1/🧵#COVID19 Compassion
Our patient wants to live 3 days to see his grandson graduate. He has #COVID19 pneumonia & is extremely short of breath. He’s chosen NOT to go on a ventilator & is on 100% O2 HiFlow Canula. He’s afraid of tight-fitting a bipap mask.
#PalliativeCare
Our patient wants to live 3 days to see his grandson graduate. He has #COVID19 pneumonia & is extremely short of breath. He’s chosen NOT to go on a ventilator & is on 100% O2 HiFlow Canula. He’s afraid of tight-fitting a bipap mask.
#PalliativeCare
2/ The intern said, “I never saw a patient whose respiratory rate was twice his oxygen saturation!” Yep, last night his O2 sats dropped to 30% and he was breathing 60 times a minute! By morning he was 85% sat and RR was 28. Better but tenuous.
#TipsForNewDocs #MedStudentTwitter
#TipsForNewDocs #MedStudentTwitter

3/ All of this raises some complicated ethical + treatment questions that I’d like to cover. We addressed this on rounds several times this week & at times it got a bit heated. His #nurse said she noticed herself flushed, mad, and heart rate >130…why? 

4/ We have #nurses present their patient on rounds, and she was anticipating we’d disagree with her ideas. #Nurses deserve autonomy and respect. We use the #A2Fbundle format & it takes them ~60 sec. This is well worth trying if you’re aren’t currently rounding like this.
5/ So his nurse compassionately told us that he had great urine output and was on all the right meds, but he was still getting worse, more anxious & out of breath. A Facetime visit w his #family, who are quarantined w #COVID, lifted his spirits a ton. Before that…
6/ Before visiting with his family, he was giving up completely, but now he said, “PLEASE keep me alive to see him graduate! This is worth everything to me.”💥 Family proved better than any anti-depressant. This is the essence of #A2Fbundle & humanism: 👁 the full person.
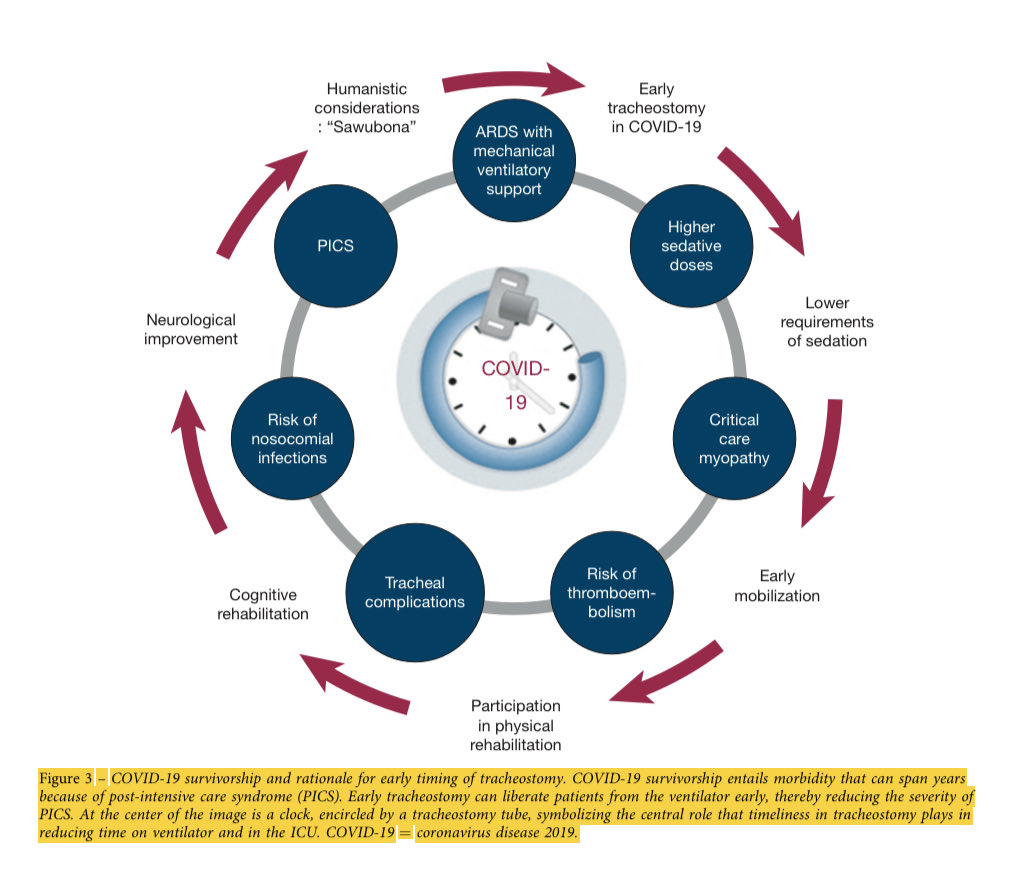
7/ the 🕰 is ticking: it’s not what’s the matter WITH the patient, but what matters TO him. He told us his immediate goals. 1. Reduce my suffering in whatever way possible. 2. I want to stay alive until graduation. But medical care is maxed out, right?
NO.
NO.

8/ Treatment Care vs. Comfort Care:
Remember to treat the patient not the numbers. His nurse asked for morphine to ⬇️ his “air hunger.” Early in COVID, she’d been told “no” unless the patient had been converted to full “comfort care.” Is that a hard & fast rule? No.
Remember to treat the patient not the numbers. His nurse asked for morphine to ⬇️ his “air hunger.” Early in COVID, she’d been told “no” unless the patient had been converted to full “comfort care.” Is that a hard & fast rule? No.
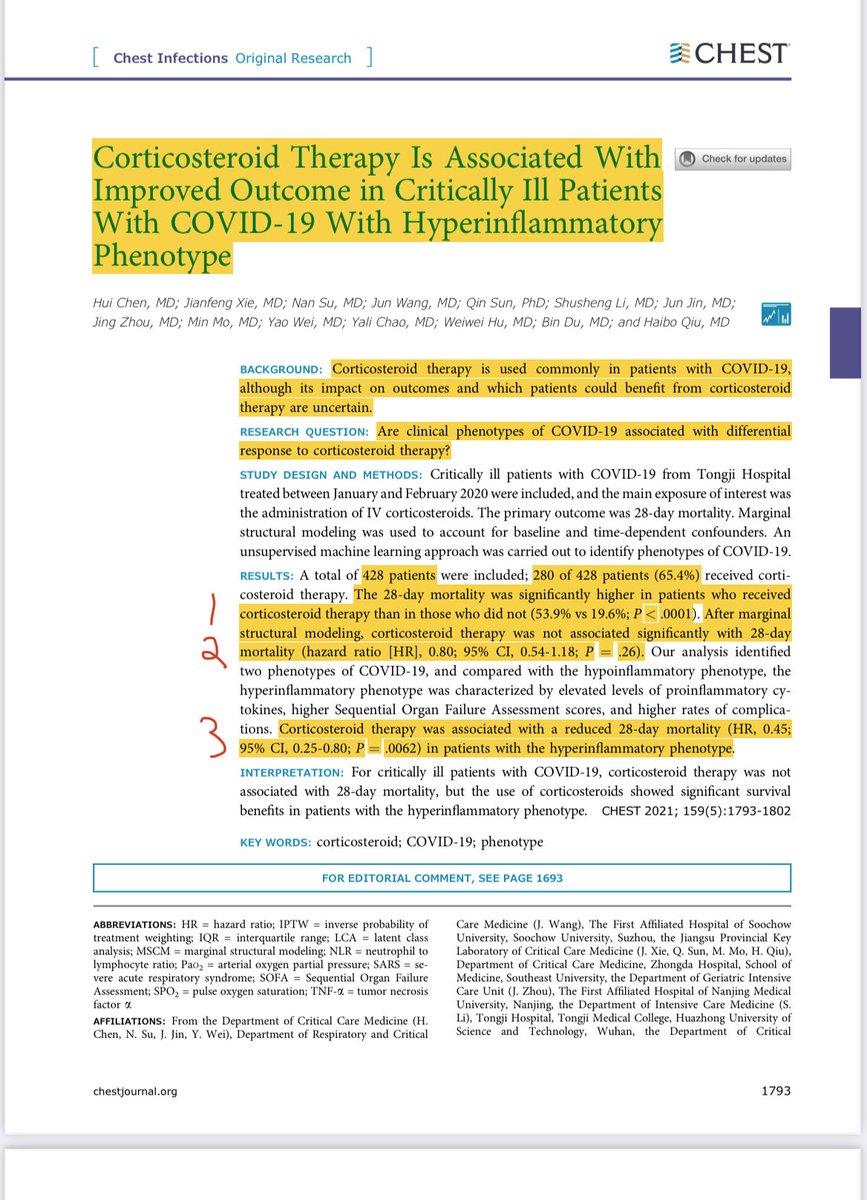
9/ Narcotics (eg, morphine) dampen the perception of shortness of breath. We give 1-4 mg Morphine every several hours when pts are at end-of-life to keep them comfortable, reduce suffering, and allow death to come peacefully. It is kind, dignified, and humane. What about now?
10/ Such care is not done w intent to end life. We are removing pain and suffering. The principle of “double effect” states that it is ethically sound because any unintended shortening of life that occurs by respiratory suppression from the morphine was not the primary intent.
11/ The Dilemma: Although he doesn’t want heroic measures like CPR, he is still getting lots of active COVID therapies and wants to live long enough to experience his grandson’s graduation in 72 hours over zoom. So can we invoke #PalliativeCare? Yes!
12/ His nurse had the right call. His air hunger had to be mitigated. We prescribed low dose morphine & I felt the nurse idea was right, caring, loving, and smart! We have a primary obligation to reduce his suffering. Period. But we can do that AND help him get to Graduation.
13/fin
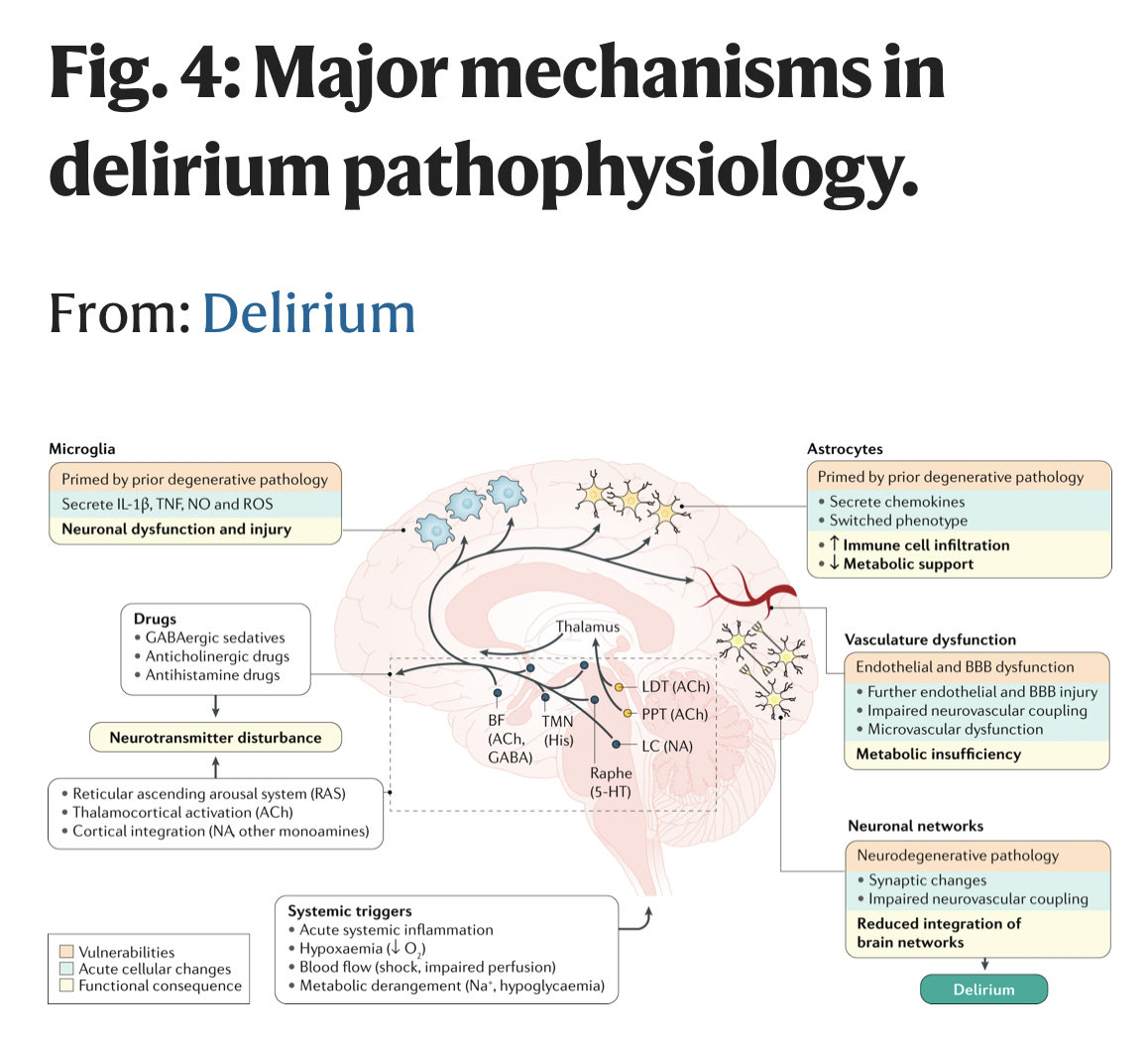
She also asked for an antipsychotic or dexmedetomidine to calm him without suppressing breathing. This combination of morphine plus dex was excellent. He kept breathing & was calm w/out nearly as much suffering. Each day, we will titrate to accomplish his stated goals.
She also asked for an antipsychotic or dexmedetomidine to calm him without suppressing breathing. This combination of morphine plus dex was excellent. He kept breathing & was calm w/out nearly as much suffering. Each day, we will titrate to accomplish his stated goals.
• • •
Missing some Tweet in this thread? You can try to
force a refresh