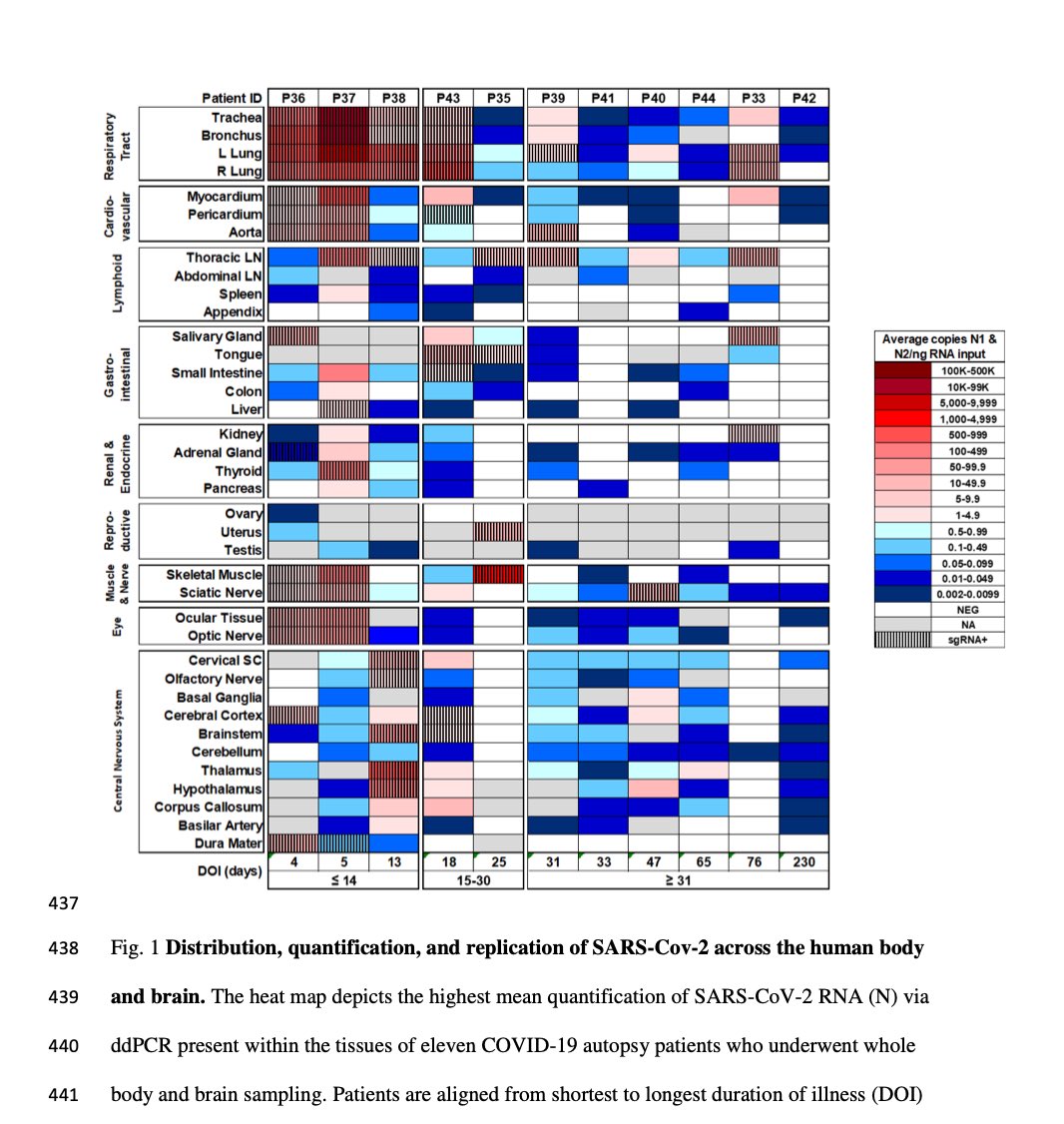
People are asking me: what if we did a similar autopsy study to look for #viruses in ME/CFS? Well, several teams that performed single autopsy studies on #ME/CFS patients found evidence of persistent enterovirus infection in subject brain/body tissue
https://twitter.com/microbeminded2/status/1473721448342687754
2/ Enteroviruses are (like SARS-CoV-2) single-stranded RNA viruses. They include the coxsackieviruses, poliovirus, echoviruses + rhinoviruses. These viruses cause about 10–15 million #infections each year in the USA alone
3/ This 1994 ME/CFS autopsy study identified positive PCR sequences with similarity to coxsackievirus B3 in samples from the #brainstem and hypothalamus (and also in muscle and heart tissue): acpjournals.org/doi/10.7326/00…
4/ This 2001 ME/CFS autopsy study found enterovirus VP1 protein in small blood vessel fibroblasts of the cerebral cortex + a patchy distribution of the VP1 protein in a small fraction of brain glial cells: tandfonline.com/doi/abs/10.130… 
5/ In 2015 Dr. John Chia presented an ME/CFS autopsy report at a scientific conference where he found #enterovirus RNA in the brainstem, lateral frontal cortex, occipital lobe + cerebellum. However results were never formally published. 

6/ It blows my mind that the ME/CFS research community has largely not followed-up on these findings. There has been little interest in autopsy studies generally, let alone studies that look for #virus in the brains/bodies of patients
7/ At @polybioRF we are working to change that. We are trying to set up an innovative postmortem (autopsy) #ME/CFS research program. If you are a scientist who wants to get involved, or a private donor who wants to support the effort let us know!
• • •
Missing some Tweet in this thread? You can try to
force a refresh