Not surprised 2hear that @AmyCEdmondson “stumbled into psychological safety while studying learning organizations.”
Perhaps that’s b/c psychosocial safety is a basic human need that must be satisfied to fully engage w/ learning
But there are numerous barriers to doing so, which are called intrapersonal risks. These risks keep us quiet and disengaged and drive impression management
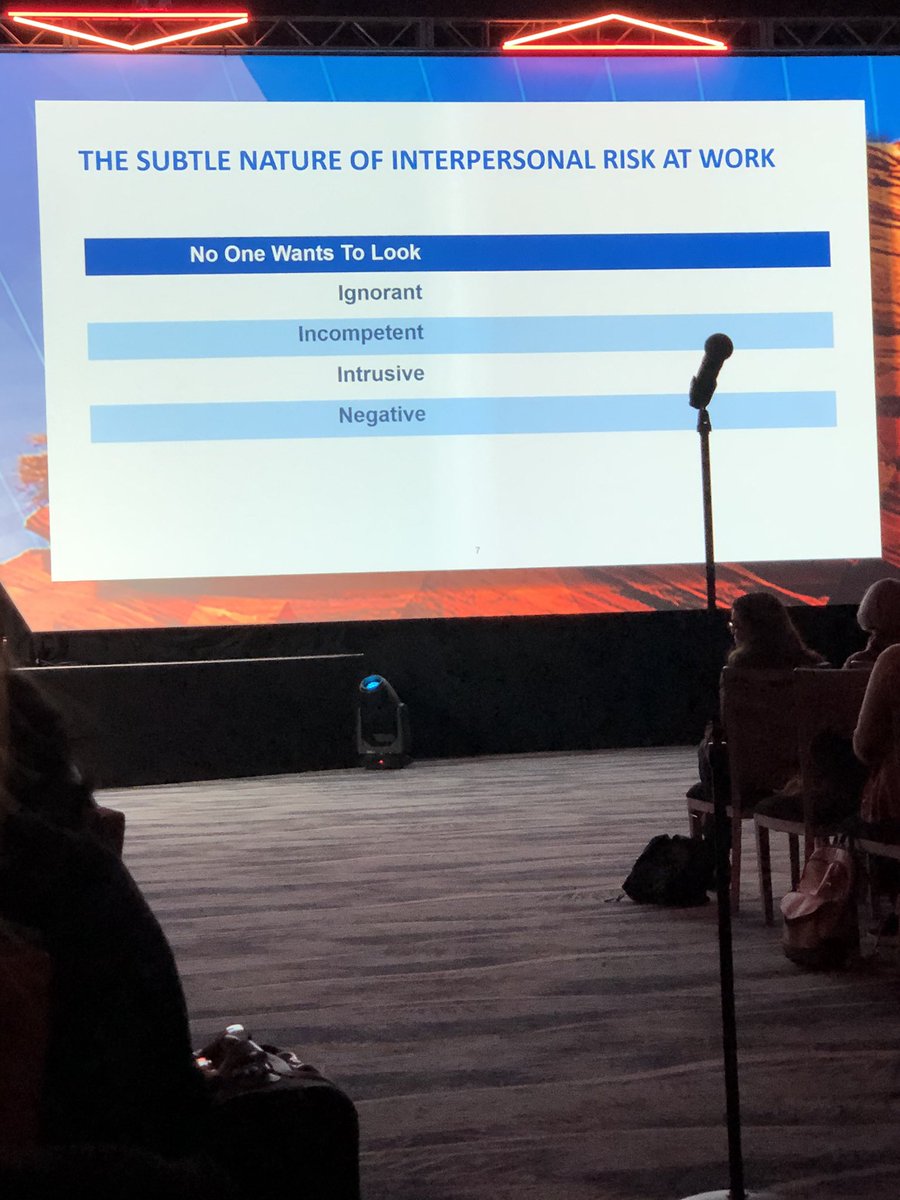
In medicine, why do we feel such pressure to protect our egos? B/c they are constantly under duress?
#aamc19
These intrapersonal risks are destructive in the effort to learn and innovate #aamc19
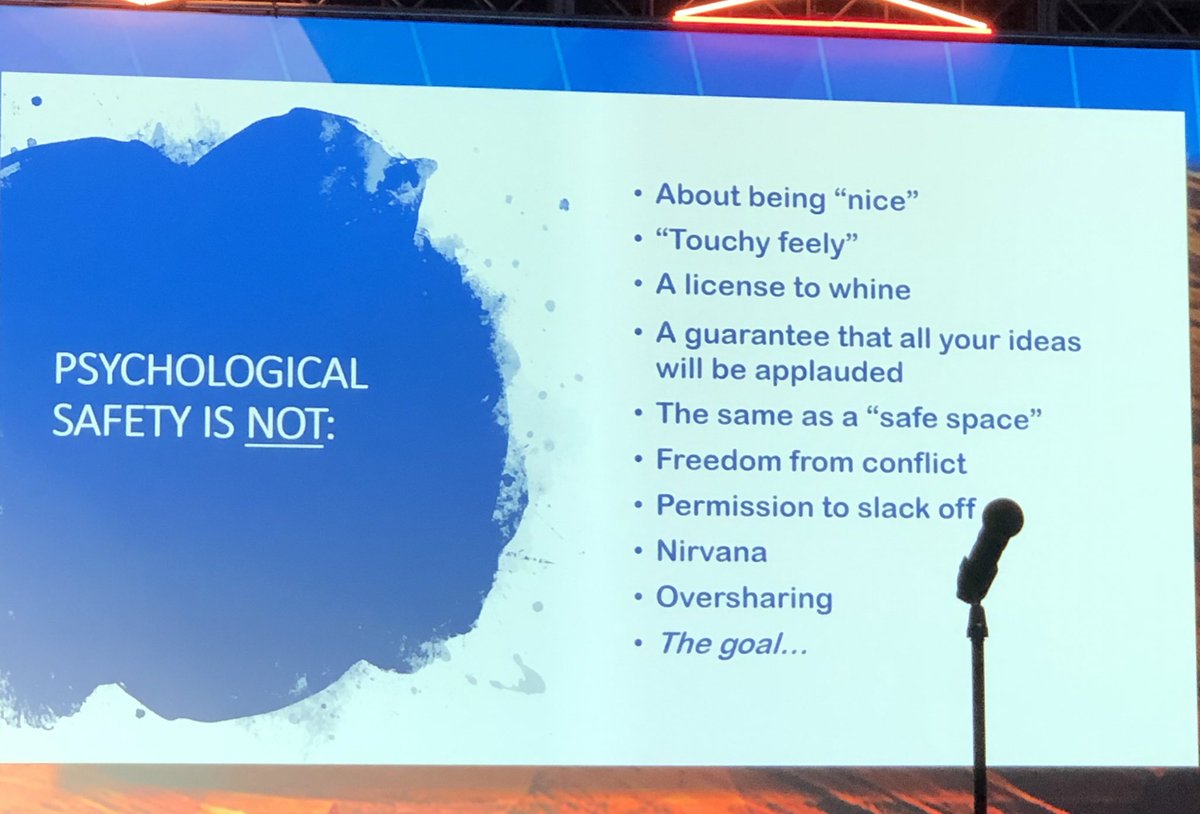
What it is NOT:
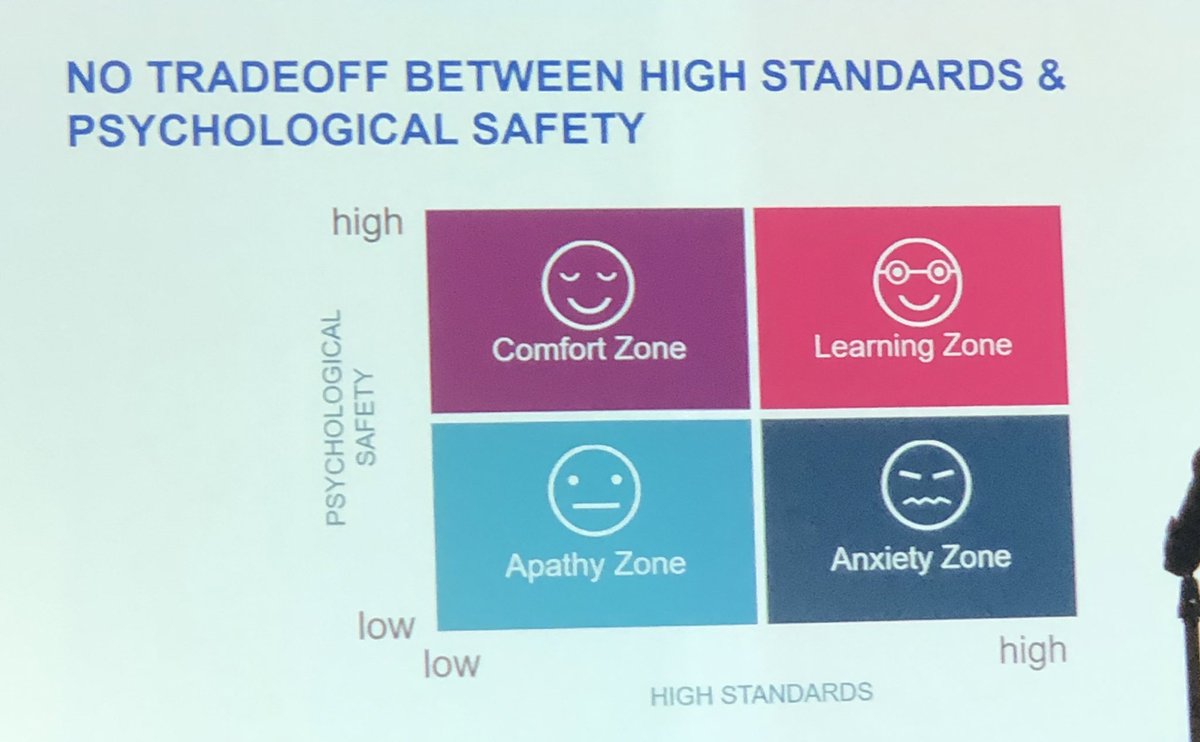
Thus, psychological safety is a specific tool through which we can push learners farther WITHOUT pushing them over the edge #aamc19 @AmyCEdmondson
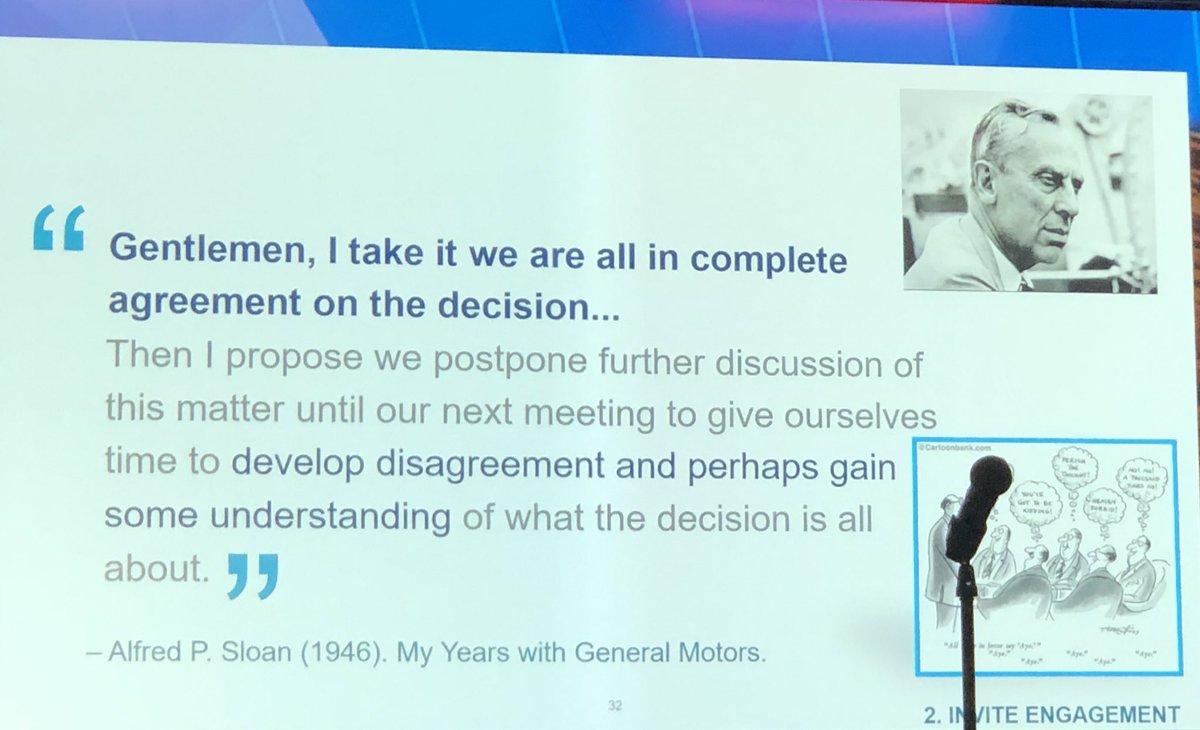
Brings up the notion of a “lowerarchy.” Can we drop the hierarchy in medicine when it isn’t absolutely needed? I’ve seen this work best within the military special operations community #AAMC19
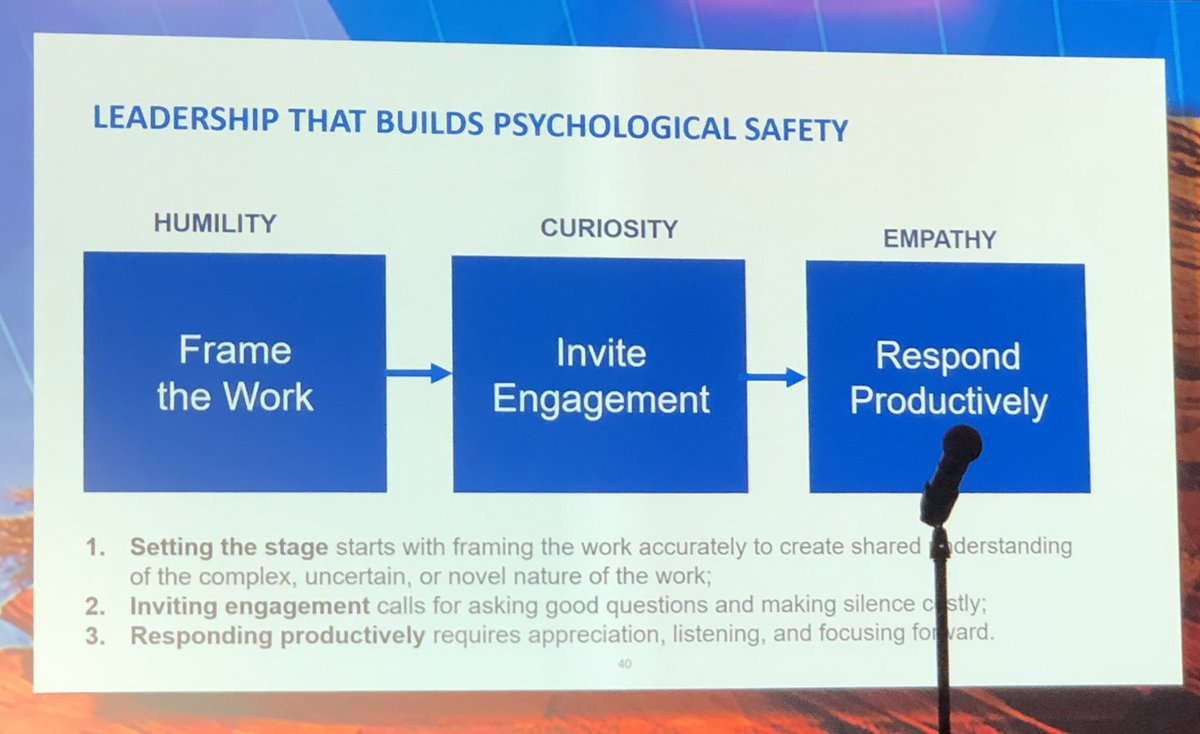
I take this 2mean that even in a toxic culture, mid-level leaders have⬆️ agency than we believe. Is it possible that local climate can overcome/change institutional culture? #AAMC19
What is the role of #shame in this paradigm? Our research suggests that high degrees of shame exist with low levels of psychological safety and high expectations #aamc19 @LaraVarpio
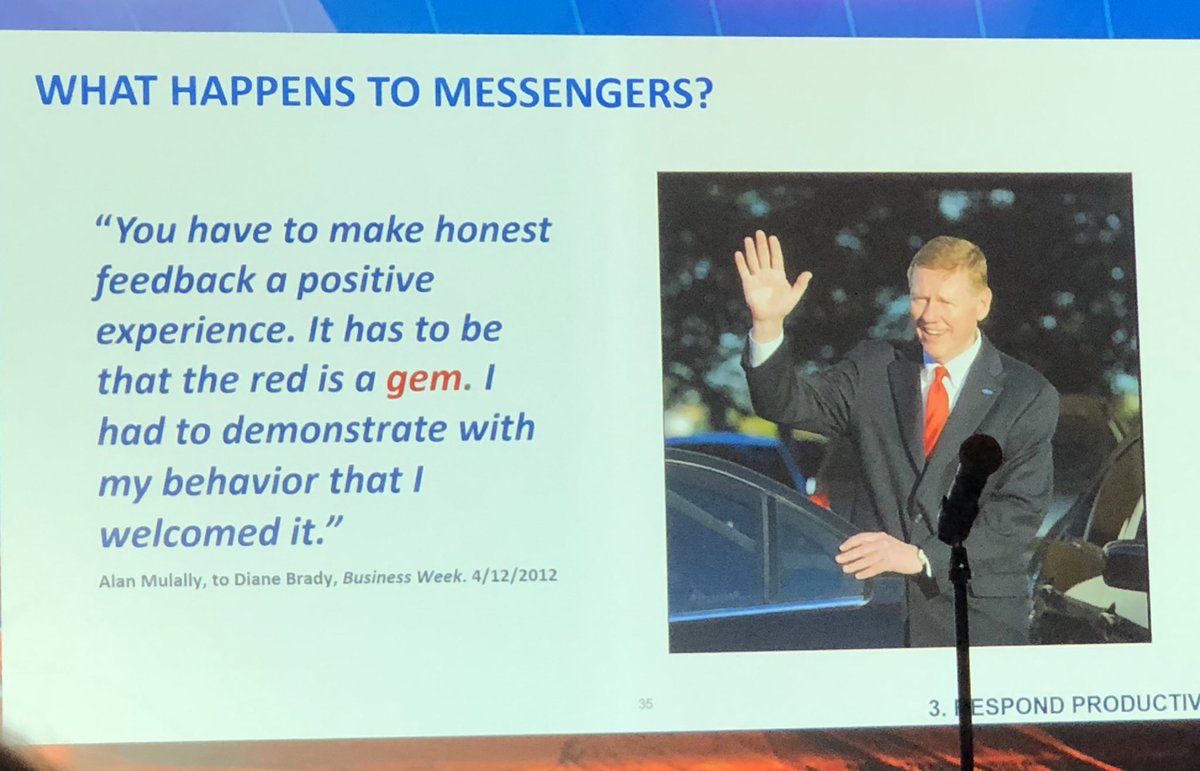
If speaking up in our environments requires heroism, we have a lot of work to do. What would patients think if they knew it takes valor & courage 2simply advocate on their behalf?#aamc19
One way to facilitate this is to actively manage the potential for shame in the feedback exchange #AAMC19 onlinelibrary.wiley.com/doi/10.1111/me…
Thank you @AmyCEdmondson and @AAMCtoday for bringing this critical topic of #psychologicalsafety to #meded
[end]