Why does E. coli clear from the blood faster than S. aureus?
I've heard this repeatedly but never fully understood the difference.
One answer helps explain why cirrhosis is a risk factor for infection and introduced me to a Trojan horse of the immune system.
Read on!
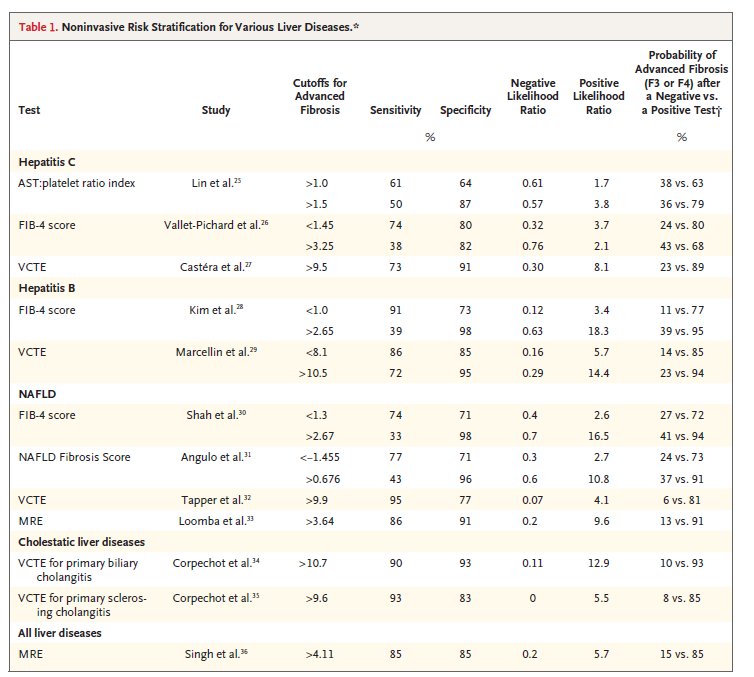
Let's start with some data showing that there IS a difference in how well E. coli and S. aureus are cleared from the blood.
The SCRIBE study reported the following rates of persistent bacteremia:
🔹E. Coli 7%
🔹S. aureus: 33%
ncbi.nlm.nih.gov/pubmed/27296858
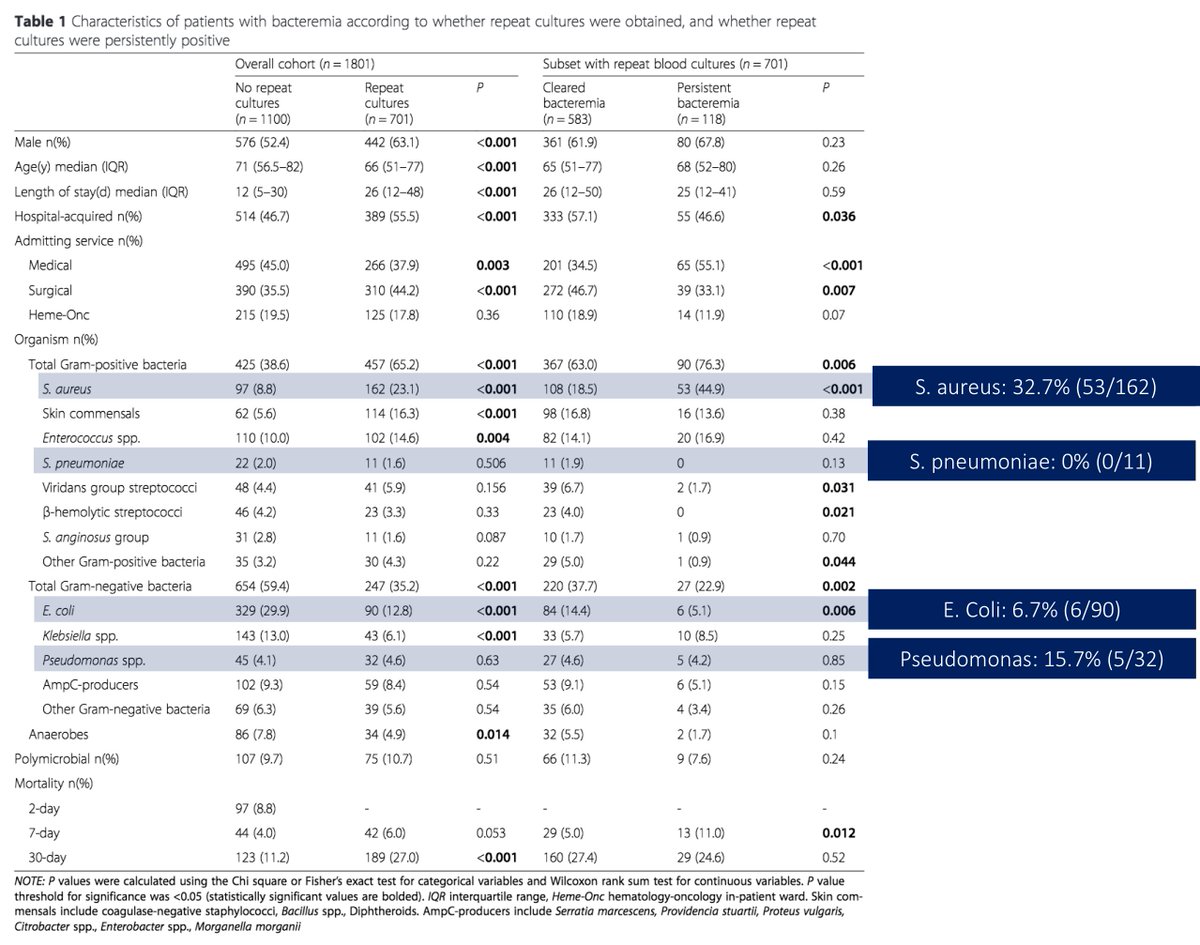
To understand this difference, we need to explore WHERE bacteria are cleared from the blood.
One of the first sites is the reticuloendothelial system (aka the mononuculear phagocyte system or MPS).
🔹One key organ of the MPS: liver
🔹One key cell in the liver: Kupffer cell
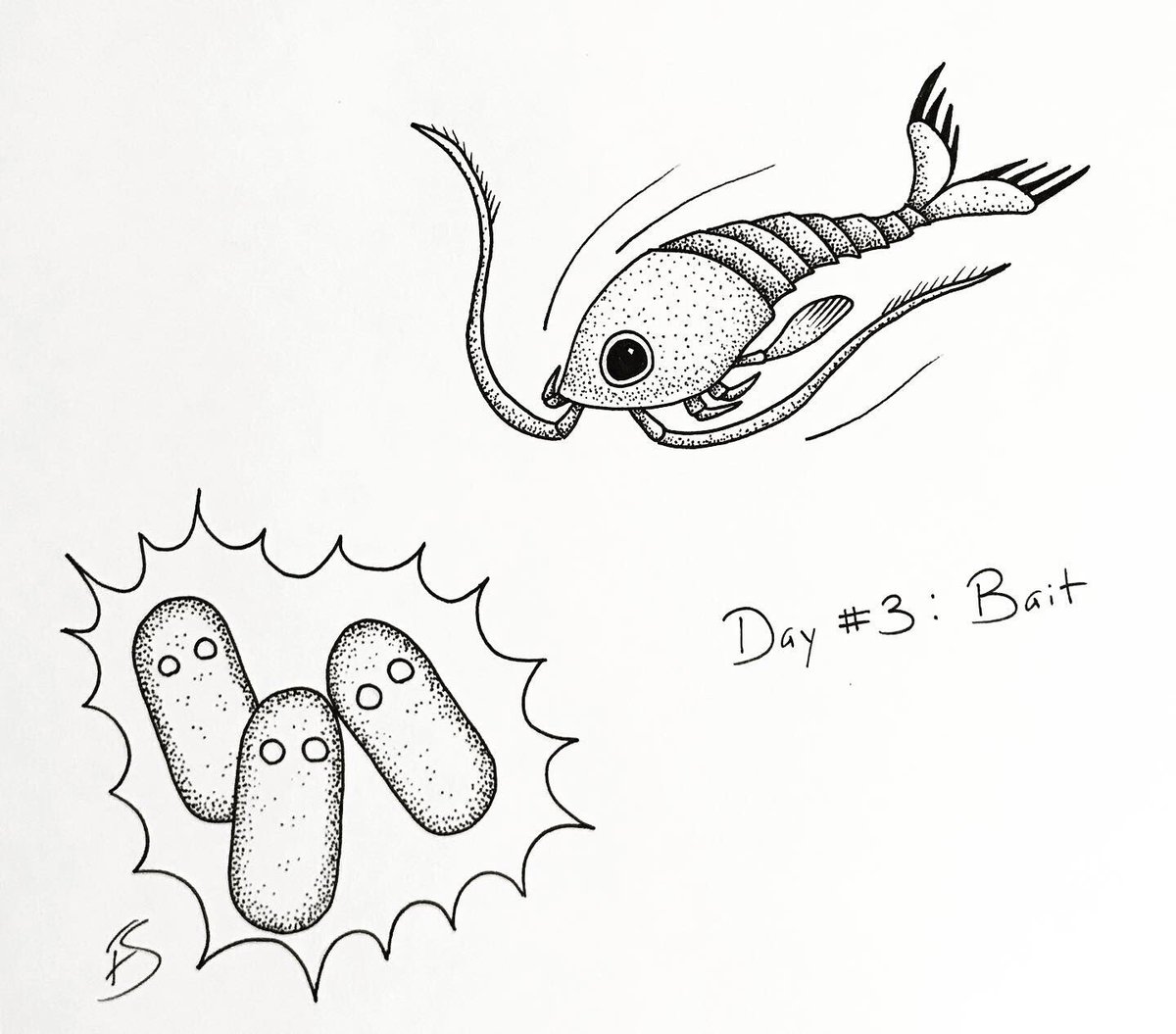
Kupffer cells (KC) phagocytose bacteria as they enter the sinusoids of the liver.
In fact, some have described the liver as a "firewall" against bloodstream bacteria (KC make up >50% of the cells in the MPS).
ncbi.nlm.nih.gov/pubmed/24848256
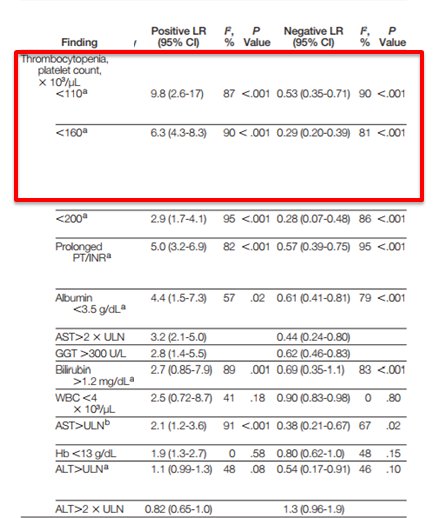
An understanding of the role of the MPS (and KC within the liver, more specifically) sheds light on a fact we all know:
💥Cirrhosis is a risk factor for infection💥
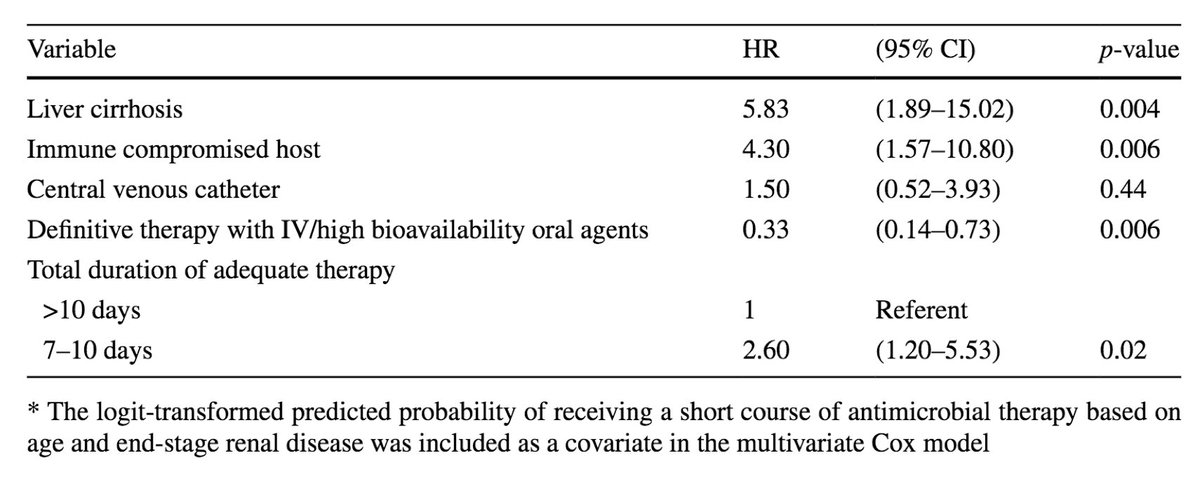
Cirrhosis was associated with a HR of 5.8 for treatment failure after GNR bacteremia.
ncbi.nlm.nih.gov/pubmed/28478600
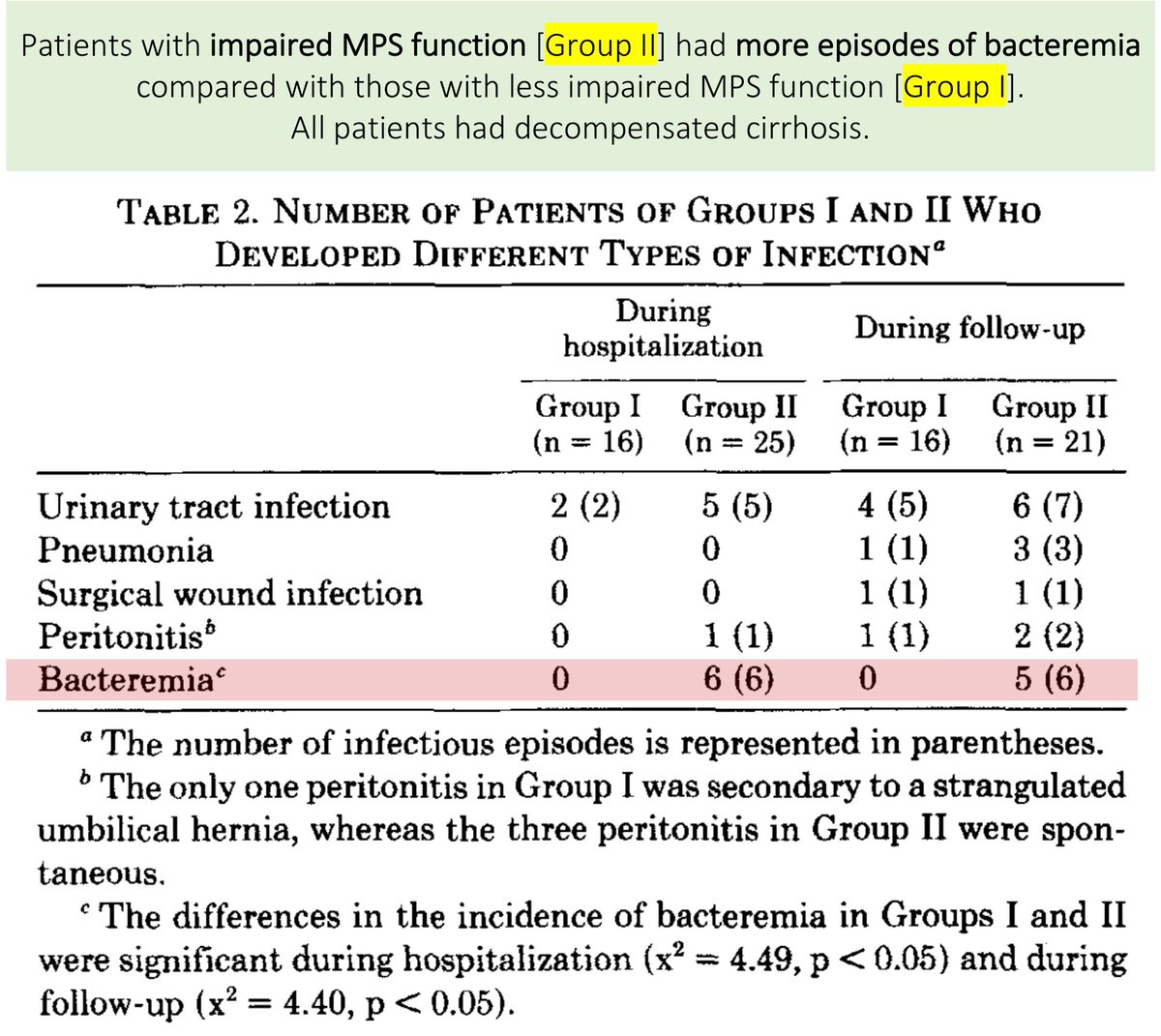
Though the infection risk ascribed to cirrhosis is multifactorial, the role of MPS dysfunction seems clear.
In one study of 41 patients with cirrhosis, it was those with reduced MPS function had an increased risk of bacteremia.
Kupffer cells matter!
ncbi.nlm.nih.gov/pubmed/6693068
Key point #1
🔑The mononuclear phagocyte system (MPS) is important for the clearance of bacteria from the blood.
This leads to a POLL question.
Which bacteria do you suspect is cleared more rapidly by the MPS?
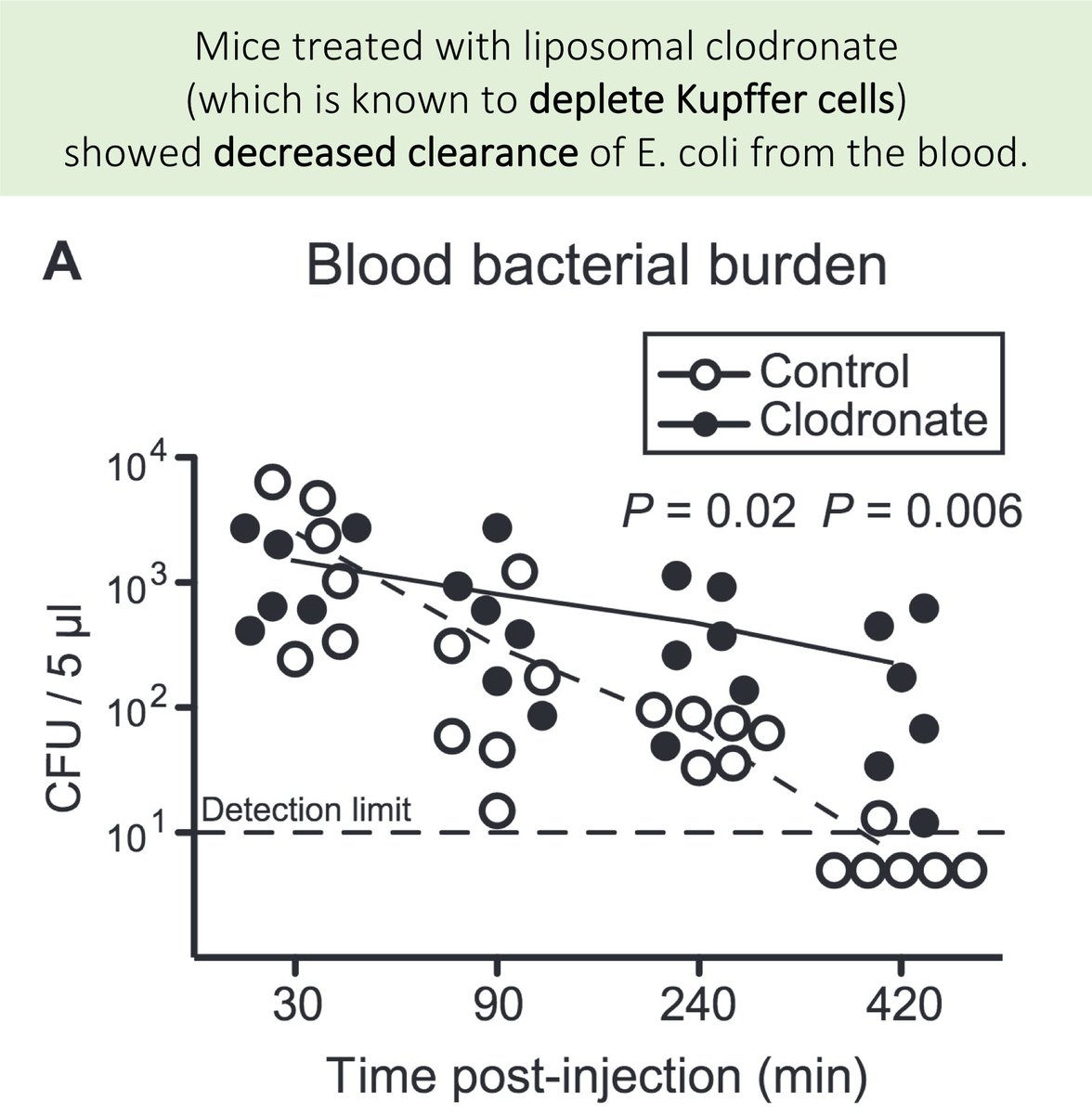
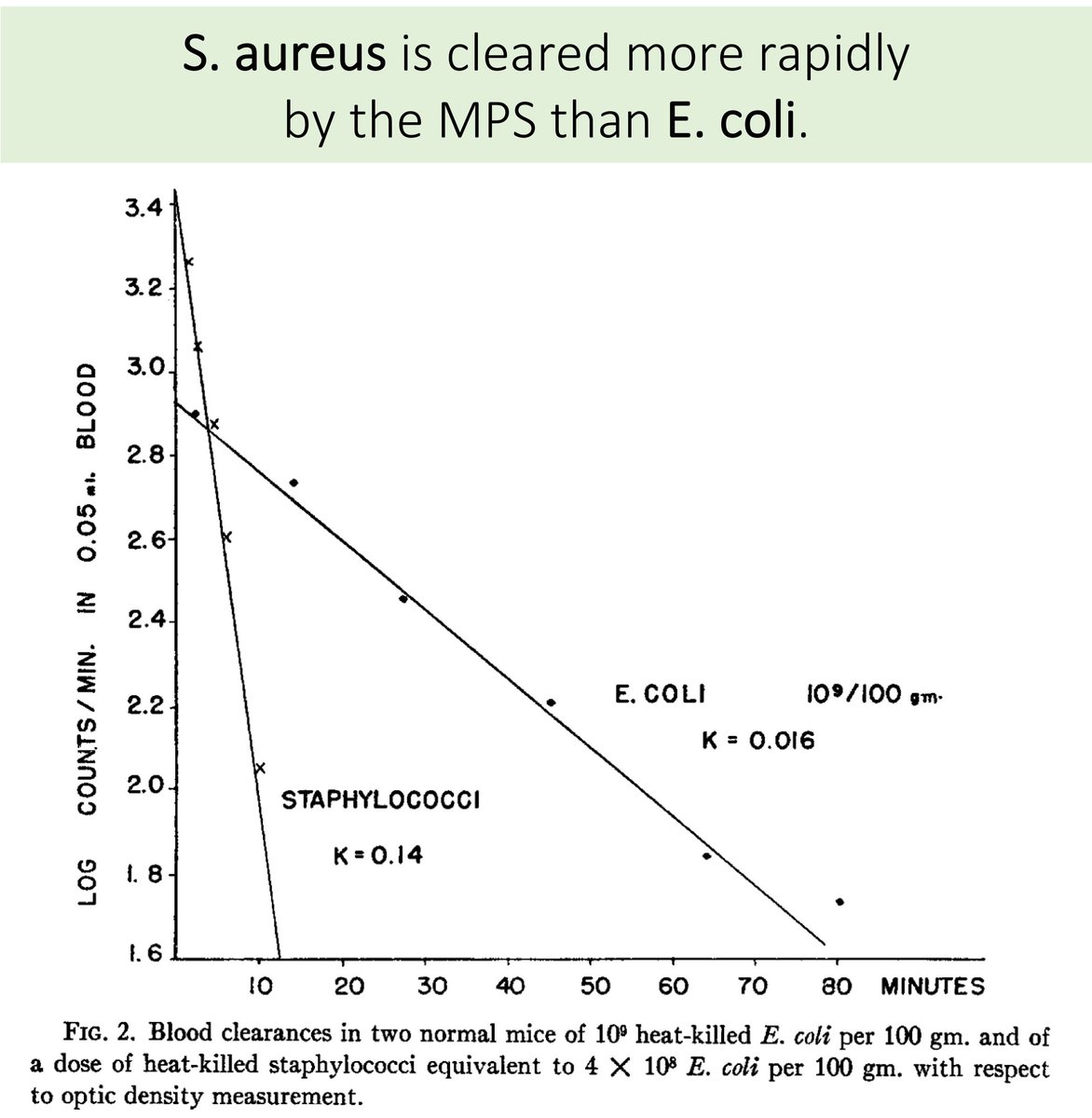
It turns out that MPS clearance may be FASTER with S. aureus.
This is NOT what I expected to find when I began reading about this topic.
ncbi.nlm.nih.gov/pubmed/13664867
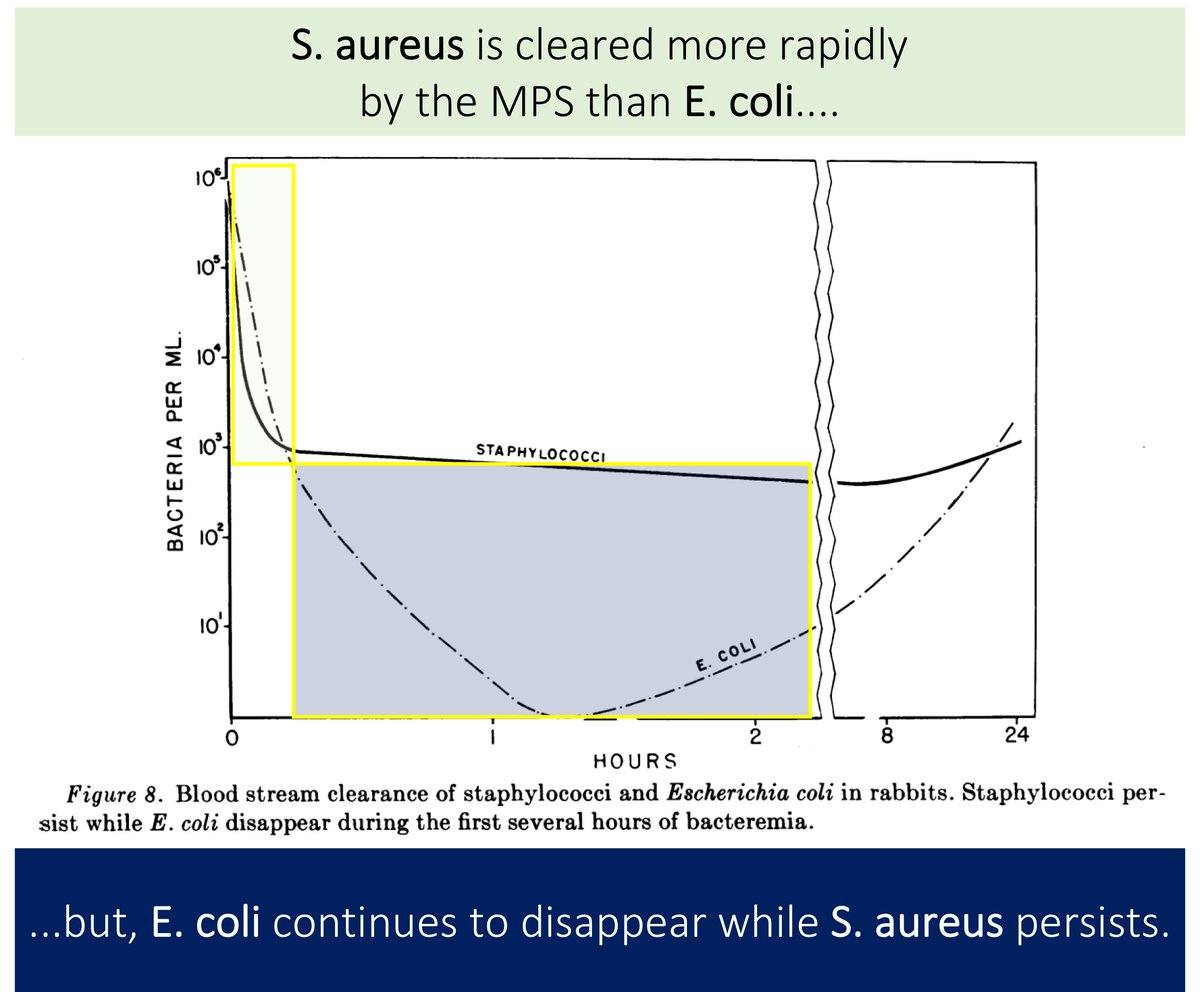
These results (i.e., that S. aureus is cleared by the MPS more quickly than E. coli) run counter to what I have understood.
Another study demonstrates that although S. aureus counts drop more quickly, it levels off.
Clearance of E. coli continues.
ncbi.nlm.nih.gov/pubmed/14438353
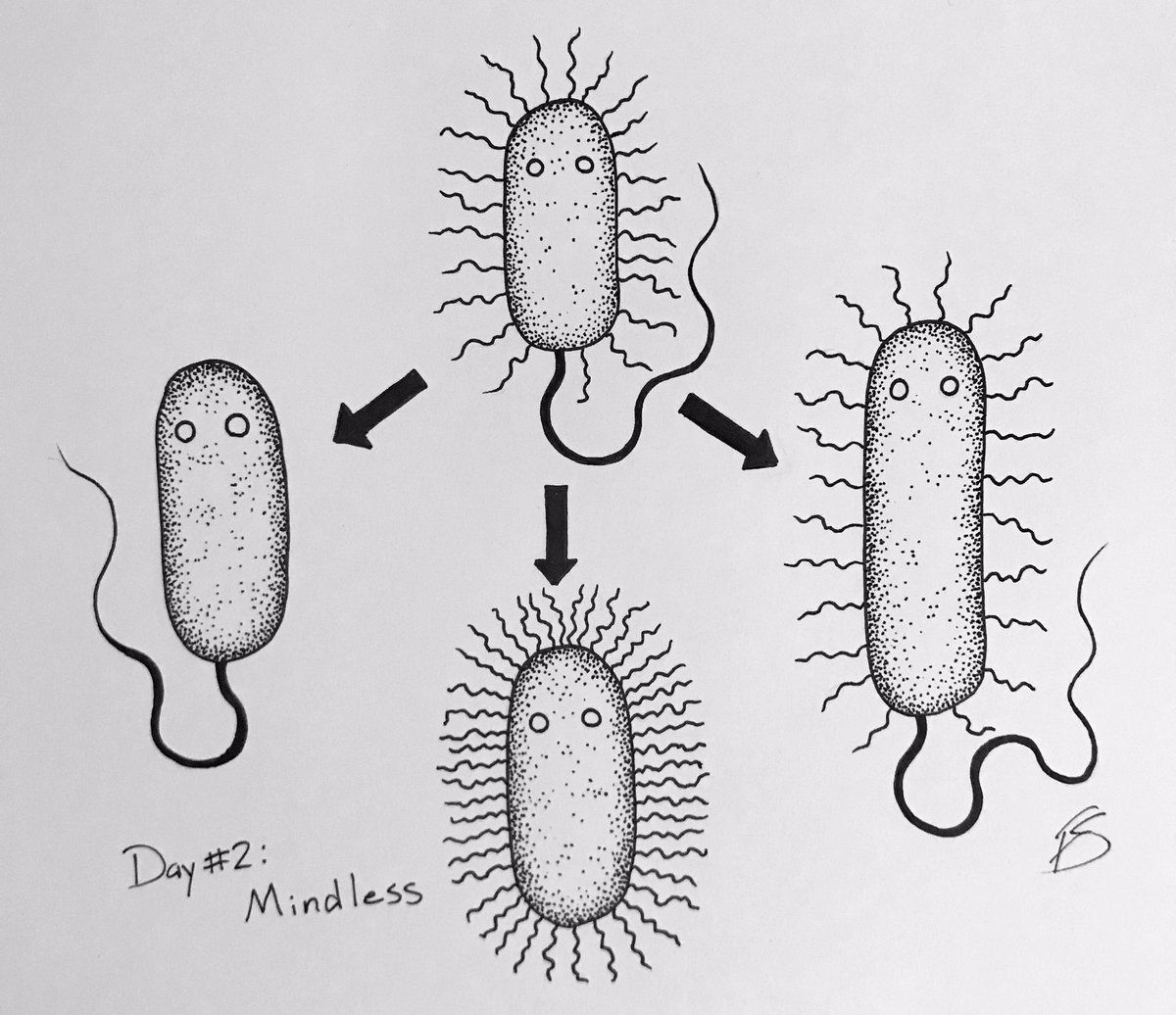
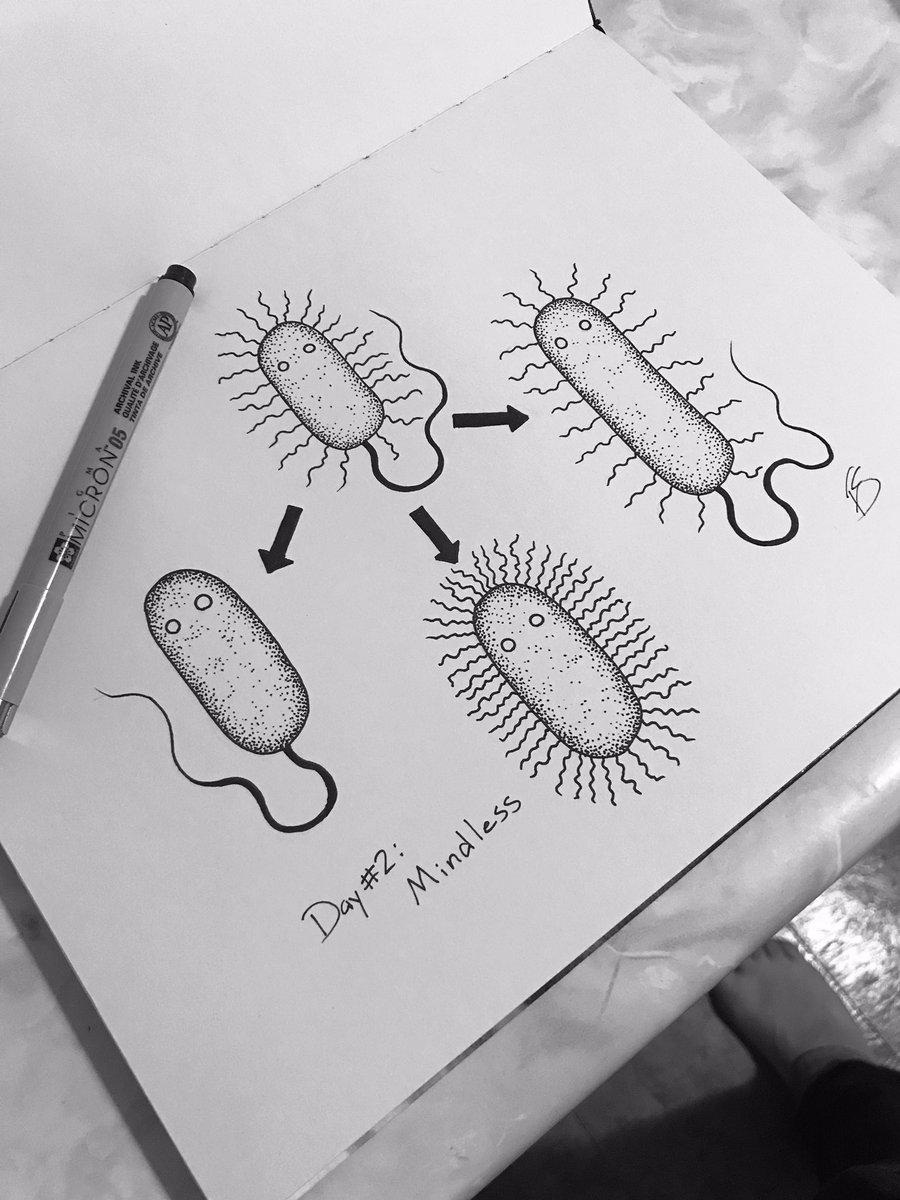
One proposed explanation for late/persistent bacteremia: S. aureus hides inside neutrophils.
Evidence for S. aureus survival within neutrophils has been around for decades. In 1952, Rogers and Tompsett observed viable bacteria in the cytoplasm.
ncbi.nlm.nih.gov/pubmed/14907971
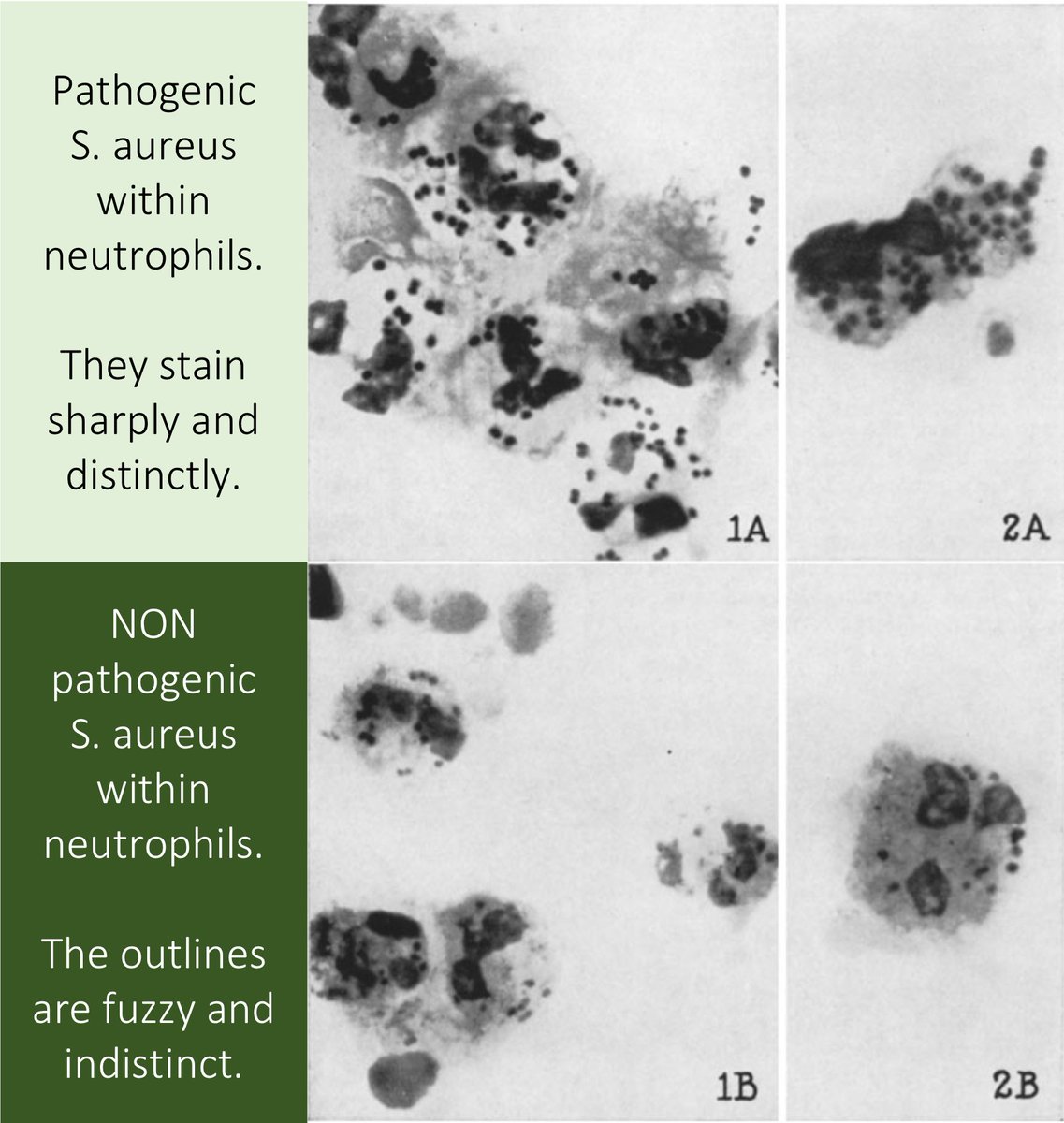
There are contemporary data suggesting that neutrophils act as Trojan horses for S. aureus.
One prospective study of adults with cancer found LOWER rates of S. aureus bacteremia in those who were NEUTROPENIC:
🔹Neutropenic: 12%
🔹Not neutropenic: 35%
ncbi.nlm.nih.gov/pubmed/16424972
Key points #2-3
🔑It appears that the MPS deals with S. aureus and E. coli in slightly different ways.
🔑Neutrophils may harbor viable S. aureus, allowing for their re-emergence in the blood.
There are undoubtedly other factors at play.
Differences in...
🔹Organisms (e.g., S. aureus is more likely to create metastatic foci)
🔹Treatments (i.e., antibiotic efficacy varies for E. coli and S. aureus)
🔹Immune response (e.g., there are variable cytokine responses)
🔑The MPS is important for the clearance of bacteria from the blood.
🔑It appears that the MPS deals with S. aureus and E. coli in slightly different ways.
🔑Neutrophils may harbor viable S. aureus, allowing for their re-emergence in the blood.