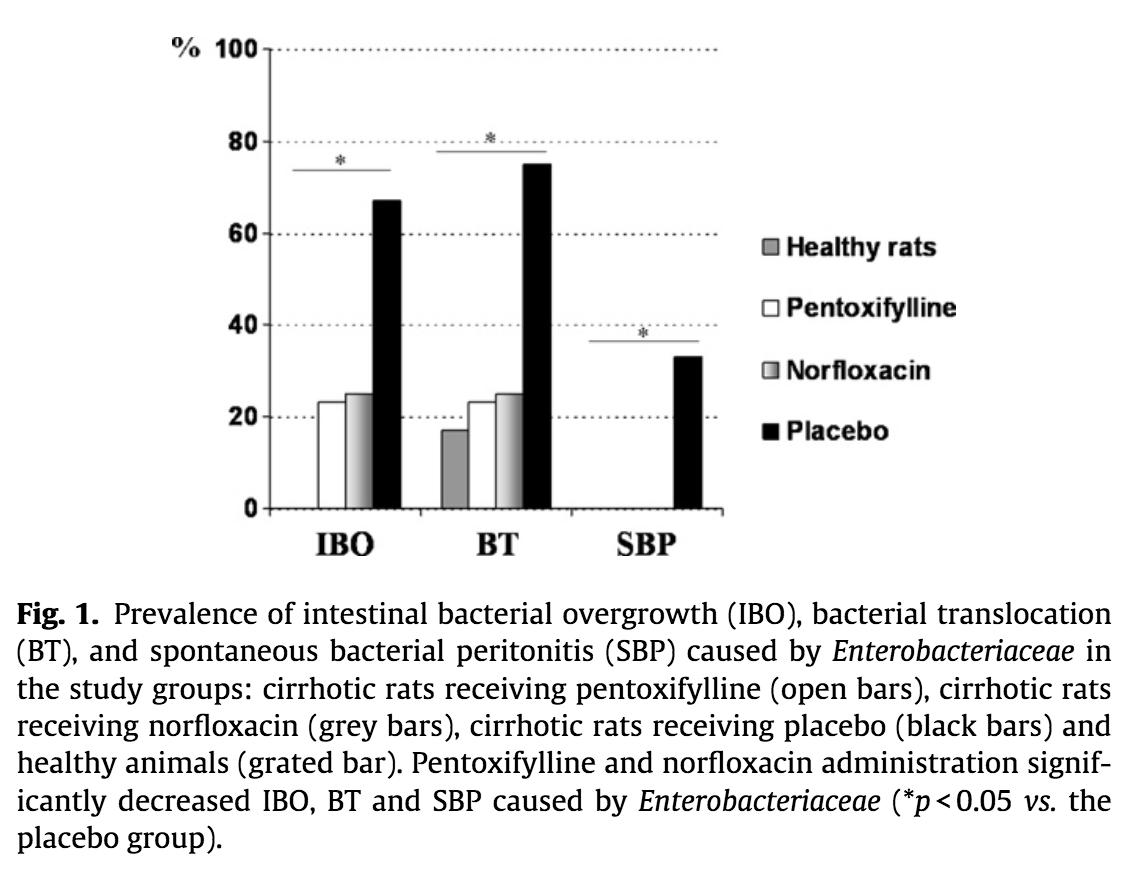
Unsurprisingly, agents that decrease bacterial overgrowth have been shown to reduce the risk of SBP. These include:
➢ Norfloxacin (and other antibiotics)
➢ Pentoxifylline
ncbi.nlm.nih.gov/pubmed/22119621
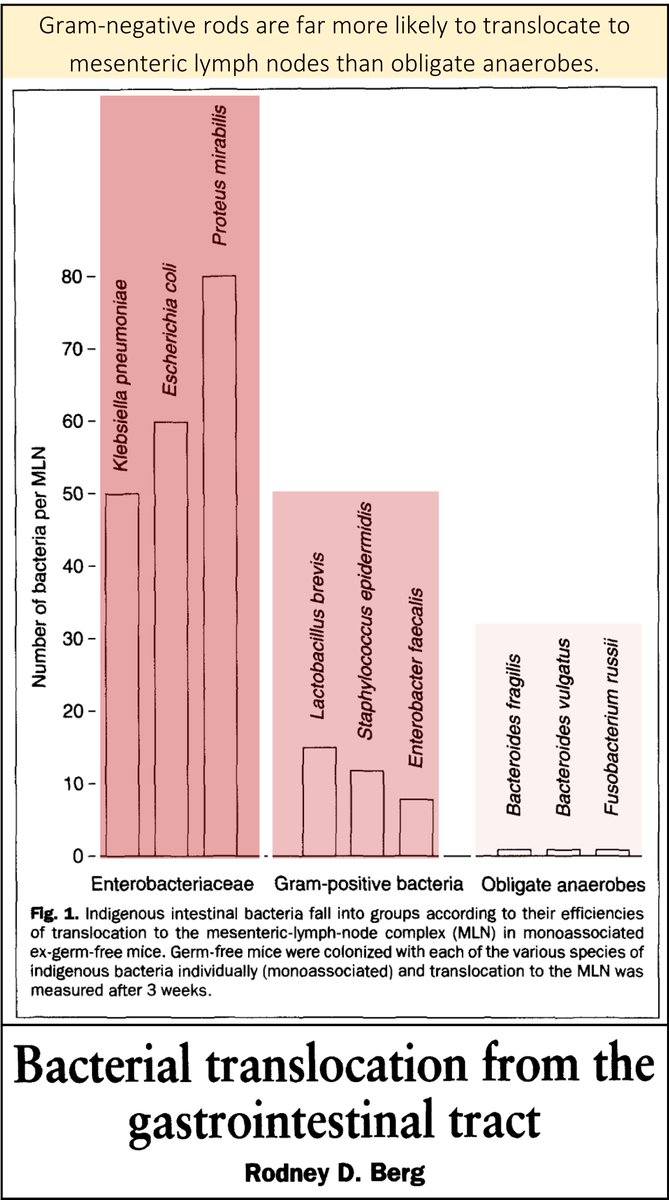
Have you ever wondered why we don't empirically cover anaerobes in SBP (even though we cover them in many other "GI" infections)?
➤Anaerobes don't translocate as well as gram-negatives and therefore cause less SBP and don't require empiric coverage.
ncbi.nlm.nih.gov/pubmed/7613757
Before closing, I want to highlight a great tweetorial by @ebtapper entitled "A celebration of paracentesis".
It covers why/how we should make the diagnosis of SBP.
💥Why does cirrhosis predispose to "bacterial translocation"?💥
➢ Bacterial overgrowth and increased intestinal permeability contribute to the risk of SBP
➢ Bacteria translocate to mesenteric lymph nodes, then blood, then ascites
➢ GNRs do this better than anaerobes