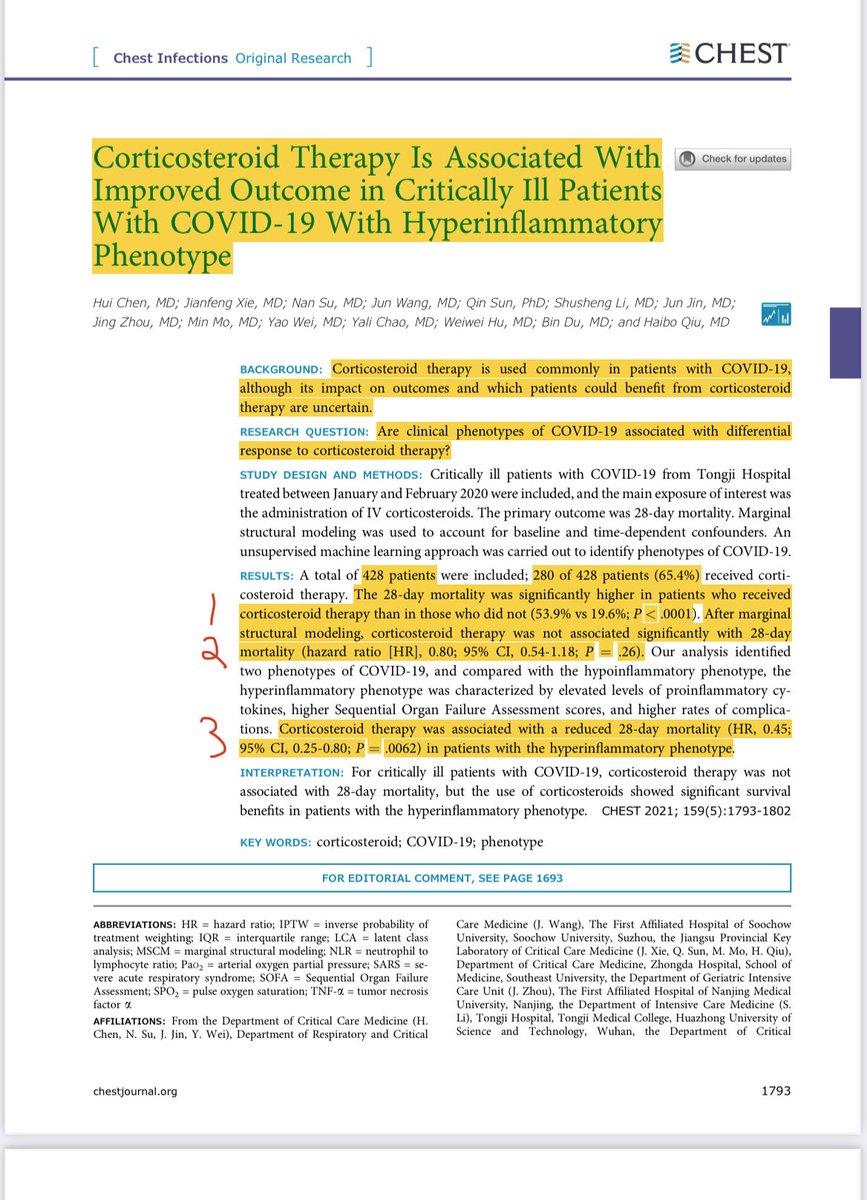
1/ Steroids in #COVID19?🧵
N=428. In 1 study we go from
1. statistically significant ⬆️ Deaths w steroids
2. to no difference by adjusting
3. to statistically significant ⬇️ Deaths by subgroup phenotyping of inflammation…
All in the same study? Let’s unpack this...
#MedTwitter
N=428. In 1 study we go from
1. statistically significant ⬆️ Deaths w steroids
2. to no difference by adjusting
3. to statistically significant ⬇️ Deaths by subgroup phenotyping of inflammation…
All in the same study? Let’s unpack this...
#MedTwitter
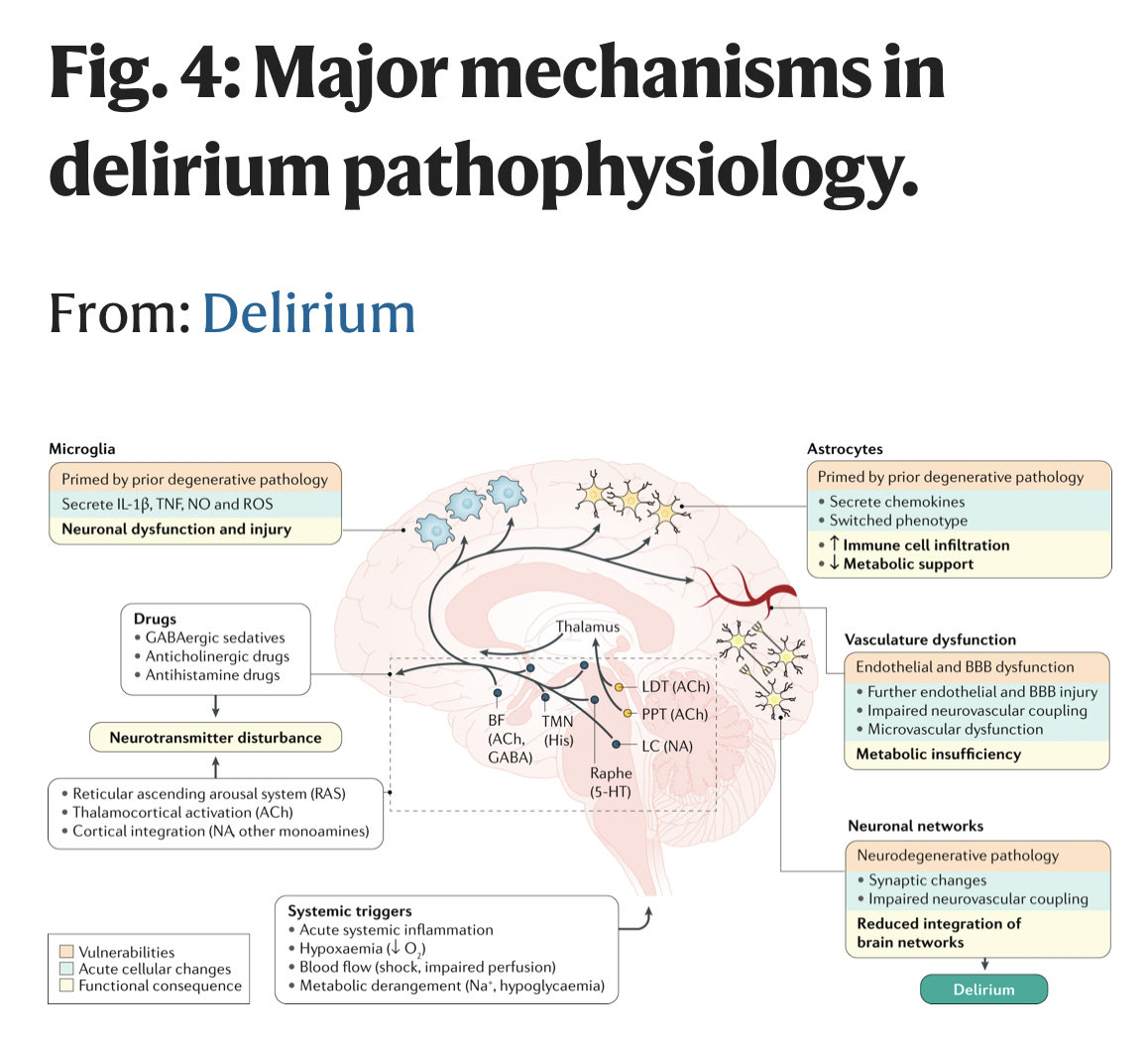
2/ Chen et al built on a 2014 @LancetRM study by Dr. Calfee of 1,022 pts, showing that sick people on a ventilator w ARDS (think #COVID19) are of 2 types, 1 of which is Hyperinflammatory (storm of inflammation) who might benefit from drugs like steroids.
bit.ly/3o3t8qV
bit.ly/3o3t8qV

3/ First Chen tried to overcome the biases associated with their observational data & showed that some observational methods (eg, multivariable regression including baseline SOI) can give the exact wrong answer (HR 1.97) because it does not include temporal biases.
4/ The same mistake was made early in #COVID with a bunch of hydroxychloroquine & anticoagulation analyses. I agree w their point that a large well-done observational study will provide superior results to a meta-analysis including poorly conducted observational data
5/ Then they adjusted for temporal associations in a way that flipped the direction of the signal but failed to reach significance (HR, 0.80; 95% CI, 0.54-1.18; P 0.26); which may be real but just underpowered.
6/ Then, they looked for different phenotypes, like Dr. Calfee’s study, based on inflammatory markers & found that the hyperinflammatory phenotype benefitted independent of baseline respiratory status, and a group that did not benefit, independent of baseline respiratory status. 



7/fin
To conclude, we are currently giving steroids to all sick #COVID19 ICU pts based on RECOVERY & other studies. It is very likely NOT benefiting all pts & likely causing harm to some (eg, ⬆️ sugars, ⬇️ wound healing, extra infections)? We need more data & other options!
To conclude, we are currently giving steroids to all sick #COVID19 ICU pts based on RECOVERY & other studies. It is very likely NOT benefiting all pts & likely causing harm to some (eg, ⬆️ sugars, ⬇️ wound healing, extra infections)? We need more data & other options!

• • •
Missing some Tweet in this thread? You can try to
force a refresh