Case: A gentleman is brought to the ER after being found down. He was reportedly walking around a Target parking lot without clothes on just before collapsing. He has no ID.
What else do you want to know?
So this is a tough one for multiple reasons.
HPI: Patient responds with "Martha" to every question you ask, including asking about his name.
As a result, PMH, PSH, Social hx, Allergies, Family history are all unknown.
He has no ID, no collateral available.
Exam:
Vitals = T 103*F, BP 120/80, HR 115, RR 23, SpO2 99%
General: disheveled, constantly in motion (fidgety) but not agitated, age mid-30s?
HEENT: pupils large, equal, but sluggishly reactive to light, mucous membranes dry
Cards: RRR, tachycardic, no mrg
Exam cont'd:
Pulm: CTAB
Abd: soft, nontender, nondistended
Skin: no rashes, no track marks, no tattoos, mud on legs
Neuro: MAE spontaneously but limited by coopeation, CN's seem normal?
Psych: perseverates on Martha
He appears well, for the most part...
HEY, you hear a nurse yell at you, HE's IN VTACH! The nurse points at the monitor, and he is indeed in a wide complex tachycardia with rate 160. It doesn't look like torsades. He's still alert and his BP is 100/70. You converts out of it before you do anything
Now what? I'll assume you want BMP, CBC, UDS, EKG, maybe a blood gas. Anything else?
Do you want to do anything in the meantime while these are in the lab.
Looping in the participants so far @rloganjonesmd @fernandbteich @Ndouthit @speak_of_diablo
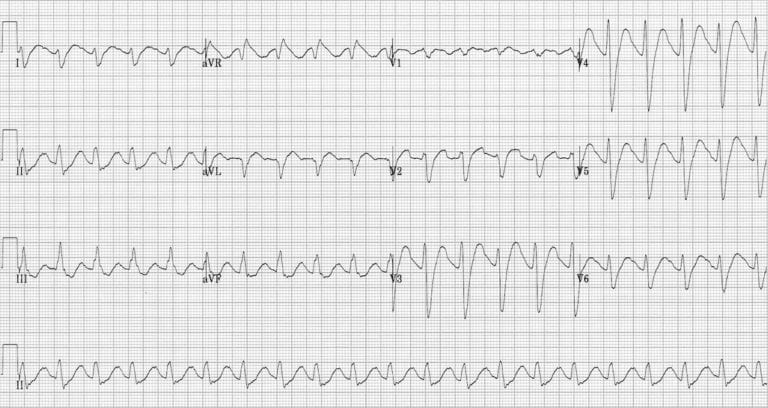
EKG shows: QRS 150, sinus tachycardia --> Patient started on Sodium Bicarb gtt. Thiamine given empirically
UDS is pending... Other labs as follows:
Na 130, K 4, Cl 100, HCO3 20, BUN 35, Cr 1.0, Gluc 100
WBC 7, Hb 15, Plt 190
LFTs normal, INR 1.3
It sounds like the main ddx is toxodromic, focusing on anticholinergic given his confusion, fevers, and pupils. Particular concern for TCA given the rhythm issues.
Any other thoughts before the UDS hits? Hey @ToxAndHound, any pearls you can throw our way?
Great work everyone! The UDS comes back --> amitriptyline, diphenhydramine, nicotine with negative ASA/APAP. Serum ethanol positive (don't have value).
The patient got initial bicarb boluses with decreases in QRS, but needed a drip therapy b/c the QRS widened
For those of you who haven't seen one before, check out this article on LITFL about TCA toxicity. The keys are the wide QRS >100 ms and the slurred S-R' pattern in lead AVR (among other findings). #MedEd #FOAMed
litfl.com/tricyclic-over…
The case concludes with the patient in the ICU for arrhythmia monitoring. His mental status clears; he admits to attempting overdose by taking a handful of his amitriptyline and diphenhydramine.
You all zeroed in on anti-ACh tox, but let's talk "found down"
Patients who are "found down" (Fahn Dahn in Pittsburghese) can be perplexing. Little history, confusing picture.
In the words of our Chair of Medicine here at @PittDeptofMed "Don't fall into the booby traps of patients found down!"
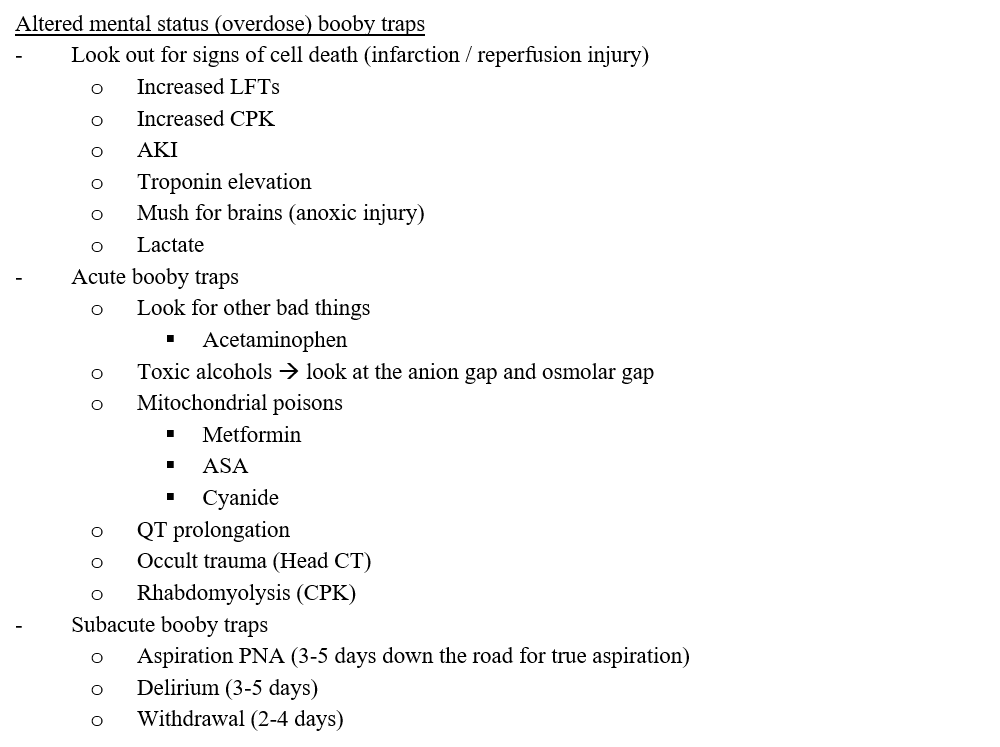
Acute booby traps (dead and dying tissue) --> kills patient quickly
-look for CPK, LFT, Tn elevation, AKI, lactate
-make sure their brain works
-check for poisons: UDS, Acetaminophen
-if lactate is out of control, think of mitochondrial poisons: metformin, CN
Subacute Booby Traps --> kills patient after you've stabilized them
> 3-5 days --> aspiration PNA/ARDS, delirium
> 2-4 days --> withdrawal
Make sure you keep these in mind. The patient may not be able to give you a history so you have to speak for them!
Finally: collateral is key. If you can get a history from anyone - EMS, family, neighbor - you can get one step closer to helping your patient out.
Finally finally: we're big on #FOAMed references, so check out @ToxAndHound's podcast on toxidromes. We think you'll find it helpful!
emcrit.org/emcrit/tox-hou…
We hope you liked today's case. Give us your feedback. It helps us make cases better!











