Buckle up,
A thread is forming....
1/
Pelvic fractures - they’re HIGHLY vascularised bones surrounding super vascular tissues. Fractures = bad ?
Got it
Perfect
Moving on
There’s a few things to be concerned about.
0. Pain
1. Bleeding
2. Clotting (and disorders of clotting)
3. Nerves
4. Organs
5. Other stuff
How do I know if the patient had broken their pelvis?
Well. If they tell you they’ve broken their pelvis that’s usually a fairly reliable indicator.
Well, if both you and the patient aren’t sure; whilst they’re lying down, see if they can lift their own leg straight up.
3/
ncbi.nlm.nih.gov/m/pubmed/29132…
Why?
If either you or the patient THINK the pelvis is broken- treat it as if it is.
Either way touching (or worse: rocking) is a useless exam
don’t do it.
So
We think the pelvis is broken or the patient isn’t fully alert to tell us.
What do we do now?
Like a book.
An Open book if you will
Yeah im not going to lie to you it’s not amazing.
Frankly a lot of people with ploy trauma die so it’s difficult to test this well.
But we are pretty sure that pelvic binders contribute some benefit and minimal harms.
So please use them.
1. Take their clothes off.
Binder goes against skin! Always.
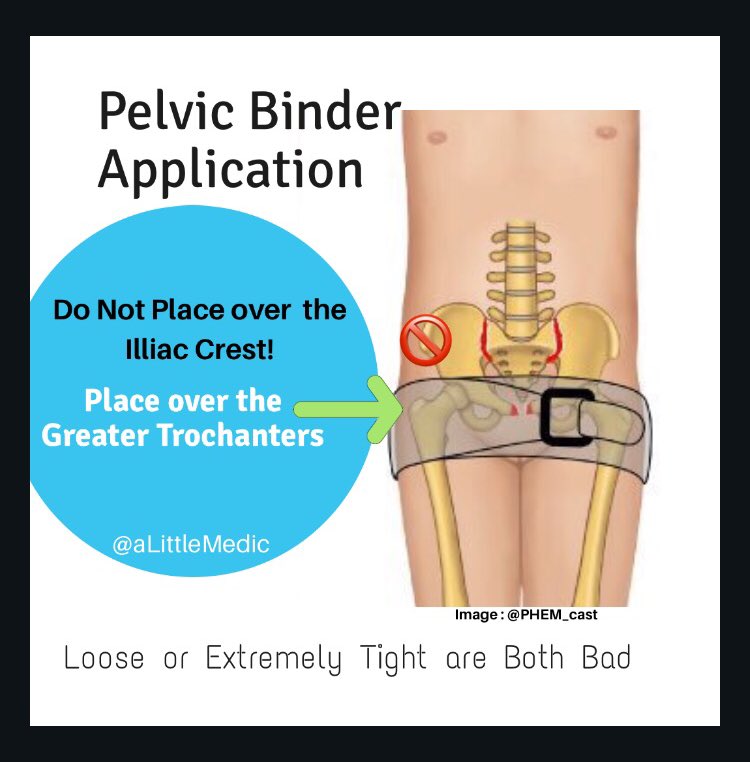
2. Apply it at the top of the legs, NOT the pointy part of the hips.
3. firm. Snug. Like you’re supporting a broken bone - not tight like mooring a boat or soft like applying a blanket.
Binder is on.
Wait.
Hang on a second.
HOW did we get it on?
Ok.
A few ways.
1. Use a SCOOP stretcher to get the patient off the ground and place them on a bed. Think ahead and have already laid the binder out underneath them on the bed. Put the patient on top and bind.
3. Log roll the patient like a normal trauma patient and smoosh all the broken bone fragments together in a painful, often unnecessary, and harmful manoeuvre.
The pelvis has been bound.
We’ve fixed their fracture right?
Not quite.
See, pelvic binders are good at some things but they aren’t a panacea.
What they do well:
✅ motion restriction = less pain
✅ reduce bony / venous bleeding
✅ lessen clot disruption
✅ visual warning
❌ total pelvic stabilisation
❌ arterial tamponade
❌ potent analgesia
❌ fix coagulopathy
That means we still need to do some things:
✳️ minimise movement as much as possible to reduce pain and clot disruption
✳️ provide multimodal analgesia (I’ll come to this further down)
✳️target coagulopathy (TXA, warmth, don’t dilute with massive crystalloid bolus)
They need a fully capable trauma centre.
A place with CT scanners, orthopaedic surgeons, AND interventional radiology - some pelvises need embolisation (radiologists plugs the holes) before, instead, or in combo with ortho.
The Local ER might not cut it 🤦🏻♀️
What are the options?
First up: opioids.
This is not the time to single handedly fix America’s opioid crisis. Be generous.
Adjuncts:
Ketamine (its twitter, can’t leave it out), IV paracetamol, Nitrous Oxide, NSAIDS are contentious.
And....
That’s right.
You can do a nerve block!
How?
Well, there’s two kinds of Fascia Illiaca Compartment Blocks*:
infra-inguinal and supra-Inguinal
(Below or above the inguinal ligament)
The traditional *FICB can be done blindly below the ligament ...
We really want to be hitting the obturator Nerve and as high up into the plexus as possible to block as much pelvic pain innervation as possible.
So, we really need to go above the ligament.
Now.
The patient might be sore on one side (good - do it on this side)
Or they might be sore on both sides (this makes things trickier)
Using ultrasound.
Above the inguinal ligament.
Remember that fascial plane Blocks are VOLUME blocks.
So use 40-50mls of dilute local anaesthetic.
Lidocaine is always a safe option.
If you wanna get fancy then ropivicaine is good.
Technically speaking you *could* do bilateral FICBs using reduced doses and dilute solutions, dual Fem Nerve blocks are done for elective procedures in some places.... but I’m not sure I’d be too keen to jump on that bandwagon just yet.
Trauma patients are at a HIGH (up to 1 in 3) risk of developing post traumatic stress reactions and persistent neuropathic pain syndromes.
Analgesia is crucial.
Let’s mention that pelvic fractures in the over 65yo age group can be more common, require less force, and be more subtle to detect
TL;DR
Pelvic Fractures:
✅Be suspicious
🆕Straight leg raise to rule out low risk patients
‼️Bind against skin, not hip pointy bits
🛑Minimise movement
🌀Give analgesia
☢️Take to IR & Surgery Capable facility
💔Target coagulopathy if needed
🚷Don’t stand them up!