@MedDermSoc & @DermHospitalist Mini-Symposium on #COVID19 & #dermatology!!
I will be attempting to #livetweet the Zoom meeting!
Join along if you'd like. I will be using the h/t #COVIDDerm!
@RoxanaDaneshjou @dschless
Your cohosts are super excited to have you join. To give a little background, this meeting was planned in ~1 week, and we have over 500 RSVPs!
@MishaRosenbach now kicking us off with #COVIDDerm!

Reminder to do so here:
aad.org/covidregistry
#COVIDDerm
Powerhouse of #dermatologists!
#COVIDDerm
#COVID Toes
Urticaria
Morbilliform
Vesicular rash
Livedo reticularis
and more!
#COVIDDerm
Once the disease hit Italy, we saw our first report because #dermatologists were redeployed to the front lines which allowed for better characterization.
#CovidDerm
18/88 patients (~20%) had a skin manifestation.
Here's the paper: joidairouso.com/bb/img/207_2.p…
#COVIDDerm
Later on, a case series from Wuhan showed 7 critically ill COVID19 patients with distal ischemia (much more severe than just the toes, with frank necrosis).
#COVIDDerm
1 - virally mediated
2 - consequence of drug or other systemic disease
#COVIDderm
jaad.org/article/S0190-…
A Spanish paper with prospective data!
47% "maculopapules"
19% covid toes
9% vesicular (small monomorphic)
6% livedo or necrosis
19% urticarial
also - sickest patients had livedo, & most mild cases were pseudochilblains. maculopapules in btw.
#COVIDDerm
Could this be thrombotic? vasculitic? inflammatory? some mixed picture?
This paper from @JAADjournals is referenced, with mean duration of rash to be 8.7 days.
jaad.org/article/S0190-…
Notably, #COVID19 PCR was negative in the majority of those tested (very few tested). This was the case in 3 case series being presented.
#covidderm
Seems to look like regular pernio, per @lindyfox1.
#COVIDDerm
#covidtoes seem to be:
- in young healthy patients
- CAN have respiratory/other sxs
- Seems to be a later finding. Can have +PCR, but usually not. Should we worry about infectious poss?
- Most Ab testing has been negative
#COVIDDerm
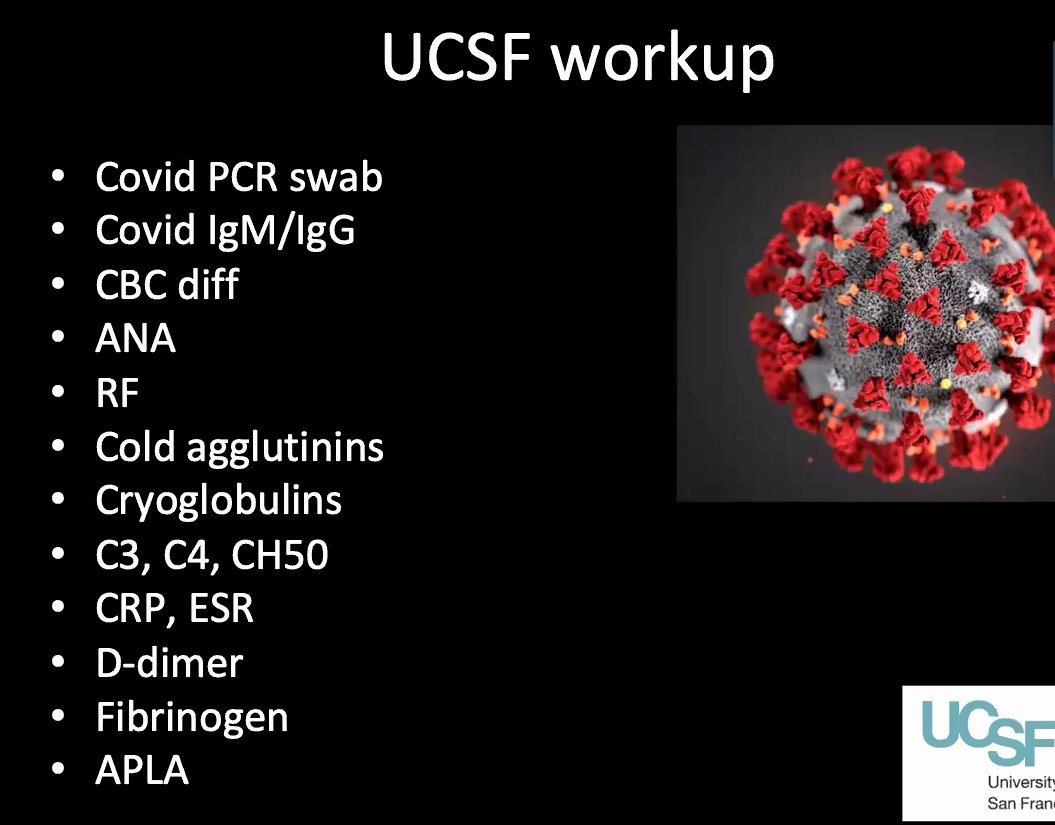
My personal take: I might avoid sending the entire work up if it's not going to change management.
HOWEVER - if it affects a patient's ability to return to work, or potentially donate plasma etc, I might send more.
#COVIDDerm
Some patients seem to have disease course that is much longer than the published ~9-13 days.
#COVIDDerm
#COVIDDerm
#COVIDDerm
Instead, acral livedo racemosa has been the most frequent finding!
#COVIDDerm
Skin bx was performed in 6 pts. all 6 had a pauci-inflammatory thrombogenic vasculopathy.
4/6 had arterial thrombosis!
3 of 4 died from thrombosis! (Stroke, PE)
#COVIDDerm
Perhaps this skin finding can help warn about soon to come coagulopathy!
#medtwitter #dermtwitter #COVIDDerm
This fits with the many thrombotic complications seen on autopsy, and all the clotting seen by the intensivists and #hospitalists!
Notably, these aren't patients going into DIC.
#COVIDDerm
- ?complement activation and deposition
- ?endothelial cell infection and endotheliitis
- ?antiphospholipid?
#COVIDDerm
- livedoid pattern may likely be a manifestation of systemic coagulopathy, especially if high d-dimer
- partner with #hematology, especially re: anticoagulation
#COVIDDerm
#COVIDDerm
Need to have ongoing dialogue with primary teams to make sure they understand our changed workflows
#COVIDDerm
Important to recognize that in-person evaluation is the gold standard.
#telemedicine has made in person eval much more efficient, making it easier to plan.
#COVIDDerm
Also need to think about billing! Unclear if time spent on the consult (even not face to face) is the only factor for billing. Good to keep track.
#COVIDDerm
#COVIDDerm
Most importantly - lack of data! So a lot of judgement is required!
#COVIDDerm
Important to have shared decision making process.
#COVIDDerm
- severity of underlying condition
- potential need for emergency care increasing risk of exposure if stopping immunosuppression.
- job exposures
- need for lab monitoring
- relative level of immunosuppression
#COVIDDerm
#COVIDDerm
Many biologics for #psoriasis show that biologic URI risk is similar to placebo. Based on paper from lebwohl in the @JAADjournals
#COVIDDerm
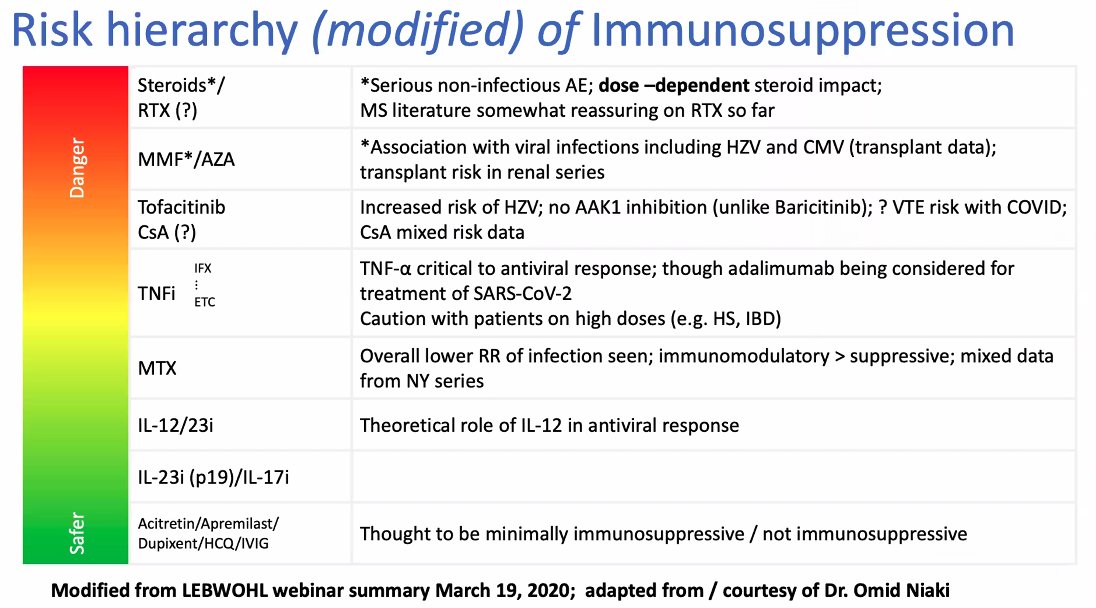
Paper from @JosephMerolaMD's group in @JAADjournals showed that azathioprine, prednisone, and mycophenolate are higher risk than methotrexate!
#COVIDDerm
jaad.org/article/S0190-…
BUT, new paper showed higher rate of ventilation with kidney transplant pts who get #covid19
#COVIDDerm
Check it out yourself, with encouragment from @JosephMerolaMD to check out the supplement!
#COVIDDerm
nejm.org/doi/full/10.10…
Lots more to study! Here's a slide regarding risk hierarchy edited by @JosephMerolaMD
#COVID19 #COVIDDerm #medtwitter #dermtwitter