A question: Which of the following is hypothesized to contribute to gout’s predilection for the first metatarsal phalangeal joint (MTP)?
OA = osteoarthritis
Before answering the original question, we need to review the mechanism of MSU crystal deposition in gout.
In order for crystals to deposit, you need:
*hyperuricemia
*nucleation (birth of new crystals)
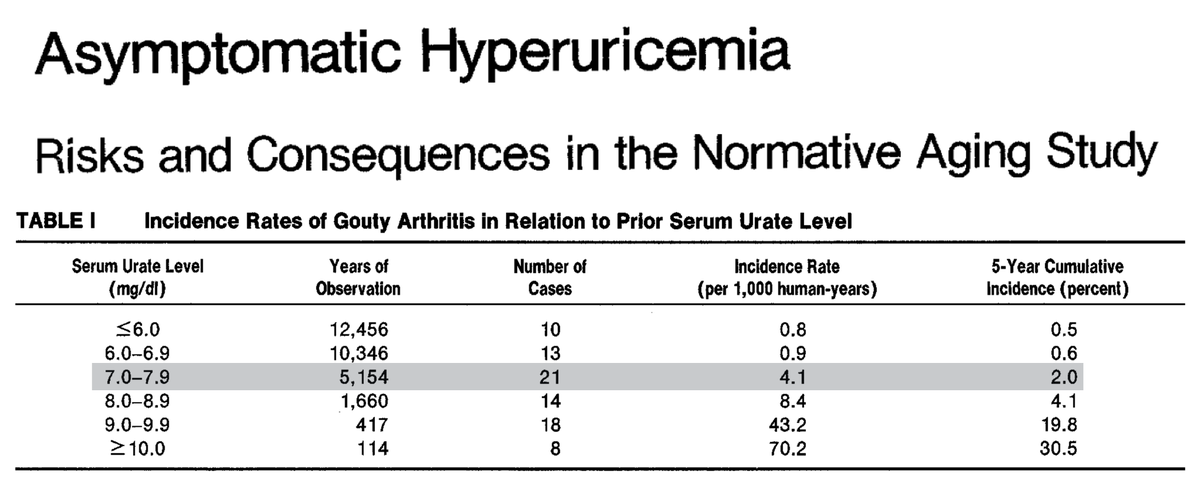
Regarding hyperuricemia, the solubility of MSU at 37ºC is about 7 mg/dL. Not surprisingly, the risk of gout increases above these levels.
ncbi.nlm.nih.gov/pubmed?term=38…
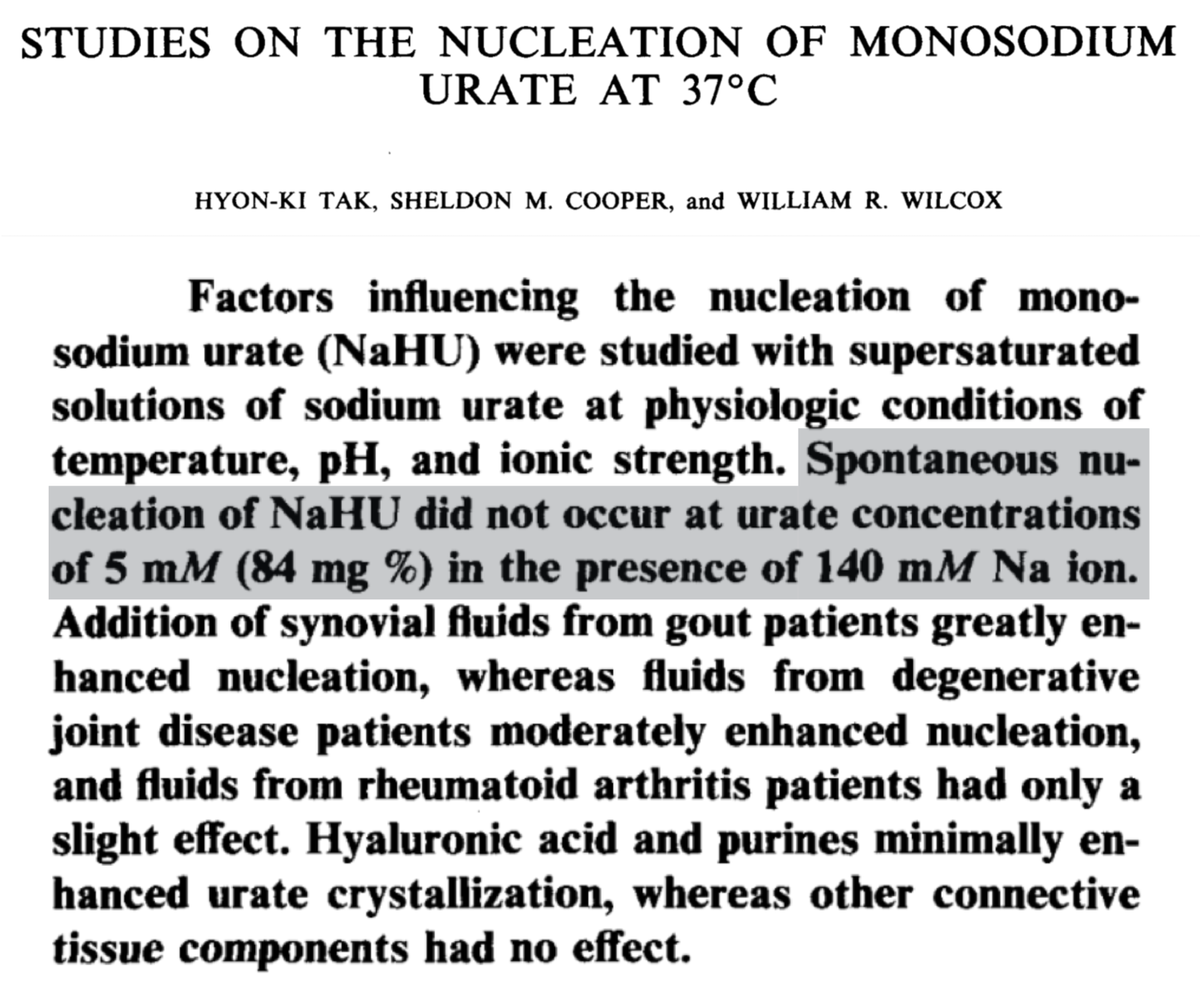
But, here's the thing: even at 84 mg/dL urate may remain soluble. Something must trigger MSU to leave solution and form crystals.
Put another way, something must trigger nucleation.
ncbi.nlm.nih.gov/pubmed?term=73…
So, our explanation for first MTP involvement in gout should ideally explain why this specific joint might be prone to:
*higher concentrations of MSU, or
*lower solubility of MSU at otherwise "normal" concentrations, and
*nucleation of MSU crystals
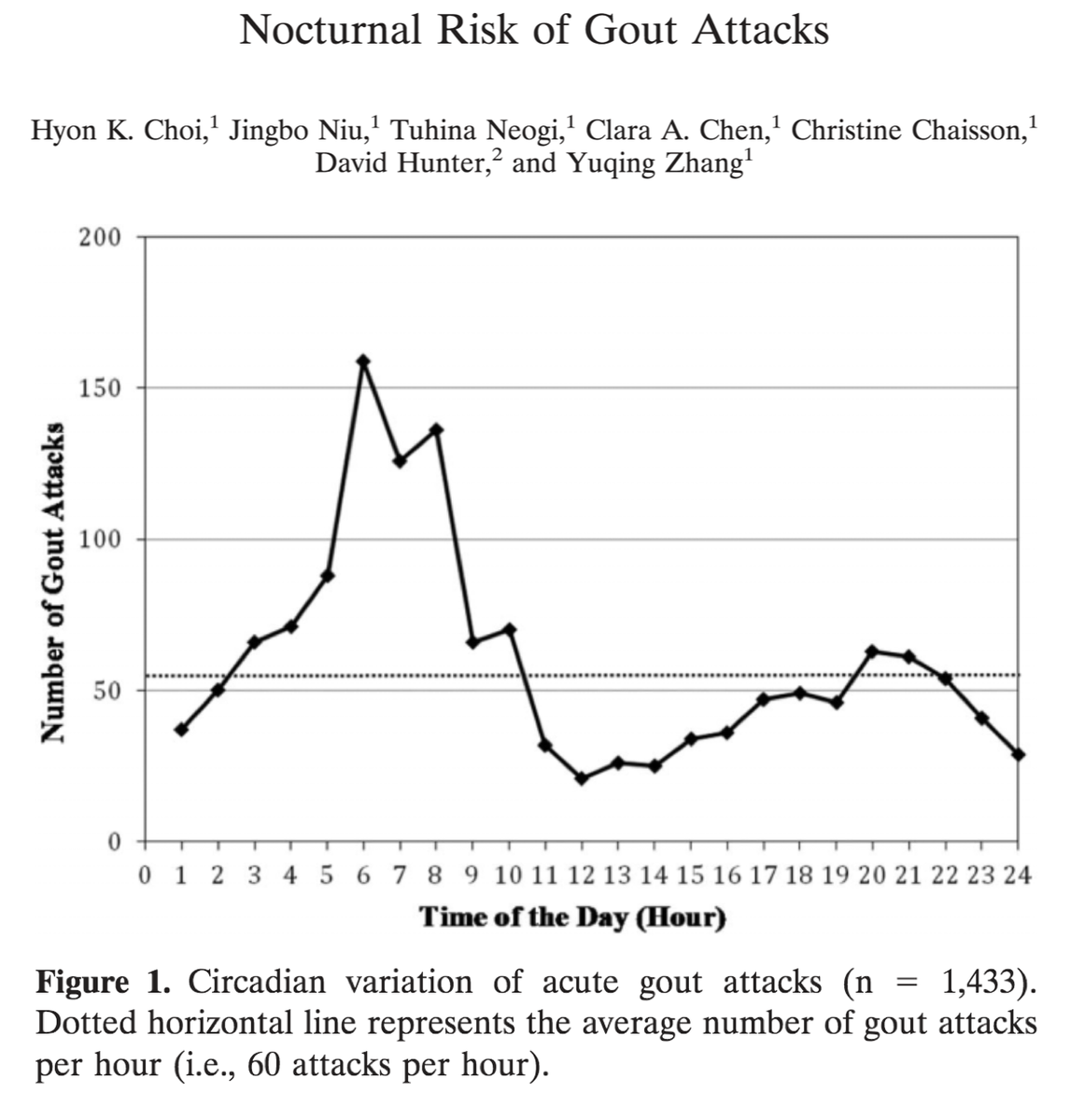
Forty years ago, Simkin proposed that trauma leads to synovial effusion in the first MTP. This effusion is resorbed overnight, leaving behind a higher concentration of MSU.
The result? Crystal formation and first MTP gout (also known as podagra)!
ncbi.nlm.nih.gov/pubmed/319726
This provides a partial explanation for why patients experience gout flares at night and may provide an answer regarding elevated MSU concentrations in a traumatized first MTP.
ncbi.nlm.nih.gov/pubmed/25504842
But there's more. Other characteristics of the first MTP include:
*low temperatures (my feet sure do get cold...)
*propensity for trauma (I stub my big toe all the time...)
*underlying OA (I'm 40, so I suspect I have this everywhere...)
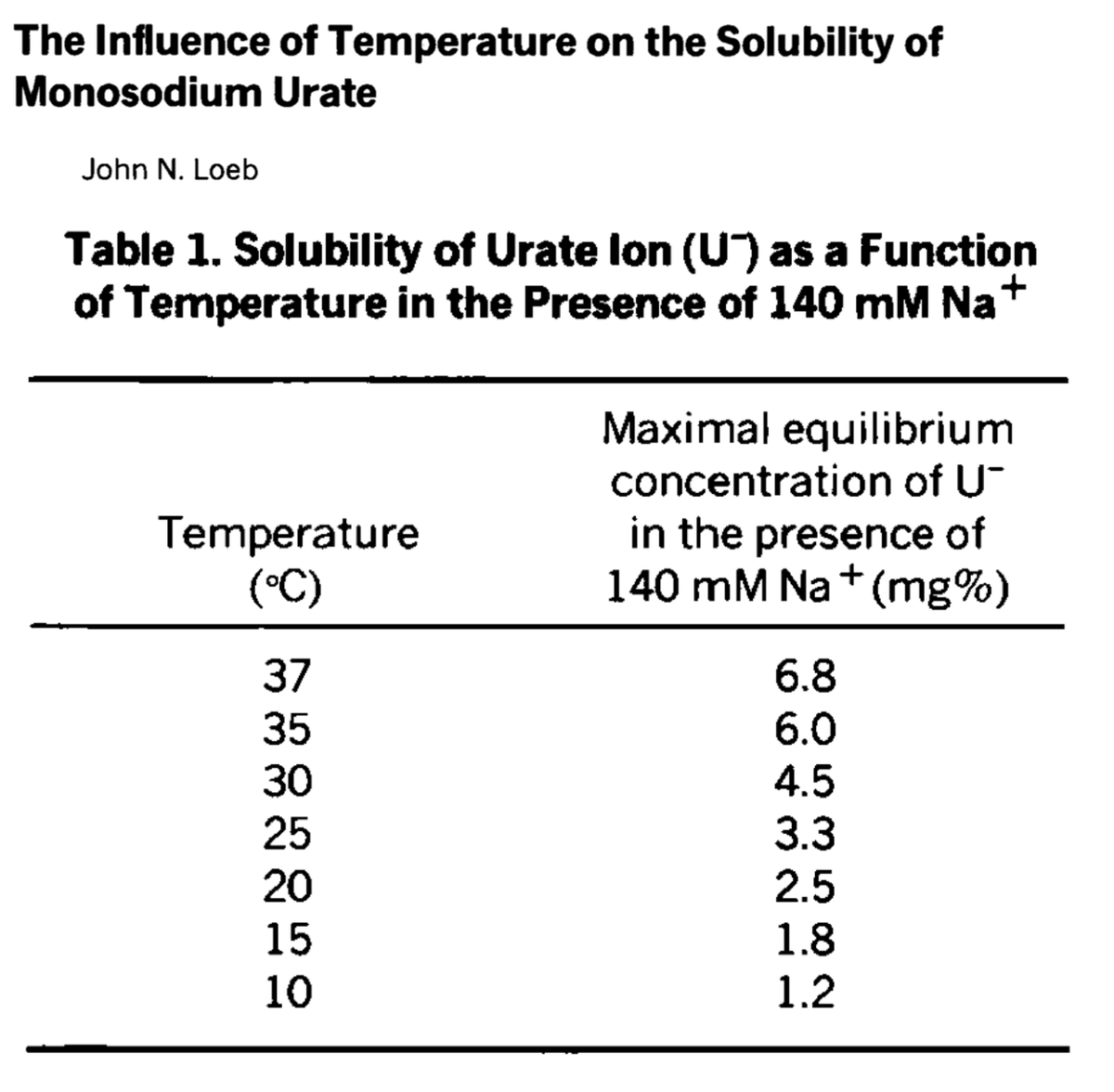
In 1972, Loeb showed that as the temperature decreases, the solubility of MSU also decreases. Loeb even wondered if the inflammatory response, by increasing the local temperature and therefore the solubility of MSU, helped to abate attacks.
ncbi.nlm.nih.gov/pubmed/5027604
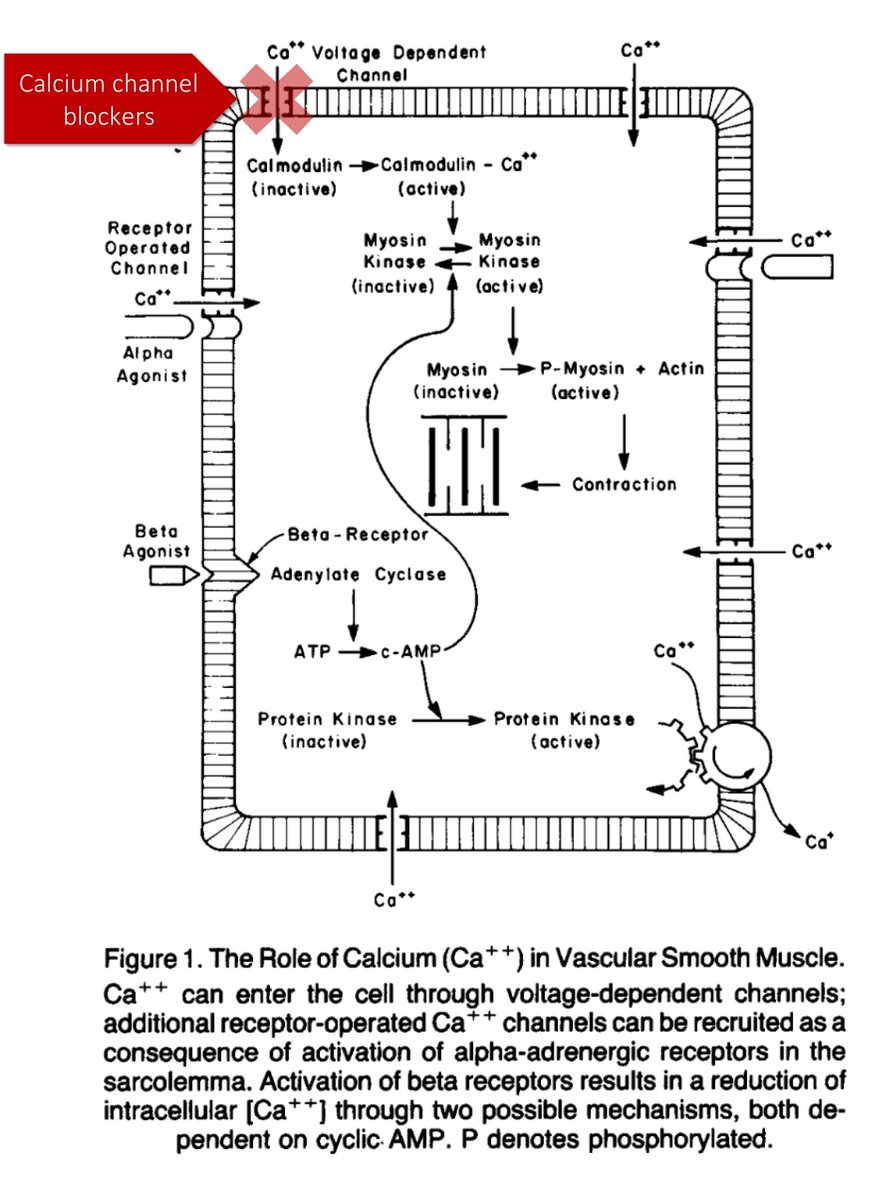
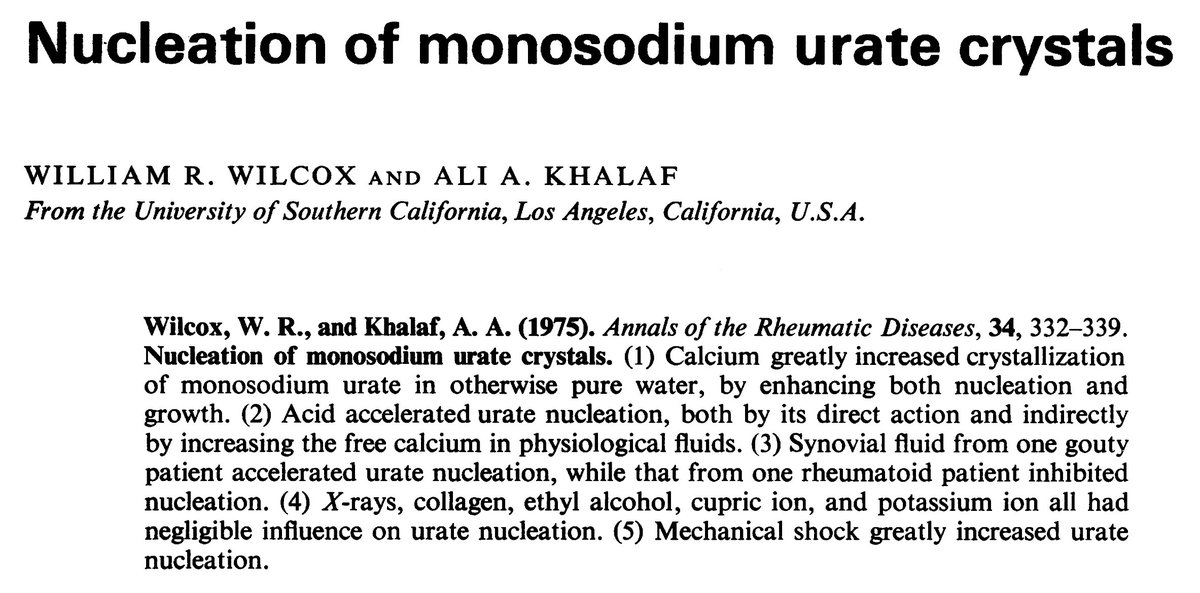
As for trauma, who hasn’t stubbed their big toe? This propensity for trauma may lead to a decrease in local pH and an increase in ionized calcium.
And calcium? It is a nidus for nucleation of MSU crystals.
ncbi.nlm.nih.gov/pubmed/242279
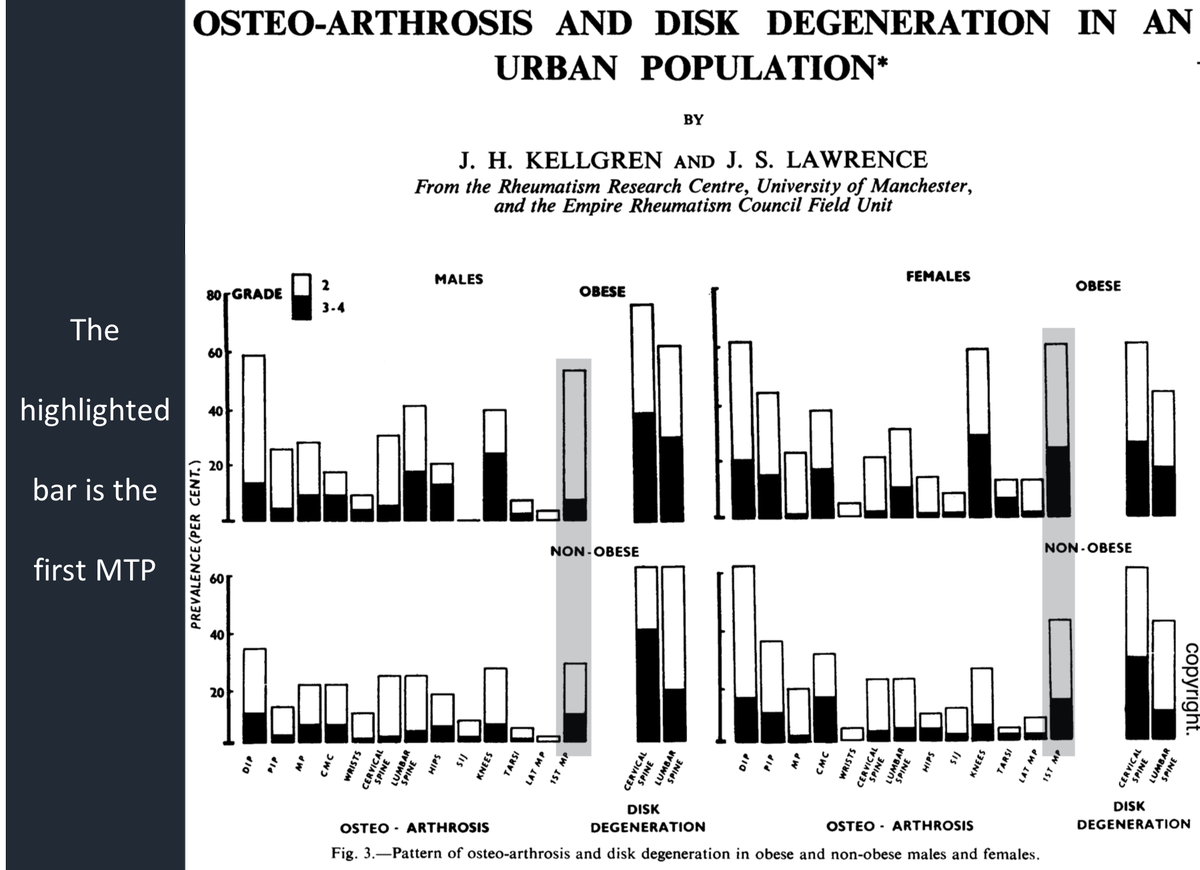
The final contributor may relate to osteoarthritis (OA).
So, what do you think... does OA affect the first MTP?
Does OA affect the first MTP?
It sure does. And, it appears to be one of the more commonly affected joints.
Given how active the first MTP is with each step, this didn't surprise me. I just hadn't thought of OA afflicting toes before.
ncbi.nlm.nih.gov/pubmed/13606727
If underlying OA increases the risk for gout, the exact mechanism is not clear. It may relate to synovial levels of chondroitin sulfate. This glycosaminoglycan may affect solubility and/or nucleation of MSU crystals.
ncbi.nlm.nih.gov/pubmed/27686950
Before giving my summation, here's the original question, posed once more:
Which of the following is hypothesized to contribute to gout’s predilection for the first metatarsal phalangeal joint (MTP)?
OA = osteoarthritis
To sum up, here are some reasons why the big toe may be particularly prone to gout:
*it's colder (lower solubility of MSU)
*we traumatize it (decreased pH and formation of effusion and nucleation)
*it's got underlying OA (possible effect on solubility and nucleation)