TWEETORIAL of GETUG-16 and hormone therapy with SRT
I have been asked many times to discuss this paper and my views on the topic now that the GETUG-16 was updated. It is a great trial with numerous strengths. So here we go…
@MCWardMD @RTendulkarMD @subatomicdoc #PCSM
Overall the trial can be viewed as positive or negative. How is this?
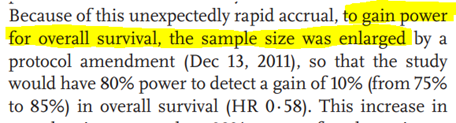
Original primary endpoint: PFS = was met!
Sample size was increased to be powered for OS, which was not met. So the endpoint the trial was actually powered for was not met = negative.
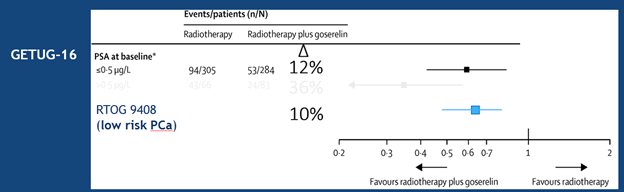
PFS should really not be used for ph3 trials. PFS basically equals BCR, which will near always be improved w/ ADT as you are inhibiting the PSA-based endpoint you are measuring. Even in RTOG 9408 low risk pts have a BCR benefit. Signal finding not practice changing.
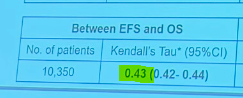
Is BCR/PFS a surrogate endpoint? No.
New ICECaP data shows PFS (they call it EFS) is a very poor surrogate endpoint for OS. Amazing lecture given from ICECaP statistician @Merregan showing how single trials using Prentice criteria are not enough to demonstrate surrogacy.
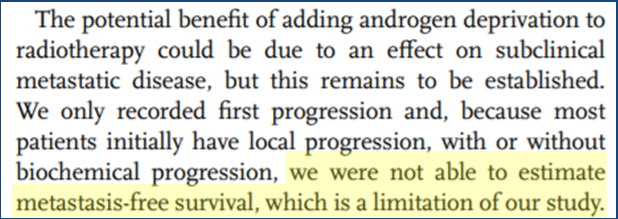
MFS- As stated in 2016 version and the update, MFS could not be calculated as they didn’t collect all mets events. They thus had to retrospectively ask sites, which are not blinded in any way. Thus, MFS is “hypothesis generating”.
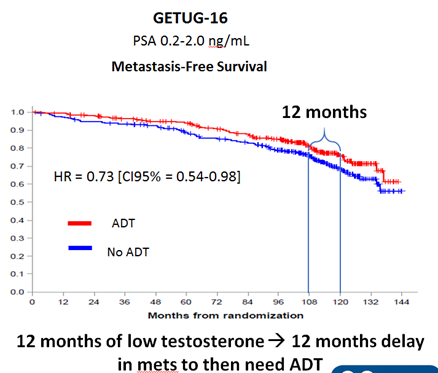
The improvement in MFS was not even really a “benefit”. Why?
6m ADT gives ~12m T suppression and side fx. Delay in MFS at median f/u was exactly 12m! Given developing M1 dz is common trigger for ADT, you simply delayed mets by duration of T suppression you induced upfront.
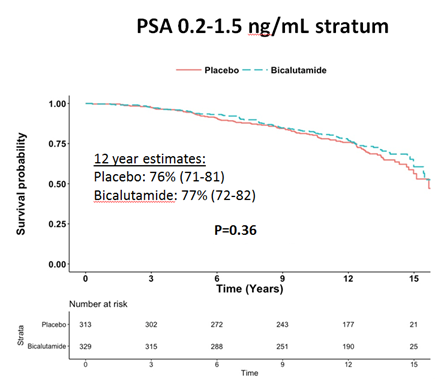
This was also shown in RTOG 9601 in patients with PSA <1.5 ng/mL (stratification factor and 85% of the cohort). Most men got 18-24 months of AA tx for a 18 month DELAY in mets. @DrewMoghanaki @NRGonc
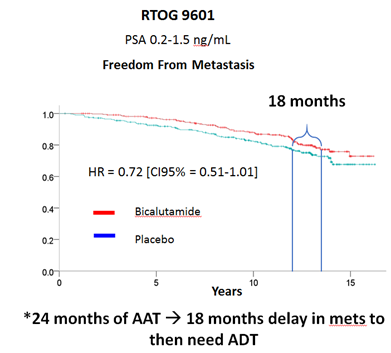
In RTOG 9601 or GETUG-16 the tails of the curve do NOT flatten out indicative of increasing CURE rates. Thus you simply are DELAYING patients by the duration of T suppression. HOWEVER, >85% of men at 10 years will never develop mets with early SRT and would never need ADT
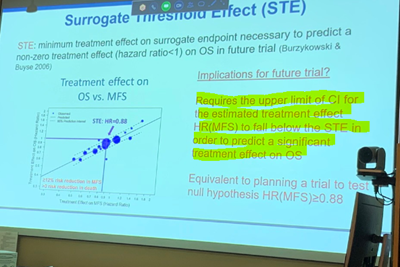
The GETUG-16 paper was mistaken to state that ICECaP supports that MFS would save them time and don’t need to wait for OS. Figure 5 of the JCO paper shows that HR >0.67 for MFS will not save any time and recommend using OS to infer survival improvement!

The surrogate threshold level in ICECaP for MFS was 0.88. The upper bound of 95%CI must be below this to indicate that OS will be improved. The upper 95%CI bound in GETUG-16 was 0.98 and thus, you CANT USE MFS differences this small to infer OS improvements.
@Merregan
Surrogacy is treatment specific. ICECaP included ZERO SRT trials, and included too few surgery trials even to demonstrate surrogacy in the subset of surgery trials as they state in the paper.
Thus, there is not high level data that MFS is a surrogate endpoint with SRT.
The argument put forth by @DrPaulNguyen and @RTendulkarMD that we need to wait longer for OS is likely inaccurate. RTOG 9601 for patients with PSA <1.5 ng/mL there was near identical OS results with 13 year median f/u. OCM becomes dominant this far out.
CONSPIRACY THEORY TIME :)
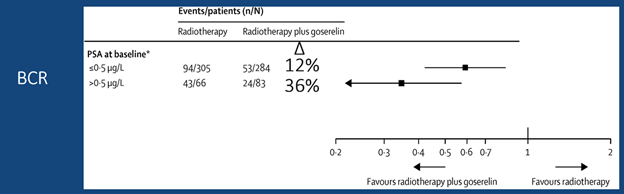
GETUG-16 reported outcomes by PSA in 2016 paper and showed a 3-fold greater benefit in PFS from ADT with late SRT than early SRT.
However, in the 2019 paper they oddly hid the PSA breakdown….hmmm
@MCWardMD @DrStish
Bottom line, we never have adopted ADT w/ RT unless there is an OS benefit (or very strong MFS signal like in M0CRPC trials). ADT improves BCR for low risk and FIR. Long-term ADT improves BCR and MFS in intermediate risk. Conclusively no OS benefit in men with lower PSAs
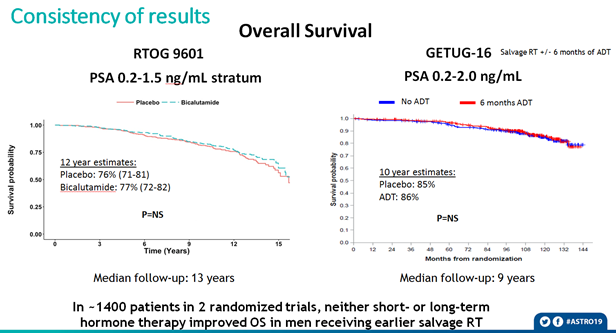
That's a wrap. You dont have to agree, but I believe just about every statement made has facts and data to back it up. ADT appears to be unnecessary for most men getting early SRT as most wont develop mets, and doesnt appear to increase cure rates but simply delay PSA rise