1/🧵 Lung Scarring in #COVID19 – what’s the deal?
I got a birds eye view of #LongCOVID yesterday from my patient who’s still on Oxygen at 8 months. WHY?
Let’s unpack what happens in the 🫁 and why it’s such a life-changing disease is for so many...
#MedTwitter #NurseTwitter
I got a birds eye view of #LongCOVID yesterday from my patient who’s still on Oxygen at 8 months. WHY?
Let’s unpack what happens in the 🫁 and why it’s such a life-changing disease is for so many...
#MedTwitter #NurseTwitter
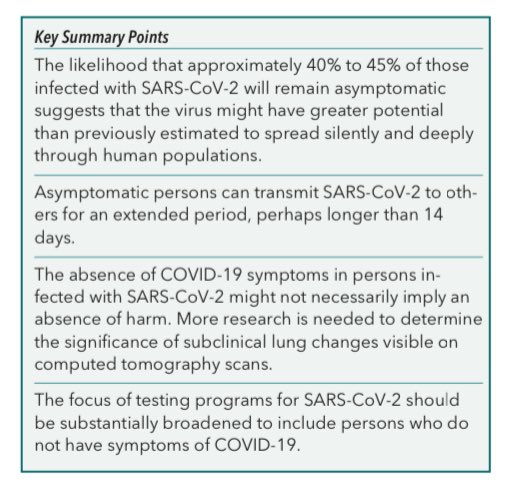
2/ 4-months after #COVID, this @JAMA_current study found 51% of N=478 pts had >=1 #LongCOVID symptom that wasn’t there before. 63% of those w CT scans had lung problems, with 1 in 5 showing scarring. What else?...
bit.ly/34a29k9
bit.ly/34a29k9

3/ This JAMA study also showed this important array of symptoms that essentially constitute #LongCOVID – 31% gross fatigue, 21% cognitive problems, and 23/18/7% anxiety, depression & PTSD. Their outsides look normal, but they aren’t! 

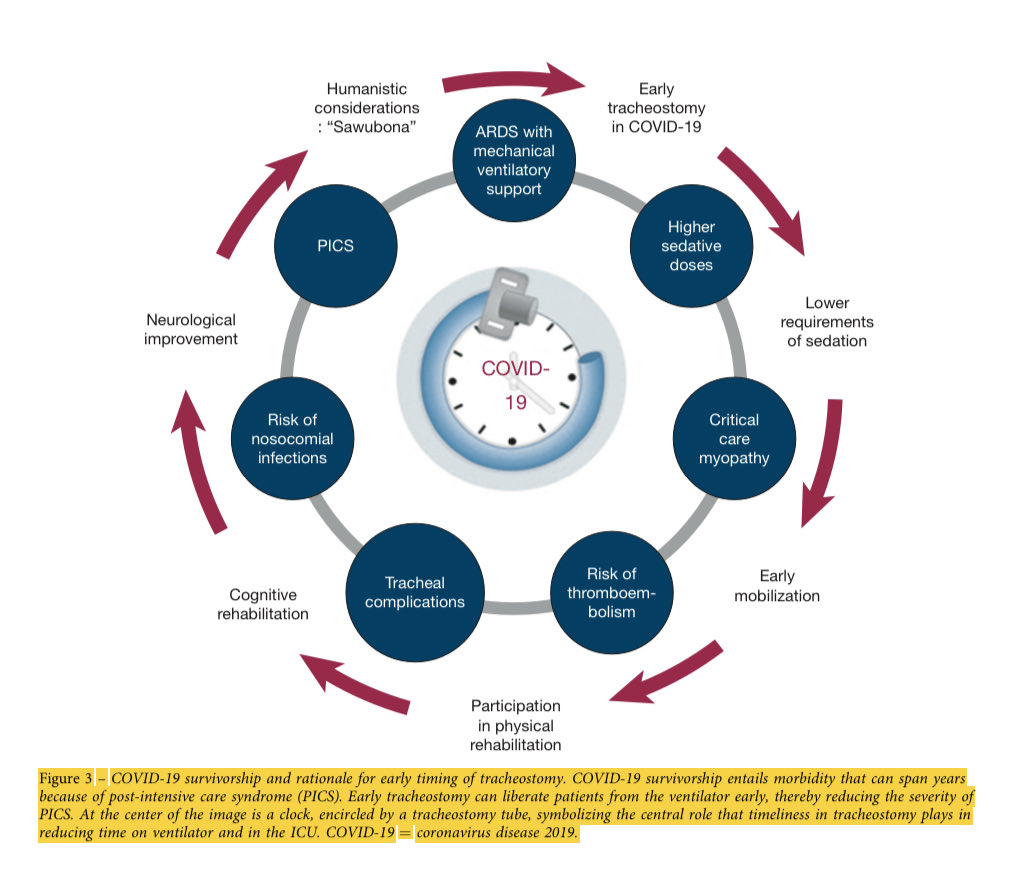
4/ The lung has a limited number of ways to respond to Covid, several of which lead to scarring we call fibrosis. That limits the flexibility of lung tissue. Importantly, it’s not always permanent and you need to be seen early if symptoms are ongoing.
5/ One type of lung scarring that can be melted away nicely with steroids is called cryptogenic organizing pneumonia (COP). The top pictures show “white” (damage) in lungs that turns to “black” (air – bottom pics) after steroids. This is what we want to see. 
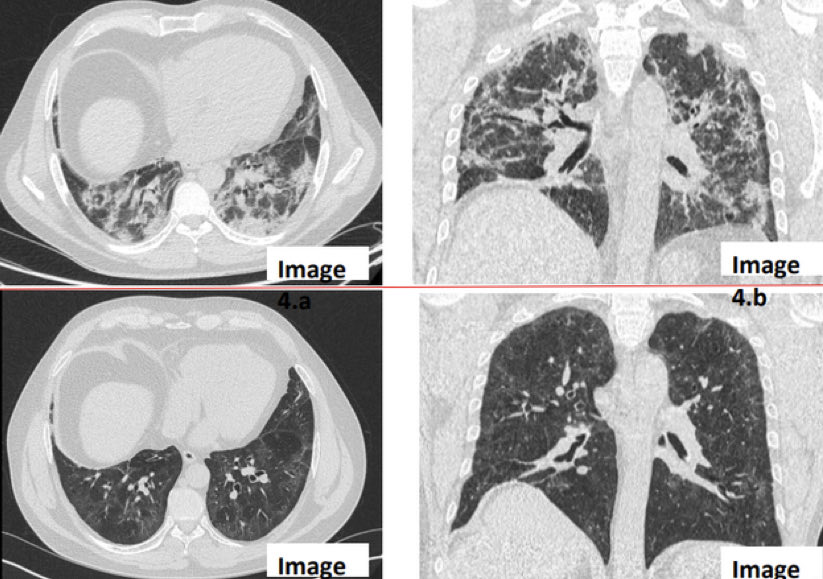
6/ Think of keloid scars. See this tuft of tissue I’ve circled? That’s scarring that is “stuffing itself” into an airway. We want to melt with steroids before it’s too late. 

7/fin
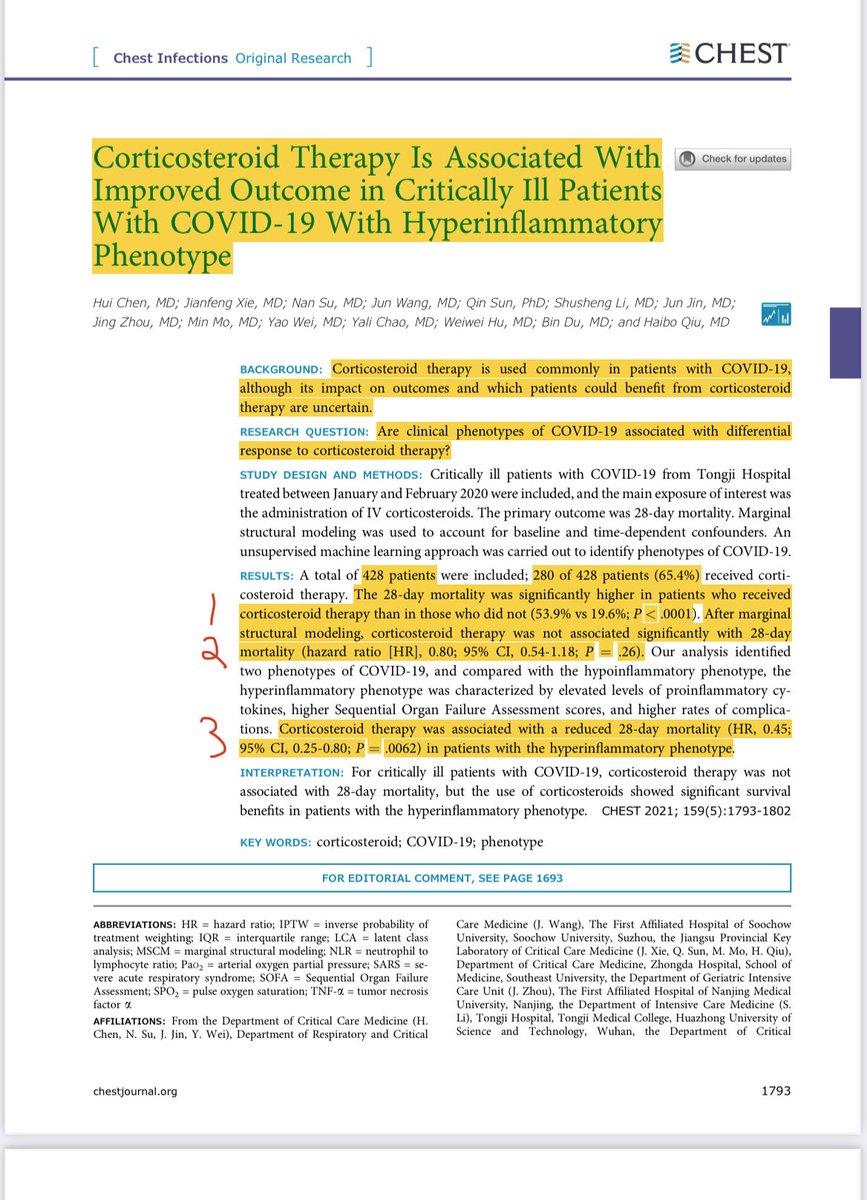
This study of >800 pts found that 40% had #LongCOVID symptoms, of whom 1 in 25 had this “organizing pneumonia” (COP) type of treatable lung scarring. Most got better on steroids (prednisone 0.5 mg/kg) for a month or two. Be sure to ask for help!
bit.ly/349E9h7

This study of >800 pts found that 40% had #LongCOVID symptoms, of whom 1 in 25 had this “organizing pneumonia” (COP) type of treatable lung scarring. Most got better on steroids (prednisone 0.5 mg/kg) for a month or two. Be sure to ask for help!
bit.ly/349E9h7


• • •
Missing some Tweet in this thread? You can try to
force a refresh