Don’t miss a new accredited #tweetorial launching TOMORROW here on @cardiomet_ce. #Emergencymedicine researcher and devotee of deep understanding of drug mechanism of action @md_pollack will be considering why being #nonsteroidal means better #MRA. Don't miss it! @GoggleDocs
@drkevinfernando @kidney_boy @KateIsabelle24 @SantosGallegoMD @aayshacader @VietHeartPA @Lross246 @SeguraCardio @ValleAlfonso @edgarvlermamd @nephondemand @DrRaniKhatib @HanCardiomd @SABOURETCardio @ChristosArgyrop @JavedButler1 @Steph_Achenbach @mvaduganathan #cardiotwitter
1) Welcome to a #tweetorial where we’ll explore the mechanism of action of mineralocorticoid receptor antagonists (#MRA) & consider why it's so #vogue to be #nonsteroidal. This program is accredited for 0.50 credits for #physicians #nurses #pharmacists. I am @md_pollack. #FOAMed 

2) This series is supported by educational grants from AstraZeneca, Bayer, and Chiesi, and is intended for healthcare professionals. Faculty disclosures are listed at cardiometabolic-ce.com/disclosures/ and earlier programs, still available for credit, are at cardiometabolic-ce.com.
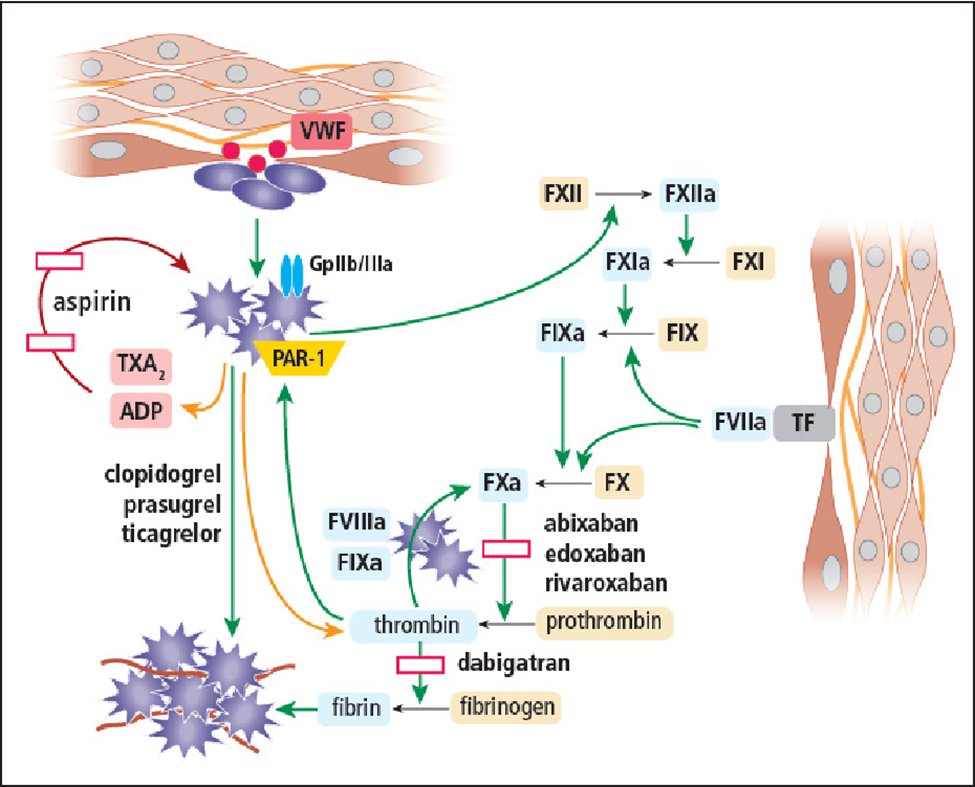
3) #Aldosterone is the primary--tho not the only--endogenous ligand of the mineralocorticoid receptor (MR). #Cortisol is the other. What do they have in common? They are both #steroids. We will focus on aldosterone. Synthesized in the glomerular zone of the adrenal cortex ...
4) ... in response to #hyperkalemia or sodium depletion, aldosterone is the culmination of activation of the renin-angiotensin system. It is key to controlling both #bloodpressure and extracellular volume homeostasis by ⬆️ renal sodium reabsorption & ⬆️potassium excretion.
5) We now know that there is also local aldosterone production in peripheral tissue. Overall aldosterone has protean effects and is therefore an important therapeutic target. See annualreviews.org/doi/10.1146/an…. 

6) The history of recognizing these diverse impacts is nicely recounted by Epstein in 🔓karger.com/Article/FullTe…. In its "nonepithelial role", aldosterone in promotes inflammation, collagen formation, fibrosis, and necrosis. Chronically elevated aldosterone, especially ...
7) ... coupled with salt loading, promoted cardiac fibrosis. In animals receiving a high salt diet and aldosterone, spironolactone, a steroidal aldosterone receptor blocker, appeared to protect against development of cardiac fibrosis, all suggesting that cardiac fibrosis ...
8) ... might be mediated by MR activity. Similarly, data suggests that blockade of the MR receptor might slow progression of #CKD because its activation by aldosterone promote inflammations and fibrosis and manifests as proteinuria and nephrosclerosis.
9) Hence the #cardiometabolic organ cross-talk effects discussed by @md_pollack (and still available for free CE/#CME at cardiometabolic-ce.com/cardiorenal9/) . . . #Spironolactone & #eplerenone, the approved steroidal MRAs often viewed as "kidney drugs," reduce both ...
10) ... mortality and hospitalization when treating #heartfailure. For example, #HFrEF guidelines from @ACCinTouch updated this year state that "aldosterone antagonists are added in as part of the therapy for patients with symptomatic chronic HFrEF who are already receiving ...
11) ... beta-blockers and an ARNI/ACEI/ARB and who do not have contraindications ... The doses of aldosterone antagonists used in clinical trials, which are typically below those that might influence blood pressure, are sufficient for clinical efficacy." (jacc.org/doi/10.1016/j.…)
12) And also in 2021, new @escardio #HF guidelines state, "MRAs (spironolactone or eplerenone) are recommended, in addition to an ACE-I &a beta-blocker, in all patients with #HFrEF to reduce mortality and the risk of HF hospitalization. They also improve symptoms.
13) MRAs block receptors that bind aldosterone and, with different degrees of affinity, other steroid hormones (e.g. corticosteroid and androgen) receptors. Eplerenone is more specific for aldosterone blockade and, therefore, causes less gynaecomastia." (academic.oup.com/eurheartj/arti…
14) How does this happen? Again, it's a steroid effect and it's off target when one thinks of aldosterone simply ⬆️potassium retention. Spironolactone induces gynecomastia by decreasing testosterone production, by ...
15) ... increasing peripheral conversion of testosterone to estradiol, and displacing estradiol from sex hormone-binding globulin (ncbi.nlm.nih.gov/pmc/articles/P…)
16) And aye, there's the rub. The problem with steroidal MRAs? Side-effects! Primary? #hyperkalemia Others? #gynecomastia #erectiledysfunction #menstruation irregularities. BTW, "aye there's the rub" were #Hamlet's words when he discovered #uremic #pericarditis. 

17) We'll consider those further tomorrow and then start to discuss the nonsteroidal approach. Meanwhile, here's a recap question: Which of the following might blocking aldosterone NOT impact?
18) Return tomorrow and check your answer, then buckle up for more learning. @MedTweetorials @goKDIGO @DLBHATTMD @CMichaelGibson @cpcannon @gcfmd @hvanspall @ShelleyZieroth @renaltubules @DrMarthaGulati @JonathanNefro @edurontoFF
19) Welcome back! We are talking #MRA therapy and the difference between #steroidal and #nonsteroidal therapy on your ONLY source for CE/#CME-accredited, serialized education on Twitter! FOLLOW US for FREE credit by expert authors. I am @md_pollack.
20) Yesterday's poll? All but an effect on cardiac conduction. Per @AgarwalRajivMD (academic.oup.com/eurheartj/arti…), the MR has the same binding affinity for aldosterone and cortisol, & mediates fluid, electrolyte, & hemodynamic homeostasis, as well as tissue repair.
21) Blockade of the MR with spironolactone in pts w/HFrEF (RALES; N = 1663) yielded 30% ⬇️ risk of death vs placebo (doi: 10.1056/NEJM199909023411001); the trial was stopped prematurely for efficacy, including ⬇️progressive #heartfailure ⬇️sudden death & ⬇️hosp for heart failure. 

22) These data still carry into contemporary guidelines as cited above. Limitations were ⬆️rates of breast pain & gynecomastia & risk of #hyperkalemia. In fact, a 2004 pharmacoepidemiological study showed . . .
23) . . . ⬆️incidence of hyperkalemia after RALES pub, which also correlated with ⬆️ Rx of spironolactone (doi: 10.1056/NEJMp048144). The other available #steroidal #MRA, #epleronone, binds more specifically than #spironolactone to the MR, and so has similar renal effects on ...
24) ... sodium and importantly potassium, but has fewer progestational and antiandrogenic adverse effects and therefore less painful breast/#gynecomastia risk. The risk of #hyperkalemia however remains a significant limitation of #MRA use and has been shown to limit . . .
25) . . . guidelines-recommended tx in pts with #heartfailure and #CKD. New generation potassium binders #SZC and #patiromer can safely reduce hyperkalemia risk and facilitate #MRA and #RAASi therapy. Go to cardiometabolic-ce.com/category/hyper… to learn more & earn even more FREE CE/#CME!
26) But could there be a way to provide a therapeutic MR blockade without the baggage of a steroid? No off-target antiandrogen effects and maybe less hyperkalemia? Enter the #nonsteroidal MRAs! Recently approved 🇺🇸🇪🇺, #finerenone is a novel, selective, nonsteroidal MRA.
27) You can check it out and earn CE/#CME credit at cardiometabolic-ce.com/cardiorenal5/. It holds particular promise for cardiorenal protection overall and particularly in #DKD. So how are #nonsteroidal #MRAs different? Several ways, starting with how they interact with the MR.
28) Finerenone blocks the MR as a bulky, passive antagonist, is more selective than spironolactone, & is at least as potent. Again per @AgarwalRajivMD, finerenone's physicochemical properties--lipophilicity & polarity--determine tissue penetration & distribution, allowing ...
29) ... a novel MRA pharmacology w/pronounced anti-fibrotic efficacy in animal models. Compared with other MRAs, finerenone has differential downstream effects on MR blockade. 
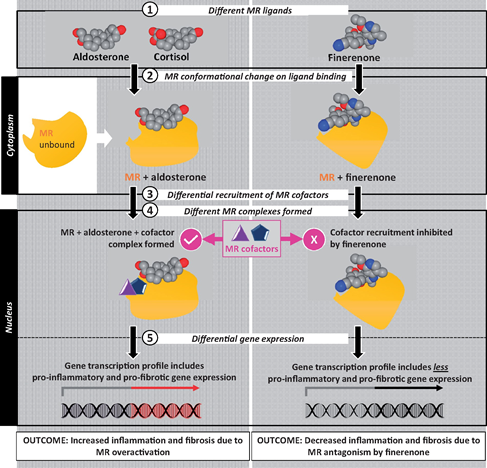
30) Other differences include a more balanced kidneys-heart distribution for finerenone, improved #pharmacokinetics that may ⬇️hyperkalemia, and thru various mechanisms finerenone likely offers greater protection from cardiac & renal injury/remodelling & stronger inhibition . . .
31) ... of renal expression of pro-inflammatory and pro-fibrotic markers. So, a quiz:
Which of the following is true about finerenone compared to spironolactone & eplerenone?
Which of the following is true about finerenone compared to spironolactone & eplerenone?
32) Mark your response and return tomorrow for the answer, a wrap-up of this program, and your link to FREE CE/#CME--#physicians #nurses #Pharmacists #PAs #NPs. Nod to @GoggleDocs @CardioNerds @DrRaniKhatib @Drroxmehran @BiykemB @Steph_Achenbach @KateIsabelle24 @HanCardiomd
33) Welcome back! I am @md_pollack & you are just a few clicks away from FREE CE/#CME for following along this #tweetorial on NONsteroidal #MRAs! Did you even know that #spironolactone is steroidal?? That's where the #gynecomastia and much of the #hyperkalemia comes from.
34) So yesterday we were talking about finerenone, the prototypical nonsteroidal #MRA. The poll? #Finerenone has a short half-life. It inhibits cardiorenal fibrosis and it isn't a great #antihypertensive. There have been lots of new data coming out in 2021.
35) Finerenone's approval by the @US_FDA is for reduction in the risk of kidney function decline, kidney failure, CV death, non-fatal heart attacks & hospitalization for heart failure in adults living with CKD associated with T2D.
36) Approval was largely on the basis of FIDELIO-DKD which had 1º renal & 2º CV endpoints. It explored the use of finerenone in people with CKD stage 3 or 4 & severely elevated albuminuria & T2D. (Thanks, @GoggleDocs) 

37) Then FIGARO-DKD explored the impact of finerenone in people with T2D & a wider range of CKD. In contrast to FIDELIO-DKD, FIGARO-DKD had 1º CV & 2º renal endpoints but less advanced CKD Nearly half had microalbuminuria and the mean eGFR was 68ml/min Mean follow-up was 3.4yrs. 

38) So, who was studied?
✅7437 participants T2D & CKD
✅ACR 30-300mg/g (microalbuminuria) & eGFR 25-90ml/min (CKD 2-4)
✅ACE 300-5000 (macroalbuminuria) & eGFR at least 60ml/min (CKD stage 1-2), a group not extensively studied in the past
✅ Max tolerated #RAAS inhibitor
✅7437 participants T2D & CKD
✅ACR 30-300mg/g (microalbuminuria) & eGFR 25-90ml/min (CKD 2-4)
✅ACE 300-5000 (macroalbuminuria) & eGFR at least 60ml/min (CKD stage 1-2), a group not extensively studied in the past
✅ Max tolerated #RAAS inhibitor
39) Individuals had to have a K ≤4.8mmol/l at screening Mean HbA1c 7.7% Mean SBP 136mmHg. Of note, there was 8.4% background SGLT2 inhibitor use & 7.5% background GLP-1 receptor agonist use. These agents have been recommended to reduce cardiorenal risk in many guidelines for T2D 

40) Individuals like those recruited to FIDELIO-DKD i.e., advanced #CKD were excluded from FIGARO-DKD Additionally, individuals with symptomatic #HFrEF were also excluded as MRAs are a key pillar of HFrEF management with prognostic and symptomatic benefit. 

41) The 1º endpoint of FIGARO-DKD was a composite of death from CV causes, nonfatal MI, nonfatal stroke, or hospitalization for HF (HHF)
The key 2º endpoint was a composite of kidney failure, a sustained decrease from baseline of at least 40% in the eGFR, or renal death
The key 2º endpoint was a composite of kidney failure, a sustained decrease from baseline of at least 40% in the eGFR, or renal death
42) The 1º composite endpoint was significantly ⬇️by 13% (ARR 1.8%) mainly driven by a 29% RRR in HHF. Other components of 1º endpoint were not significantly reduced. CV benefits were seen in all categories of UACR & eGFR. Benefits were also independent of SGLT2i & GLP1RA use. 

43) The 2º composite renal outcome was numerically lower but did not reach statistical significance. There was no significant difference in adverse events (including #AKI & gynecomastia) between groups.
44) Incidence of #hyperkalemia-related discontinuation was not high, but was ⬆️ with finerenone (1.2%) compared w/placebo (0.4%). This is less than the expected hyperK+ with steroidal MRAs in a similar population.
45) One of the main limitations of FIGARO-DKD was that only around 3.5% of trial participants were of Black ethnic origin. It is well established that individuals of a Black ethnic background are at increased risk of developing end-stage renal disease.
46) FIDELIO-DKD was published in nejm.org/doi/full/10.10…. FIDELITY, a pre-specified meta-analysis of individual pt data from FIDELIO-DKD & FIGARO-DKD, was presented at the virtual #ESCCongress2021. Again cited @AgarwalRajivMD discusses FIDELITY here: ajmc.com/view/results-f…
47) FIDELITY showed that finerenone significantly ⬇️ the risk of a composite CV outcome (time to CV death, nonfatal MI, nonfatal stroke or HHF) by 14%, and also sig ⬇️risk of a composite renal outcome (≥57% decline eGFR, time to kidney failure or renal death) by 23%. 

48) Such data clearly suggest that a nonsteroidal #MRA has benefits, especially in patients with CKD/DKD who might benefit from aldosterone inhibition but are at particularly high risk for hyperkalemia. Data on combo finerenone and #SGLT2i are eagerly awaited in such pts.
49) That's it! You made it! Claim your 0.5h CE/#CME at cardiometabolic-ce.com/cardiorenal13/ now, and then FOLLOW US for more of the ONLY accredited serialized #tweetorials in #cardiometabolic medicine! I am @md_pollack. Also JOIN US at @ckd_ce for more credit focused on--you guessed it--#CKD!
• • •
Missing some Tweet in this thread? You can try to
force a refresh