1/🧵This figure from CHEST on early tracheostomy in #COVID19 pts is helpful for 2 reasons: it points out different ways of care. Read the BLUE circles clockwise & then switch to OUTER RED ARROWS clockwise again. Clear and True.
bit.ly/3w3DXfc
#medtwitter #nursetwitter
bit.ly/3w3DXfc
#medtwitter #nursetwitter
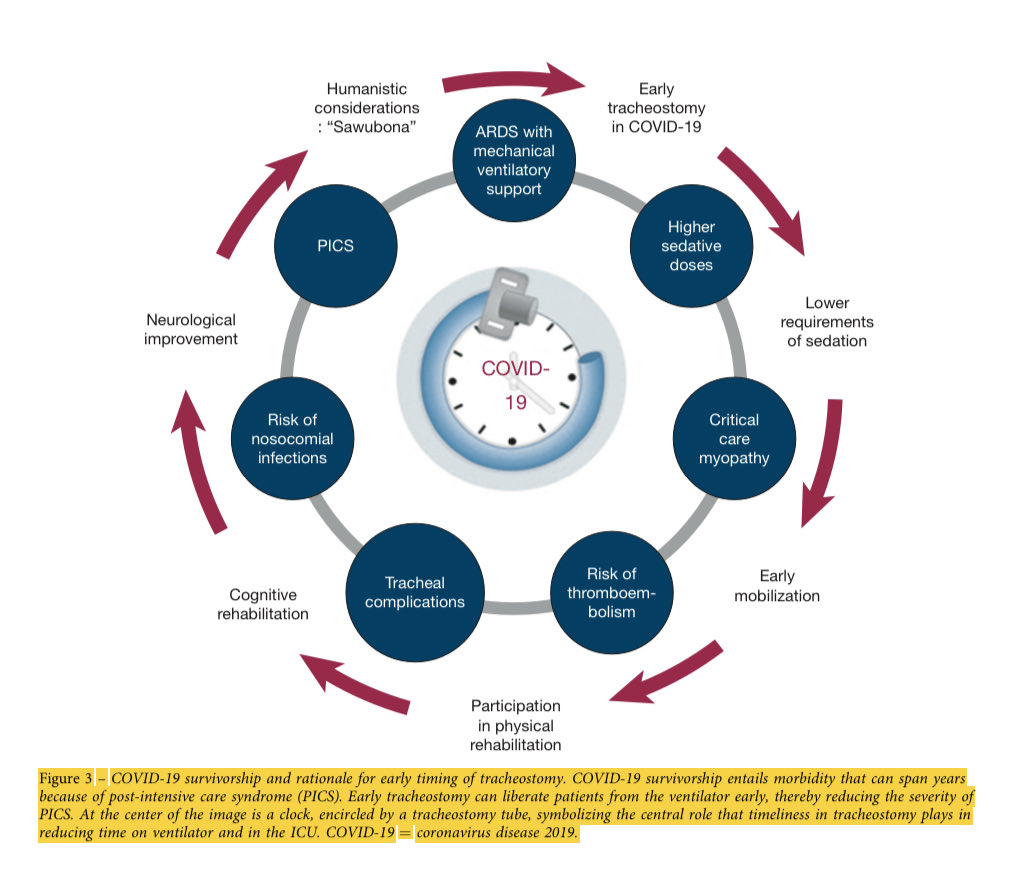
2/ The #COVID pt with ARDS + Sepsis on a ventilator is TOO often subjected to TONS of sedation, which adds brain injury, immobilization & development of physical disability. NEW DISEASES added to the original problem. We call this Post-Intensive Care Syndrome #PICS. 

3/ Early tracheostomy around day 10 can help (not always!) as outlined in the RED ARROWS. The goal is to lessen the added injury by waking people up, getting them out of bed and early mobilization plus talking with family. This is done via the #A2Fbundle. @SCCM 

4/ Do NOT think this is easy. It is not. It’s hard to orchestrate, especially when we have so many other #COVID patients to care for. But it’s our job every morning to try & to take each person’s life tenderly in our gaze & do whatever we can to prevent harm.
Get #vaccinated
Get #vaccinated
• • •
Missing some Tweet in this thread? You can try to
force a refresh