1) Welcome to a new #accredited #tweetorial on parenteral #antiplatelet therapy in #neurovascular interventions. Our expert author is Fawaz Al-Mufti MD @almuftifawaz, interventional #neurologist Interventional Neurologist @NYMedcollege @WestchesterMed @neurocritical @svinsociety 

2) This program is intended for #healthcare providers & is accredited for 0.5h CE/#CME for #physicians #PhysicianAssociate #nursepractitioner #nurse #pharmacists and is supported by educational grants from AstraZeneca, Bayer, and Chiesi.
3) Be sure to see prior tweetorials on #antiplatelet management, still available for credit, at cardiometabolic-ce.com/category/plate…. Faculty disclosures are listed at cardiometabolic-ce.com/disclosures/.
4) Pretreatment with dual antiplatelet therapy #DAPT is recommended to⬇️incidences of both ischemic &hemorrhagic complications in #neurovascular interventions.
5) Data are limited, however, re the optimal timing, dose, and duration of treatment for #carotid artery #angioplasty with stenting #CAS, especially in emergent stenting for complete or near complete occlusion of the internal carotid #ICA.
6) So let's consider a case that illustrates this. An octogenarian ♂️ with HTN/HLD/CAD presents with severe dysarthria, L homonymous hemianopia. Flaccid L sided face/arm/leg hemiparesis, and profound neglect.
Last know normal=8 hours ago. Baseline mRS=0.
Stroke Code is called.
Last know normal=8 hours ago. Baseline mRS=0.
Stroke Code is called.
7) Time is brain!
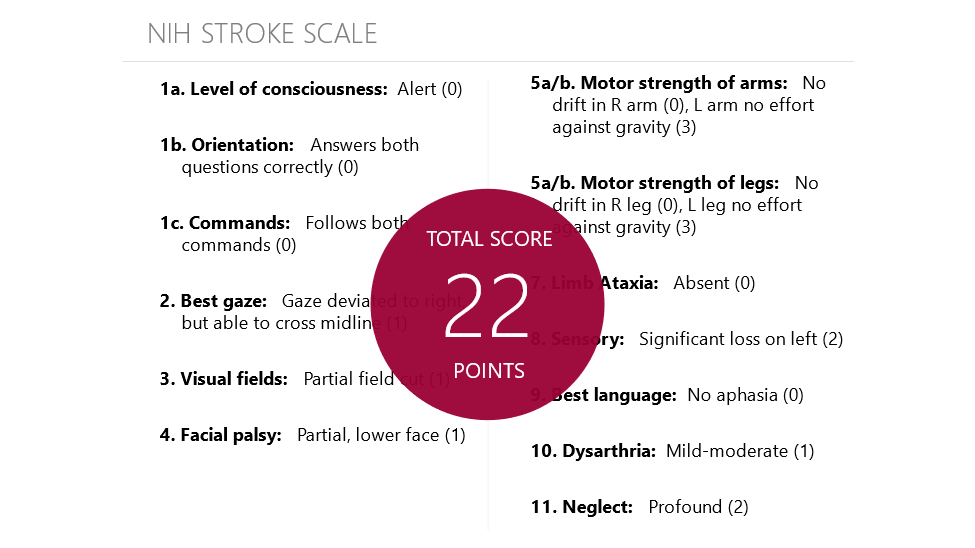
8) An #NIH #StrokeScale is calculated on this gentleman. (It takes practice, but there's a handy calculator available at mdcalc.com/nih-stroke-sca….)
It's not good--22.
It's not good--22.
9) So we must assemble the #stroketeam. #Neurology & #EmergencyMedicine are on the ⏰to plan an immediate treatment approach. CODE BAT (Brain ATTACK)
10) Gather data:
VS: BP 180/102, HR 85, RR 18, T 98.6
LABS: Glucose 110 mg/dL, Labs pending
EKG: EKG not done yet, but normal sinus rhythm on monitor
VS: BP 180/102, HR 85, RR 18, T 98.6
LABS: Glucose 110 mg/dL, Labs pending
EKG: EKG not done yet, but normal sinus rhythm on monitor
11) Gather more data:
CTH : No ICH, Dense MCA sign, ASPECT 6
CTA : High grade right Internal Carotid Artery stenosis and M1 segment MCA Occlusion
CTP : >160cc of salvageable brain tissue ( #Tmax >6seconds) and 40cc of core (Cerebral Blood Flow #CBF<30)

CTH : No ICH, Dense MCA sign, ASPECT 6
CTA : High grade right Internal Carotid Artery stenosis and M1 segment MCA Occlusion
CTP : >160cc of salvageable brain tissue ( #Tmax >6seconds) and 40cc of core (Cerebral Blood Flow #CBF<30)


12) Tandem occlusion, near complete occlusion of the ICA with a type 3 arch? Piece of 🍰, right?
Nope . . gulp . . . call the #neuroangio team in…..
Nope . . gulp . . . call the #neuroangio team in…..
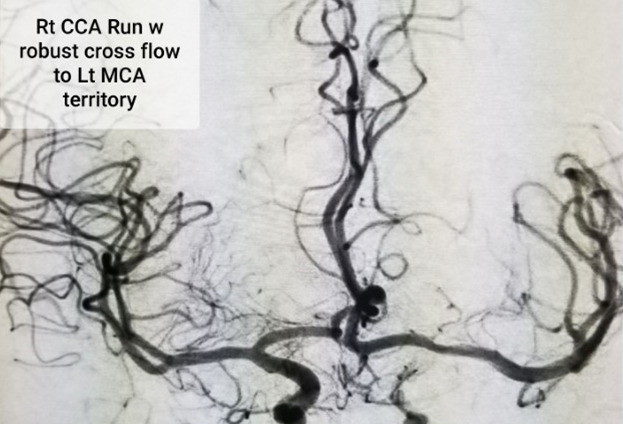
13) OK, warning: this is NOT a pretty picture. #DSA demonstrates near complete occlusion.
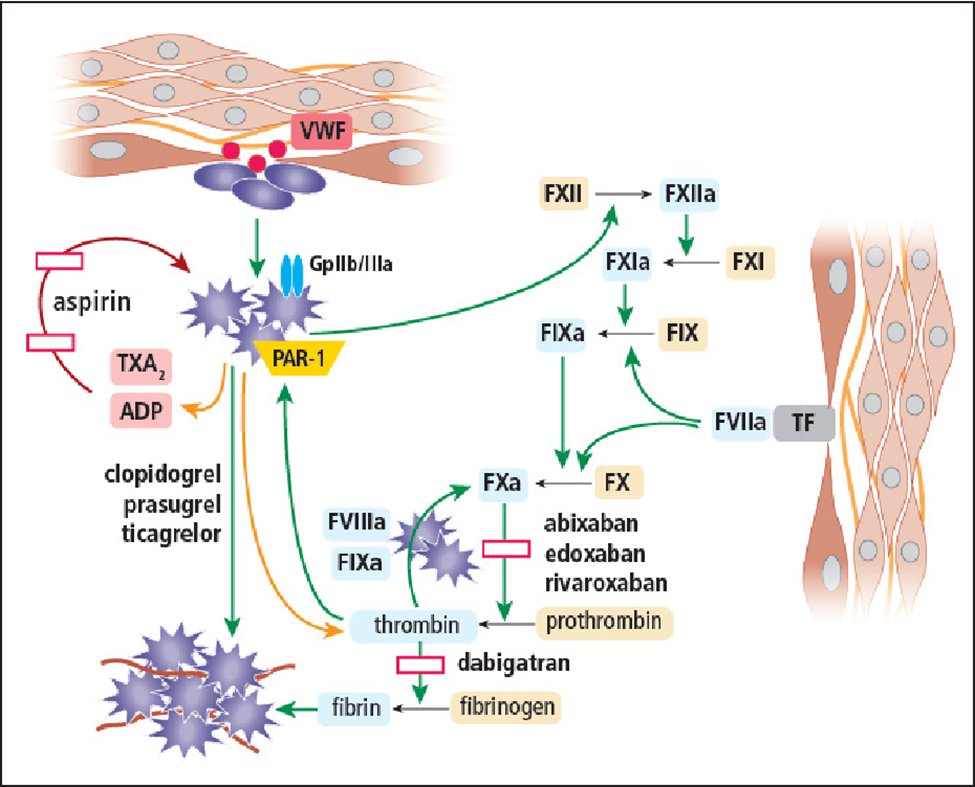
Left ICA is out at the origin with minimal collateral flow from the posterior circulation via a posterior communicator.
Left ICA is out at the origin with minimal collateral flow from the posterior circulation via a posterior communicator.

14) Not surprisingly, attempts to cross the high-grade ICA lesion were unsuccessful. So what do you do now?
a. Angioplasty & abort if unsuccessful
b. Dotter it (catheter-based angioplasty; see🔓ajnr.org/content/41/10/…) & abort if unsuccessful
c. Deploy a stent
d. Give up, go 2 🛏️
a. Angioplasty & abort if unsuccessful
b. Dotter it (catheter-based angioplasty; see🔓ajnr.org/content/41/10/…) & abort if unsuccessful
c. Deploy a stent
d. Give up, go 2 🛏️
15) So IRL, #angioplasty is performed, but attempts to cross the lesion following angioplasty were also unsuccessful ➡️decision made to perform acute stenting
You never give up!

You never give up!


16) Now, would you give #antiplatelets in preparation for emergent stenting?
a. Drop an OG tube & load oral DAPT
b. Load & initiate maintenance dose of IV antiplatelet therapy (#cangrelor, #tirofiban, #eptifibatide, or #abciximab)
c. forget the stent just start IV heparin drip
a. Drop an OG tube & load oral DAPT
b. Load & initiate maintenance dose of IV antiplatelet therapy (#cangrelor, #tirofiban, #eptifibatide, or #abciximab)
c. forget the stent just start IV heparin drip
17) Mark your best response & return TOMORROW for the correct answer, the resolution of this case & more education, & your link to🆓CE/#CME #physicians #physicianassociates #nurses #nursepractitioners #pharmacists! Hello @stephanamayer @AmuluruKrishna @neurocritical @AshuPJadhav
18) Welcome back! We are learning about IV #P2Y12i in neurovascular intervention from expert author @almuftifawaz. Did u answer the quiz in tweet 17? If not, scroll⤴️& COMMIT before moving onward!👏to @PascalJabbourMD @caseyalbin @WBrinjikji @AmeerEHassan @elghanemmoh @CamStroke
19) It’s B. #Antiplatelets are needed here.
20) Decision is made to go with IV #cangrelor:
- Potent, IV, #P2Y12i, a nonthienopyridine adenosine analog that does not require metabolic activation
- Onset w/in 2 minutes
- T1/2 3–6 min
- Platelet activity returns to normal within 60 min after discontinuation of the infusion
- Potent, IV, #P2Y12i, a nonthienopyridine adenosine analog that does not require metabolic activation
- Onset w/in 2 minutes
- T1/2 3–6 min
- Platelet activity returns to normal within 60 min after discontinuation of the infusion
22) Cangrelor is approved by @US_FDA as an adjunct therapy for patients undergoing #PCI. Use in #neuroendovascular procedures has been extrapolated from smaller trials. Cortez et al (pubmed.ncbi.nlm.nih.gov/33174182/) n=66 pts who underwent acute intervention & received cangrelor.
23) Pts were divided into 2 groups: ischemic (42) and aneurysm (24). Periprocedural thromboembolic events, hemorrhagic complications, & outcomes analyzed. Ischemic group periprocedural symptomatic complication rate was 9.5%, mortality was 2.4%. In the aneurysm group ....
24) ... 4.2% had a periprocedural complication during or after cangrelor infusion, & favorable clinical outcome was seen in 56.2% & 87.7% of ruptured and unruptured aneurysms, respectively, at discharge.
25) A meta-analysis by Marnat et al (ajnr.org/content/early/…) n=171 pts who received cangrelor as rescue strategy for refractory intracranial occlusion with or without intracranial rescue stent placement, & cervical carotid artery stent placement for cervical occlusion ...
26) ... (tandem occlusion or isolated cervical carotid occlusion). In all, symptomatic intracerebral hemorrhage occurred in 8.6% of pts & there was favorable outcome in 47.6% of patients. 90-day mortality was 22.6% & there was Day 1 artery patency in 89.7%.
27) The authors concluded that cangrelor offers promising safety and efficacy profiles, especially considering the complex endovascular reperfusion procedures in which it is usually applied.
We expect more studies.
We expect more studies.
28) Now that the stent is in, when do you load DAPT?
a. Immediately
b. 6h but obtain CTH confirming no hemorrhagic transformation (HT) prior to loading
c. 24h but obtain CTH confirming no HT prior to loading
d. continue cangrelor infusion til pt no longer at risk for HT (>72h)
a. Immediately
b. 6h but obtain CTH confirming no hemorrhagic transformation (HT) prior to loading
c. 24h but obtain CTH confirming no HT prior to loading
d. continue cangrelor infusion til pt no longer at risk for HT (>72h)
29) There are limited data, but best option is B, start #DAPT within 6h, after confirming no hemorrhagic transformation.
30) Following the endovascular thrombectomy of the M1 MCA occlusion, stenting is performed with TICI 3 recanalization. 



31) Check back here soon for an animation of what we did
32) Next, endovascular thrombectomy of the M1 MCA occlusion was performed with the same excellent result--TICI 3 recanalization 
33) Postprocedurally the IV regimen can be converted to an oral regimen within 24 hours. Coadministration of aspirin, an irreversible COX-1 inhibitor, & a #P2Y12i--best to use #ticagrelor after #cangrelor, is advised. See 🔓pubmed.ncbi.nlm.nih.gov/26444255/.
34) Remember that the multi-societal consensus document states that a P2Y12i should be continued for at least 30 days, and aspirin should be continued indefinitely. This has become the standard perioperative antiplatelet therapy. 🔓
pubmed.ncbi.nlm.nih.gov/21990803/
pubmed.ncbi.nlm.nih.gov/21990803/
35) Our patient--who started off with that frightening CT imaging--recovered in the ICU and then in the stroke unit. NIHSS was 4⃣on discharge to acute rehabilitation.
36) The take-home lesson: Cangrelor may be a feasible alternative for patients requiring immediate neurointervention w/ endoluminal devices. It also fosters secure transition to long-term ticagrelor & progression to surgery in the setting of unexpected complications.
37) #Glycoprotein IIb/IIIa receptor antagonists may be used in similar settings. There have been no head-to-head trials, and neither approach is on label per @US_FDA.
38) And you made it: 0.5h CE/#CME credits. Go to cardiometabolic-ce.com/plts13/ & grab your certificate! I am @almuftifawaz. Please FOLLOW @cardiomet_ce for cutting-edge accredited tweetorials! C'mon @AmuluruKrishna @elghanemmoh @SitaraKoneru @SharashidzeVera @gdawod1 @svinsociety
39) Kudos 👏🙏 to @SVINJournal @SVINRegistry @SVIN_MT2020 @SNISinfo @STateshimaMD @NguyenThanhMD @TudorGJovin @ShadiYaghi2 @LD_McCullough @SunilAShethMD @brainvesseldoc @AtherEnam @hadjiMDPhD @rosevmcd @HakeemShakirMD
40) Here's a link to the REMARKABLE video promised back ⤴️in tweet 31. All necessary patient consent obtained! Don't miss !
here it is: DON'T MISS IT!
• • •
Missing some Tweet in this thread? You can try to
force a refresh