1/ 🎥 Asymptomatic #COVID = Silent Spreaders
This short video from @EricTopol & @Danieloran summarizes key issues about Asymptomatic Spread of #COVID19. Watch & then read the🧵for my unpacking…there is so much at stake!
#Pandemic #Vaccinate
This short video from @EricTopol & @Danieloran summarizes key issues about Asymptomatic Spread of #COVID19. Watch & then read the🧵for my unpacking…there is so much at stake!
#Pandemic #Vaccinate
2/ In 2020, @danieloran & @EricTopol predicted that up to 40-45% of people infected w #COVID19 were totally asymptomatic, meaning HUGE risk of silently spreading the disease to others. 👁 highlights
Next tweet for the UPDATE...
bit.ly/3yz1QNN
#MedTwitter #NurseTwitter
Next tweet for the UPDATE...
bit.ly/3yz1QNN
#MedTwitter #NurseTwitter
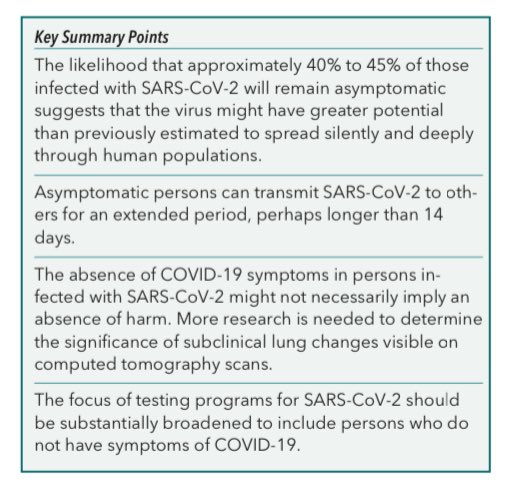
3/ Now we know ~1 in 3 people infected with #SARSCoV2 remain asymptomatic. This is based on 61 studies & ~1,800,000 pts! Also, of those who test + w/out any symptoms, 75% stay asymptomatic. This poses a HUGE risk of silent spread to high risk patients.
bit.ly/2SiXQAn
bit.ly/2SiXQAn

4/ This @Lancet study found that asymptomatic #COVID-infected people are ~1/4 as infectious as people w symptoms (& other studies show about 1/3rd), so that is good, but there are absolutely people w/out symptoms giving covid to susceptible people.
bit.ly/3ukYM4M
bit.ly/3ukYM4M
5/ In an indoor space, you can bet there are #unVaxxed people around you w asymptomatic #COVID. If you ARE Vaxxed, you are NOT at risk for mod/severe disease, and that’s great, but YOU CAN GET INFECTED & give it to someone else without knowing it, which is where masks help.
6/ Today I was talking with a patient who declined the #Vaccine and is suffering severe blood clots and lung failure from COVID and she begged me to ask others to not make the same mistake she made…
7/fin
In order to ⬇️ asymptomatic spread, we must develop & use rapid, inexpensive home testing often as discussed by @michaelmina_lab. Financial assistance to under-resourced populations must happen. For now, #Vaccine + #Mask for indoor public spaces are still 🔑 considerations.
In order to ⬇️ asymptomatic spread, we must develop & use rapid, inexpensive home testing often as discussed by @michaelmina_lab. Financial assistance to under-resourced populations must happen. For now, #Vaccine + #Mask for indoor public spaces are still 🔑 considerations.
BTW, the source of the video on tweet #1 of this thread was this new @AnnalsofIM paper by @danieloran & @EricTopol
bit.ly/2SiXQAn
bit.ly/2SiXQAn
• • •
Missing some Tweet in this thread? You can try to
force a refresh